Get clinically-proven, coordinated SIBO care
Experiencing gastrointestinal discomfort is never fun. If that discomfort includes constipation, bloating, stomach pain, loss of appetite, or diarrhea, small intestinal bacterial overgrowth (SIBO) might be to blame. SIBO occurs when there’s an overgrowth of bacteria in the small intestine. While common, it’s also highly treatable. Treatment typically includes antibiotics and following a tailored diet. While there’s no formal or official “SIBO diet,” what you eat (and don’t eat) can help you manage SIBO symptoms for sure.
Manage your SIBO symptoms with a personalized plan. Connect with Oshi Health’s GI specialists for a virtual consultation.
The best nutritional approach to manage those symptoms differs from person to person. Fortunately, there is a process to discover what foods to eat and avoid in order to manage your SIBO symptoms. Ahead, we discuss the process to find SIBO triggers and actionable strategies to manage bacterial overgrowth in the small intestine.
What is small intestinal bacterial overgrowth (SIBO)?
SIBO is exactly what it sounds like: an overabundance of bacteria in the small intestine. Our guts thrive on healthy bacteria in the right quantities and places. When our guts are operating business as usual, the large intestine has more (and more diverse) bacteria than the small intestine.
When more bacteria—good or bad—end up in the small intestine than there should be, SIBO occurs. “There’s often a misconception that SIBO is an overgrowth of ‘bad bacteria’ in the gut,” explains Kaitlin Voicechovski, MS, RDN, LDN, Lead Registered Dietitian at Oshi Health. “It’s more accurate to think of it as bacteria simply hanging out in the wrong neighborhood.”
Get clinically-proven GI care—from almost anywhere
Oshi Health is in-network with most major insurance

Getting gut bacteria out of the wrong neighborhood usually requires a multi-pronged approach: antibiotics prescribed by a gastroenterologist or GI provider alongside lifestyle changes. Making nutritional changes is also important for treating and preventing future bacteria overabundance in the small intestine—but more on that later.

SIBO signs & symptoms
When too much bacteria moves into the small intestine, it can have far-reaching impacts on our health. Common SIBO symptoms include:
- Abdominal pain and/or swelling
- Bloating
- Constipation
- Diarrhea
- Feeling too full after eating
- Gas
- Loss of appetite
- Mood changes
- Unintentional weight loss
If you read that list of symptoms and thought they sounded similar to other gastrointestinal conditions, you would be correct! Diagnosing SIBO is tricky, since symptoms overlap with those stemming from other GI conditions.
Some research suggests over one third of people with other GI conditions experience SIBO, too. Other risk factors for SIBO include being older, a history of abdominal surgery or cancer, and a weakened immune system.
If experiencing the above symptoms (whether you have any, all, or none of the aforementioned risk factors), you should consult a team of GI specialists.
Meet Oshi's GI registered dietitians
Find relief—and stay nourished
When you work with an Oshi GI registered dietitians (RD), you’ll get personalized nutrition guidance, including help with finding and avoiding potential food triggers, choosing gut-friendly supplements and recipes, and more.
SIBO is not something you can self diagnose, and DIYing treatment won’t end well, either. Before your appointment, this GI diagnostic quiz from Tamara Duker Freuman, MS, RD, aka the Bloated Belly Whisperer, may provide useful talking points.
