If you’re experiencing gastrointestinal symptoms, they’ll hopefully be short-lived. But if they continue to plague you, the symptoms could be early signs that a gastrointestinal (GI) disease is brewing. If you have unexplained GI issues that don’t resolve, talk to an expert GI provider—they’ll help you understand what’s going on, manage symptoms, and if needed, diagnose and treat or slow disease progression.
Many of us have probably experienced this exact moment: You’re enduring gastrointestinal (GI) symptoms, such as bloating and a stomach ache, and you ask yourself, Is something wrong here? You contemplate whether the symptoms are just temporary or are early signs of a more serious gastrointestinal disease. Should you see a clinician, ride it out, call your psychic? (Just kidding on that last one.)
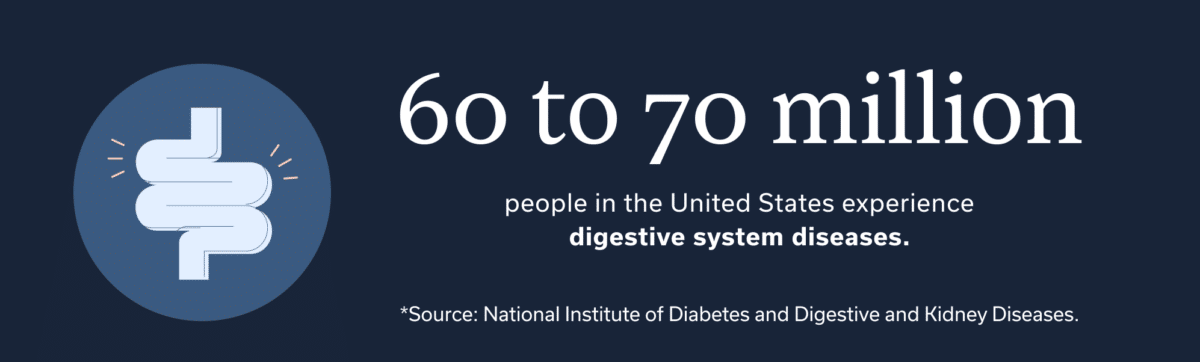
About 60 to 70 million people in the United States experience digestive system diseases in their lifetime. And about 60% of people experience gastrointestinal symptoms each week. Yet only 25% of these people receive a proper diagnosis.
Of course you don’t want anyone else to have to deal with your same pesky symptoms, but knowing that other people have a similar problem can help you feel less alone when you’re clutching your stomach and cursing the red sauce on the pizza you just ate. (Spoiler alert: That pizza may not be to blame for your stomach issues.)
In this article, we explore the different types of GI disease, their early signs and potential symptoms, and what to do to feel better in the long term.
Understanding gastrointestinal disease
It can happen to any of us: Your digestive tract signals its occasional displeasure about something in the form of a random symptom, such as diarrhea, heartburn, or nausea. You’d be hard pressed to find someone who hasn’t experienced at least some type of GI discomfort in their life. If there is such a club of people, sign us up for a membership.
While the occasional but fleeting symptom is common, ongoing GI issues, or ones that frequently come and go, can serve as a clue that something a bit more serious might be up.
If you feel like your GI tract is sending you a near-constant stream of sad-face emojis, talking to a GI provider is a good idea. GI providers can include gastroenterologists, GI physician associates (also called physician assistants), GI nurse practitioners, GI registered dietitians, and GI psychologists—or a combination of any of the above. After all, teamwork makes the dreamwork, right? Together, a team of GI experts can get you back to feeling better.
GI-TRAINED, EXPERIENCED, AND LICENSED
An integrated team of GI specialists
Our expert gastroenterologists, GI providers, registered dietitians, and gut-brain specialists are leaders in their fields, with advanced education and training in gastroenterology. Our comprehensive team approach is personalized to meet your unique needs and address the root cause of your symptoms.
Common types of gastrointestinal disease
GI diseases huddle under two umbrella terms: functional GI diseases and structural GI diseases. Both involve issues with motility, which is the movement of food and waste through your GI tract. But the key difference is that tests do not reveal a physical issue in functional diseases. Instead, test results appear “normal” because you don’t have structural damage. But that doesn’t mean the symptoms are “all in your head.” Your symptoms are very real—don’t let anyone tell you otherwise!
Think of functional GI diseases like this: You’re home alone and you definitely hear a noise, but you can’t find what’s causing it. (You can’t even blame the cat.) In this way, functional GI diseases can present you with a mystery, and a GI provider can be a trusty detective to put on the case.
Functional GI disorders and diseases.
