When gastrointestinal (GI) symptoms strike, you may be wondering how to heal your gut. Most strategies involve improving gut-brain communication and supporting the gut microbiome and intestinal barrier. Diet and lifestyle changes with the guidance of an experienced GI care team can help.
When you have a visible wound, like a scraped knee, you typically know what to do (grab the first-aid kit!) to help heal the affected skin. But when gastrointestinal symptoms strike, you can’t see an “owie.” You just know something doesn’t feel right. So, what can you do? If you’re experiencing uncomfortable gastrointestinal (GI) symptoms, such as bloating, abdominal pain, gas, diarrhea, acid reflux, or something else, you may be wondering how to heal your gut.
The best ways to improve your digestive health will depend on your specific symptoms, any underlying conditions, your lifestyle factors, and more. In this article, we’ll explore elements of GI health, factors that affect the GI tract, and what you can do to have your healthiest gut yet.
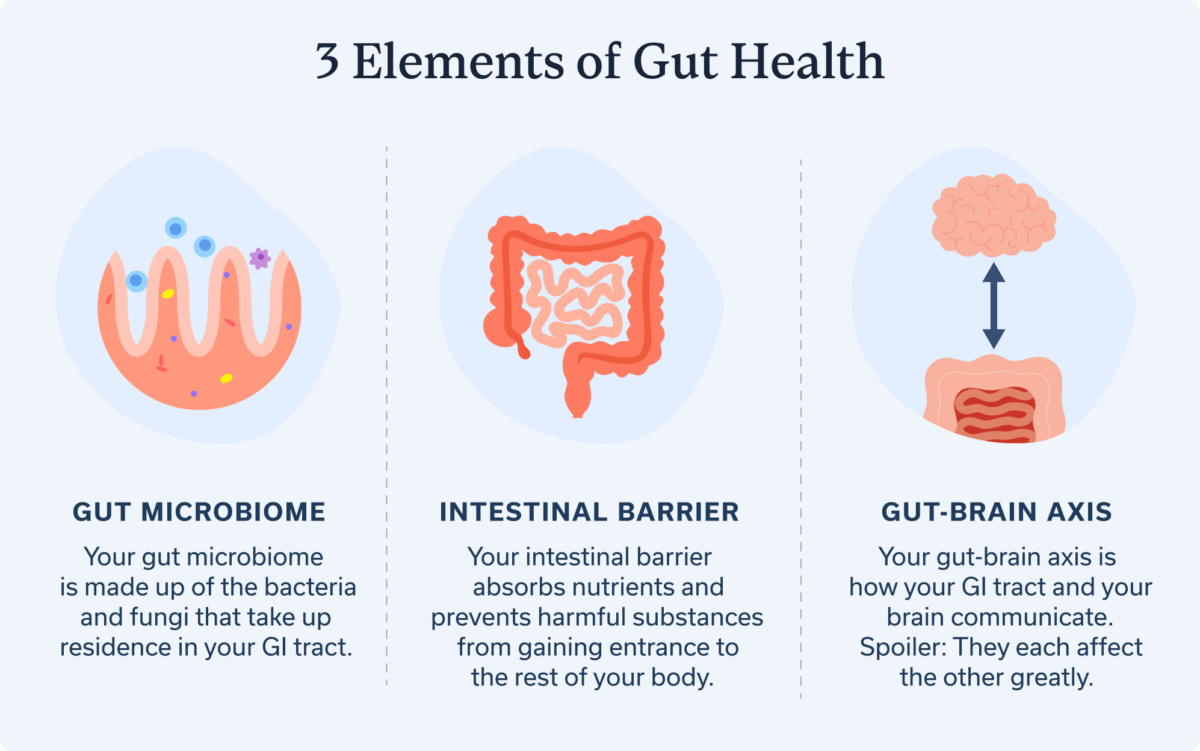
Understanding gut health
“Gut health” can mean many things, and researchers don’t necessarily have a clear definition. In a nutshell, a healthy gut or GI tract will have good communication along the gut-brain axis, a healthy microbiome, and a healthy intestinal barrier.
3 elements of gut health
- Gut-brain axis. Your gut-brain axis is how your GI tract and your brain communicate. This communication occurs through our nervous system. Spoiler: They each affect the other greatly.
- Gut microbiome. Your gut microbiome is made up of the bacteria and fungi that take up residence in your GI tract.
- Intestinal barrier. Your intestinal barrier absorbs nutrients and prevents harmful substances from gaining entrance to the rest of your body. It’s composed of three layers: a mucus layer, an epithelial layer (made up of proteins), and a lamina propria (made up of immune and nerve cells).
Factors affecting gut health
Many factors can affect your GI tract, from your mental health status to your diet to any underlying conditions. Here are few to consider.
Stress, anxiety, and depression
Our brain and GI tract communicate with each other via the gut-brain axis. So when you’re stressed, nervous, or living with anxiety or depression, your GI tract may also respond with symptoms. These symptoms can be caused by miscommunication along the gut-brain axis due to our body’s natural response to stress.