If you have one of these, your GI tract likely looks normal according to testing but motility symptoms occur. These symptoms can include the following:
- Belching disorders, or unexplained, frequent burping
- Centrally mediated abdominal pain syndrome (CAPS), regular abdominal pain that affects your quality of life
- Fecal anorectal pain, aka an unexplained ache or severe pain in your rectum
- Functional defecation disorders, a miscoordination between your abdominal, rectal, and anal muscles (when pooping) causes you chronic constipation
- Fecal incontinence, aka an unexplained inability to prevent the passage of poop
- Functional abdominal bloating or distension, or unexplained frequent feelings of fullness, bloating, or abdominal expansion
- Functional constipation, experiencing regular and unexplained pain or difficulty with going poo—or feeling as if you haven’t emptied your bowels completely
- Functional diarrhea, aka regular and unexplained loose or watery stool but without pain
- Functional dysphagia, or unexplained difficulty swallowing
- Functional dyspepsia, or pain in the upper abdomen
- Functional heartburn, experiencing an ongoing burning sensation in your chest, esophagus, or throat that doesn’t have a structural explanation
- Functional pancreatic SO disorder, when the sphincter of Oddi (which allows bile and pancreatic juice to flow into your small intestine) doesn’t relax properly, leading to the backup of juices, and causing you abdominal pain
- Functional nausea and vomiting disorders, or unexplained nausea or vomiting
- Globus, aka the sensation of a lump in your throat
- Irritable bowel syndrome (IBS), an umbrella term for bowel disorders featuring abdominal discomfort when pooping and changes in pooping habits
- Rumination syndrome, unexplained regurgitation of food
- Unspecified functional bowel disorder, meaning your symptoms are hard to pin down, but something is definitely going on.
Structural GI disorders and diseases.
If you have one or more of these, your tests likely show an abnormality with the GI tract and motility symptoms will also occur. These can include the following:
- Colon polyps, or small clumps of benign or cancerous cells that form on the colon lining
- Chronic pancreatitis, or persistent inflammation of the pancreas from digestive enzymes that get trapped there and cause damage
- Diverticular disease, aka diverticulosis, occurs when the GI tract develops small pouches. (Close to 80% of people develop this symptom by age 80. Diverticulitis is when stool particles get stuck in the pockets and you develop an infection, which is often painful.)
- Fistula, or a small tunnel that develops from the intestinal tract to another part of the intestines, outside the anus or to another organ, such as the bladder of vagina
- Gastroesophageal reflux disease (GERD), when the valve that separates your esophagus from your stomach malfunctions and your stomach contents can backflow into the esophagus, leading to symptoms and damage
- Hemorrhoids, or swollen veins in the rectum or inside or outside the anus
- Hepatitis, an inflammation of the liver from viruses, medications, alcohol, or increased fat deposition
- Inflammatory bowel diseases (IBD), an umbrella term for chronic diseases causing inflammation of the GI tract. (The two most common include Crohn’s disease and ulcerative colitis.)
- Neoplasms (tumors), aka abnormal or fast-growing tissue
- Peptic ulcer disease, aka when you experience gastric ulcers (open sores on the inside of the stomach), and duodenal ulcers (these occur inside the upper small intestine)
Early signs of gastrointestinal disease
Sometimes symptoms are a warning sign that you may have a GI condition. But that’s not always the case. Just because you have an ongoing symptom that seems to match up to a disease doesn’t mean you have that specific disease or disorder.
If you’ve ever put a jigsaw puzzle together, you know that sometimes the puzzle piece seems like it should fit—it might even almost fit—but it doesn’t. The same concept can apply for GI symptoms. Again, a knowledgeable GI provider can help you solve the puzzle. And getting to the bottom of what’s causing your symptoms can get you on track to managing and treating them.
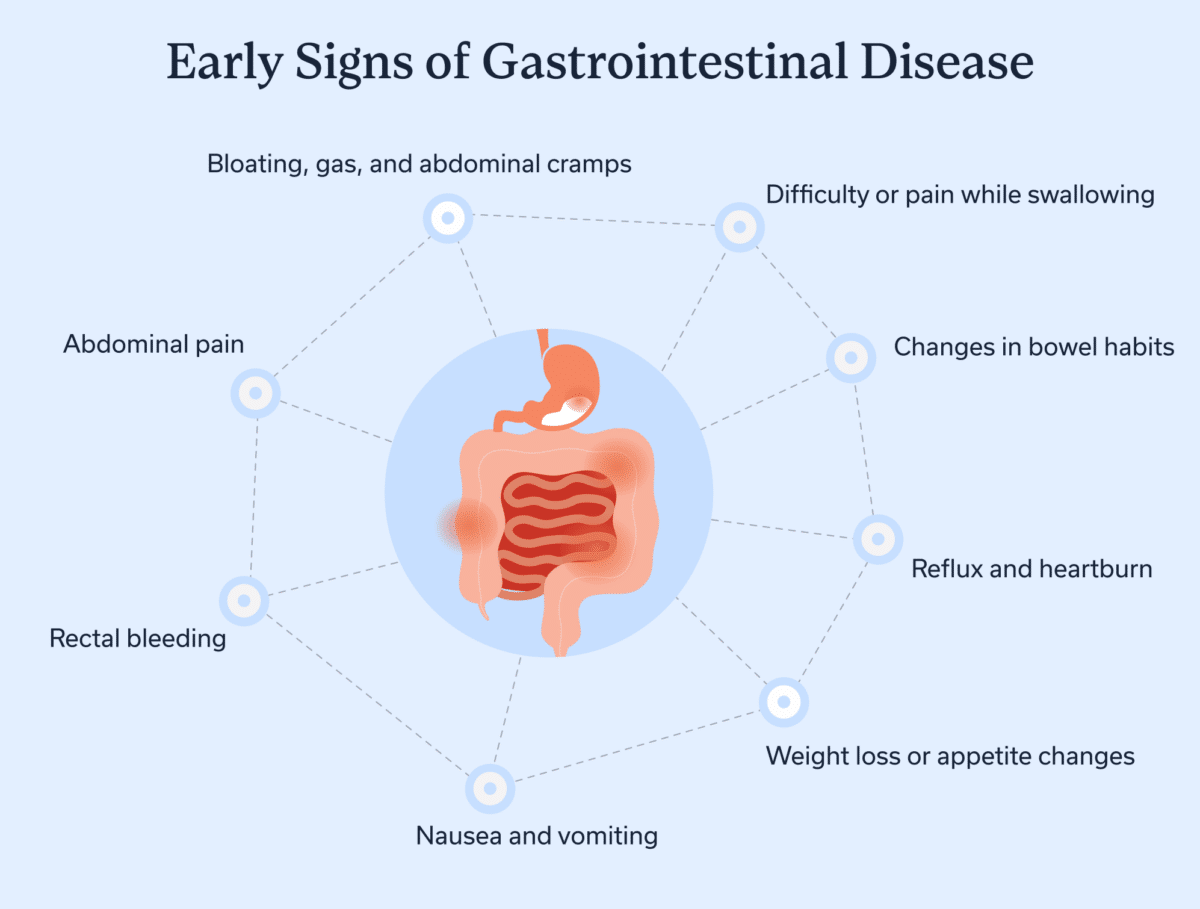
Here are some GI symptoms to consider that may—or may not!—match with a condition.
Abdominal pain
A stomach ache has struck us all at some point. Gas is a common culprit, but stress can also lead to GI upset. If you regularly feel like your abdomen is launching a war within you, you should see an experienced GI provider. Regular abdominal pain can be a sign of an underlying condition, such as IBS.
FYI: Some conditions that affect the reproductive organs can also lead to pelvic pain. These include endometriosis, polycystic ovary syndrome (PCOS), and uterine fibroids. People with these conditions often experience a delay in diagnosis, so knowing about and asking your provider about them when relevant can help.
Changes in bowel habits
Our poop habits (meaning how frequently we need to go) aren’t always the same from day to day, and our poop can look different in shape, size, and color as well. Take a minute to rate your usual poo style using the Bristol Stool Scale. Knowing which type you generally have can be helpful and alert you to any changes.
If you experience constipation or diarrhea or both frequently, especially with discomfort, you should see a GI provider. You may have IBS, which has three forms.
IBS types
- IBS- C: constipation
- IBS-D: diarrhea
- ISBS-M: a mix of constipation and diarrhea
Inflammatory bowel diseases (IBD) can also cause frequent loose or watery stools. With IBD, you may also see blood and mucus in the stool and you may experience weight loss and symptoms in other parts of the body. These conditions warrant guidance from a GI provider.

Difficulty or pain while swallowing
Dysphagia is the term for difficulty (but no pain) while swallowing. And odynophagia refers to pain while swallowing. Several factors, from damaged nerves to a narrowed esophagus, can cause these conditions. They can also be a sign of a tumor, which is why getting checked by a GI provider if you frequently experience difficulty swallowing is crucial.
Bloating, gas, and abdominal cramps
Bloating involves feeling full or having trapped gas in the abdomen, but it can occur with or without your pants feeling too tight. Distension, on the other hand, involves an increase in abdominal size, meaning those trousers might start to feel uncomfortable.
Occasional bloating or distension might occur because you’ve eaten too fast or too much. Hey, it happens: Sometimes we bolt down our lunch before a meeting or can’t resist another helping of Grandma’s lasagna. But if you’re experiencing bloating on the regular, it’s a reason to see a GI provider.