Your GI tract has an extensive network of hundreds of millions of neurons. This network is called your enteric nervous system (ENS); it controls your digestive functions and is one part of your larger autonomic nervous system (ANS). Overall, the ANS controls the involuntary responses in your body, not just digestion. Other divisions of the ANS include your parasympathetic nervous system (PNS) (aka your “rest and digest” mode) and sympathetic nervous system (SNS) (aka your “fight, flight, or freeze” mode).
When anxiety or stress strike, sometimes the brain seems to tell the ENS to press pause on what’s going on with your GI tract, which can lead to symptoms. Miscommunication along the gut-brain axis can also cause issues with motility, which means the movement of food and waste through the GI tract. Miscommunication can also lead to visceral hypersensitivity, when our internal organs cause us pain just from doing their everyday jobs.
Inadequate sleep
A lack of quality sleep can affect your GI tract health in many ways. Researchers are still trying to learn all the ways this happens, but one thing we know is that sleep disturbances can exacerbate stress, which then can lead to issues with gut-brain axis communication. Sleep is also an important period of “rest and digest” time. So, when sleep suffers, often our digestion suffers as well. Through both human and animal studies, researchers have gleaned that sleep deprivation may also negatively affect the gut microbiome.
Poor diet or food intolerances
No surprise here: What we put in our bodies also has an impact on our GI tract health. Consider ultra-processed foods, which are often loaded with additives that are linked to increases in inflammatory bowel disease (IBD) colorectal cancer, and potentially even irritable bowel syndrome (IBS). Overconsuming sugar, also found in ultra-processed foods, can damage the intestinal barrier and cause disruptions to the gut microbiome. Food intolerances—like lactose intolerance, histamine intolerance, intolerance to certain carbohydrates, and more—can also affect your GI health.
Underlying conditions
If you’re experiencing a flare-up of an underlying GI condition, such as ulcerative colitis or Crohn’s disease (both of which are types of IBD), your GI tract is likely inflamed. This inflammation can lead to a host of symptoms related to your condition, and addressing it will be crucial in improving your gut health.
Healing the gut
Now that you have a better understanding of what GI health is and the many factors that can affect it, you may be curious whether you can heal your gut—and how to do it fast. Improving GI health, however, isn’t as simple as applying a salve and slapping on a bandage—and it’s never a one-size-fits-all approach. Instead, the steps to improve your gut health should be based on an assessment of your own specific, individual needs.
Working with a knowledgeable GI provider, like those at Oshi Health, is an important place to start. GI providers include gastroenterologists, GI nurse practitioners, GI physician associates (also known as physician assistants), GI registered dietitians, GI psychologists, and more.
Our Providers
Meet the GI experts at Oshi Health
Oshi brings medical, dietary, and gut-brain treatments together under one virtual roof—all provided by leading GI specialists who are experts in their fields.
Once they understand your symptoms, underlying conditions, medications or supplements, and lifestyle factors, they can help recommend the best steps to improve your gut health. Your care plan may include plenty of different strategies, including the following:
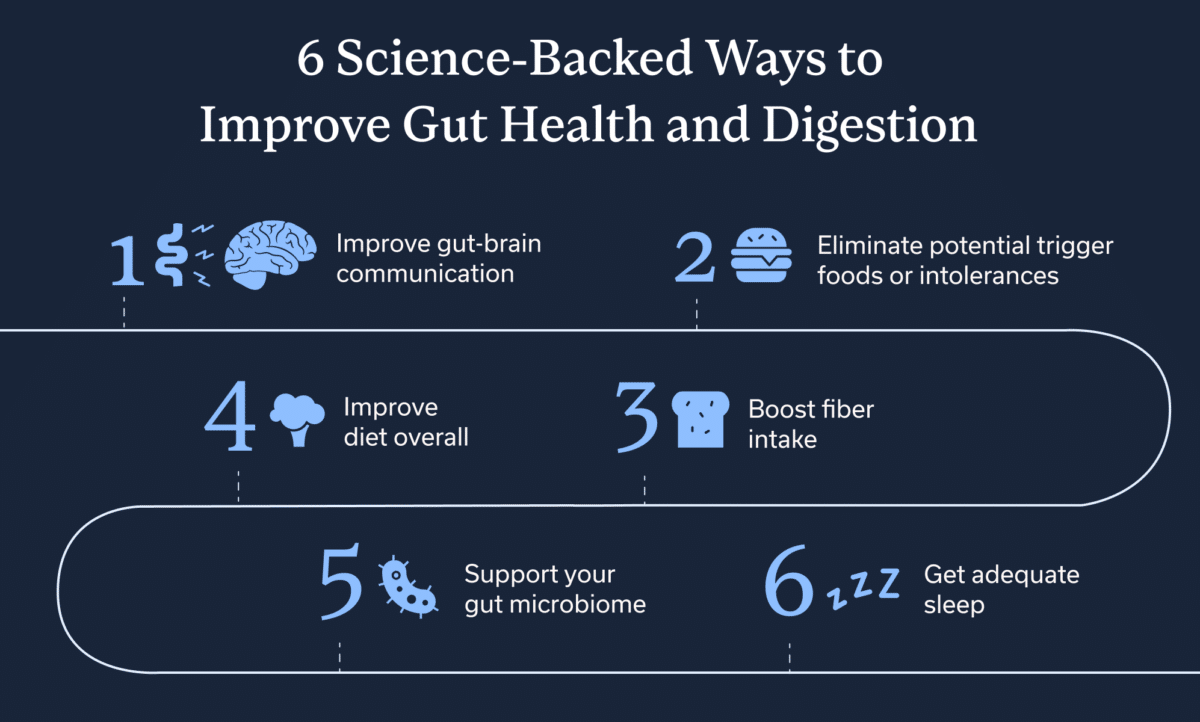
1. Improve gut-brain communication
If your GI provider determines that you are experiencing gut-brain communication disruption, they can help you develop strategies to improve communication along this important axis. Strategies may include cognitive behavioral therapy (CBT), diaphragmatic breathwork, mindfulness and stress reduction techniques, guided meditation, and gut-directed hypnotherapy.
2. Eliminate potential trigger foods or intolerances
Poor diet can worsen your gut health, but you can change your diet to have a positive impact on it instead. You should make any dietary changes for gut health with the help of a knowledgeable GI registered dietitian.
The goal should always be to ensure you can eat as wide a variety of foods as possible, including those that are important to your culture. However, sometimes a temporary elimination diet may be necessary to determine if you have food intolerances and how to address them. After eliminating foods that are common culprits of GI symptoms, your GI registered dietitian will help you carefully add them back, one at a time.
3. Improve diet overall
Ultra-processed foods are often super tasty because they are engineered to be that way. But they are loaded with sugar, sodium, and potentially harmful additives that can disrupt your gut microbiome and gut barrier. While treating yourself to a candy bar or bag of chips every now and then likely isn’t an issue, overconsumption of “junk foods” can harm gut health. Stick to whole foods as much as possible, and reduce consumption of added sugar.
4. Boost fiber intake
In general, fiber consumption is a great way to support gut health, as long as increased fiber isn’t a trigger for you. Working with a GI expert can help you determine the amount of fiber that’s best for your gut and what sources help keep symptoms at bay. Fiber does a few things. It can help bulk your stool to *ahem* keep things moving and it supports your gut microbiome, as noted below. Remember to drink plenty of water to support any increased intake. Hydration in general is also a plus for your GI tract.
5. Support your gut microbiome
Some dietary changes may also help with supporting your intestinal barrier. For example, when your gut microbiome ferments the dietary fiber you consume, it produces something called short-chain fatty acids (SCFAs). SCFAs support your intestinal barrier health and your immune system. Adding more fiber, under the guidance of a GI registered dietitian, may be beneficial in some cases. You can support your microbiome by getting plenty of fiber from a rainbow of fruits and veggies.
6. Get adequate sleep
Your sleep quality and quantity also inform gut health. We all know that sleep is good for us so that we’re on top of our game the next day. But sleep, or a lack of quality slumber, can also affect your GI tract. Improving sleep quality will positively impact the gut. Aim for at least seven to nine hours of uninterrupted sleep per night. Obviously, some interruptions may be unavoidable. I’ve yet to sleep through a night without having to pee, for example. The point is to try to reduce interruptions from light or sound pollution as much as possible.
Maintaining a healthy gut
Once you’ve worked with a GI provider to help improve your gut health based on your unique needs, you may experience symptom improvement rather quickly, or slowly over time. If you notice that your symptoms return or later worsen, then a reevaluation and new strategies may be necessary. Keeping a symptom diary can be helpful so that you can gauge when your GI health is changing.
Key Takeaways
- If you’re experiencing GI symptoms, you may be looking for ways to heal your gut.
- The strategies that best support your gut health will depend on your unique situation.
- Factors such as your mental health, lifestyle, diet, and underlying conditions can all affect your GI health. And GI health is a journey; it can change, and change again. You might feel symptom-free one week and then have symptoms the next.
- Working with a knowledgeable GI provider, such as those at Oshi Health, can help you have more symptom-free days and better gut health overall. Reach out for a consultation.
FAQ
-
The best strategies for improving your gut health will depend on your unique symptoms and other lifestyle factors. If you are experiencing GI symptoms, talk to a knowledgeable GI provider.
-
How long it takes to improve your GI health will depend on various factors, including your symptoms, underlying conditions, food intolerances, and more.
-
The foods that will best support your gut health will be different from the next person’s and will depend on any food intolerances you may have. Consult with a knowledgeable GI provider to find out what’s right for you.
Oshi is your partner in digestive health
Feel like your digestive concerns are running your life? You’re not alone—and we’re here to help you find lasting relief.
Oshi Health GI providers, gut-brain specialists, and registered dietitians work together to address your symptoms and find solutions that actually work for you.
Whether you’re dealing with chronic digestive issues or unpredictable symptom flare-ups, our GI specialists deliver:
✔ Personalized care plans tailored to your lifestyle
✔ Science-backed strategies to calm your gut
✔ Compassionate, whole-person care
✔ And so much more!
Ready to take control of your gut health?