A sensitivity or food intolerance, such as to lactose, is a common culprit. The solution might be as simple as switching what you froth in your morning latte. Or a recent infection could have disrupted your gut microbiome (the bacteria and fungi that live in your GI tract). Some solutions can help balance or support your gut microbiome and reduce or even halt your symptoms.
By the way, endometriosis, PCOS, and uterine fibroids can also cause bloating and GI symptoms in general. A good medical professional will listen to your concerns and evaluate you accordingly, rather than discount your symptoms or brush you off.
Nausea and vomiting
Vomiting has some fun euphemisms (ever heard of “praying to the porcelain gods”?) but it’s a decidedly un-fun thing, as is the nausea that precedes it. Some common causes include a viral infection, food poisoning, or motion sickness.
But ongoing or unexplained nausea or vomiting is a sign to see a GI provider. You may have a dysfunction in the communication between your gut and brain, (yep, they talk to each other via the gut-brain axis), or an underlying condition.
Rectal bleeding
The medical term for fresh or red blood in the stool is hematochezia. Hemorrhoids can cause rectal bleeding, but so can colon cancer. Seeing blood in the stool is always a reason you should talk to a doctor. By the way, black or tarry stools (melena) may be a sign of an upper GI-tract bleed. If you experience this, seek medical attention right away.
Reflux and heartburn
Heartburn or reflux can occur after eating certain foods, like if you’ve ever done a Hot Ones challenge. (Ten out of ten would NOT recommend.) Over-the-counter medications, such as ibuprofen, can also lead to a similar burning feeling. But what if the sensation is a regular thing?
Gastroesophageal reflux disease (GERD) is a more intense and chronic form of reflux. GERD occurs when stomach acid frequently finds its way from your stomach to your esophagus or even your throat, usually from a valve dysfunction. Over time, GERD can damage your GI tract, so if you suspect you’ve got it, talk to a GI provider.
Weight loss or appetite changes
If you’ve ever spent any time with a bathroom scale, you probably know your weight fluctuates a bit day-to-day, based on your hydration status, when and what you last ate, when you last pooped, what you’re wearing, and more.
But if you’re experiencing a surprising change in your appetite or unexplained or unintentional weight loss of more than about 5 pounds, you should see a GI provider. Digestive disorders are a common cause. However, digestive symptoms along with weight loss can also be a sign of several different types of cancer. Other causes of weight or appetite changes include mental health conditions, medication side effects, and more.
Key takeaways
- Some GI symptoms, especially when frequent and unexplained, can be early signs of gastrointestinal disease.
- If you have a symptom that matches up with a GI condition, that doesn’t automatically mean you have that disease or disorder.
- Working with a knowledgeable GI provider can help you get to the bottom of the issue and find the right treatments.
Oshi Health offers a comprehensive and collaborative approach to GI care—with virtual visits available within days.
FAQ
-
Each gastrointestinal disease features a unique list of symptoms that differs per person, so one GI disease will likely feel different from another. Plus, even the same GI disease may feel different to you compared to your neighbor who also experiences it.
-
The most common symptoms of gastrointestinal diseases include abdominal pain, bloating or distension, changes in bowel habits or stool appearance, nausea and vomiting, difficulty or pain while swallowing, heartburn or reflux, and unexplained changes in appetite or weight. However, these are not all the symptoms of GI disease—and just because you have one or more of these symptoms doesn’t necessarily mean you have a specific illness.
-
You should not ignore the bowel symptoms of black or tarry stools or rectal bleeding. You should seek immediate medical attention if those symptoms occur, or if you experience difficulty swallowing or unexplained weight loss. However, you should also consult a GI provider for any unexplained changes to your bowel habits or stool appearance, even if they are not this drastic.
-
If you are experiencing GI symptoms, talk to a GI provider who can help you investigate whether you have gastrointestinal disease and work with you to come up with treatment and management solutions.
-
Your GI provider may order several tests to diagnose gastrointestinal disease. These may include a colonoscopy, upper endoscopy, imaging, blood tests, and more.
-
GI providers will treat each gastrointestinal problem differently, and likely recommend varied treatment approaches per person. The first step is to talk to a knowledgeable GI provider to help you understand what’s going on and the best treatment options for your unique circumstances.
Oshi is your partner in digestive health
Feel like your digestive concerns are running your life? You’re not alone—and we’re here to help you find lasting relief.
Oshi Health GI providers, gut-brain specialists, and registered dietitians work together to address the root cause of your symptoms and find solutions that actually work for you.
Whether you’re dealing with chronic digestive issues or unpredictable symptom flare-ups, our GI specialists deliver:
✔ Personalized care plans tailored to your lifestyle
✔ Science-backed strategies to calm your gut
✔ Compassionate, whole-person care
✔ And so much more!
Ready to take control of your gut health?