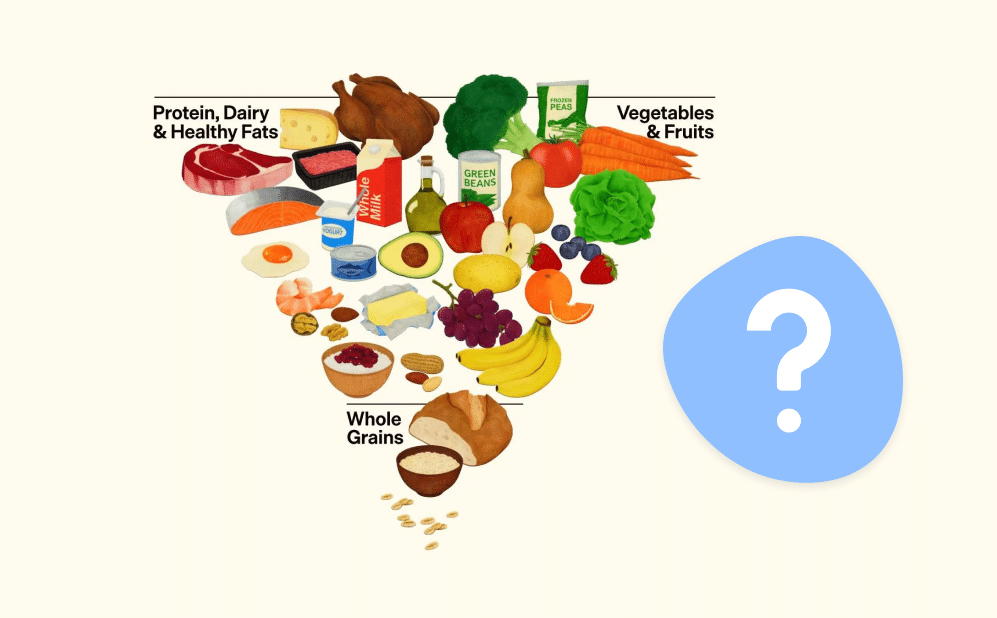
SIBO diet fundamentals
While nutrition alone can’t cure SIBO, what you eat can help with symptom management. For those diagnosed with SIBO, eliminating food triggers may help to reduce uncomfortable GI symptoms. To find these triggers, many turn to an elimination diet such as the low FODMAP diet.
Low FODMAP diet for SIBO
“FODMAPs are carbohydrates that are fermentable by our gut bacteria,” explains Voicechovski. The term is actually an acronym for fermentable oligosaccharides, disaccharides, monosaccharides and polyols (aka four carbohydrate groups that often trigger GI symptoms).
Although, she says, “eating high FODMAP foods, carbohydrates, or any other food does not increase the likelihood of developing bacterial overgrowth,” reducing the amount of FODMAPs may reduce symptoms that are exacerbated by the fermentation of FODMAPs in the gut. “It’s important to note that the low FODMAP diet cannot treat SIBO, rather it can be used as a symptom management tool before and/or alongside treatment,” says Voicechovski.
Don’t just cut out FODMAPs without guidance, though. For one, identifying high and low FODMAP foods without guidance from a registered dietitian (RD) is a tall order. Second, the FODMAP diet is an elimination diet with specific steps to follow. That’s why our clinical team at Oshi only recommends completing the low FODMAP diet under the guidance of an RD.
Foods to eat and avoid
When managing SIBO symptoms, you’ll want to avoid any trigger foods and ingredients, and instead rely on gut-friendly foods. Of course your individual triggers will vary, and you can pinpoint them with the help of your RD. That said, foods that may exacerbate symptoms associated with SIBO include:
Common trigger foods and ingredients
- Apples
- Avocados
- Barley
- Brussels sprouts
- Cashews
- Highly processed meats, especially those that contain high FODMAP ingredients
- Pasta
- Soy beans
- Watermelon
- Wheat bread
Gut-friendly foods
Swap trigger foods for gut-friendly options. Popular options include:
- Almond milk
- Blueberries
- Green beans
- Lactose-free milk
- Oatmeal
- Oranges
- Rice
- Strawberries
- Tomatoes
- Walnuts
Other dietary approaches
Other dietary approaches, such as the elemental diet, are sometimes recommended to manage SIBO symptoms. The elemental diet consists of liquid meals with the basic “predigestive nutrients” our body needs to function (i.e. amino acids, vitamins, short-chain triglycerides, minerals, electrolytes, and short-chain maltodextrins).
When well-tolerated, this diet can help manage symptoms of multiple GI conditions, including SIBO. However, the diet’s rate of intolerance is over 40%, not to mention a liquid only diet isn’t always accessible or socially acceptable.
That’s why Voicechovski notes that strict dietary approaches like this one aren’t ideal for managing SIBO symptoms. She instead recommends finding and eliminating any food triggers (aka trying out the low FODMAP diet) and swapping them for foods that can help manage symptoms.
Managing gut bacteria
Since SIBO involves an overgrowth of bacteria in the small intestine, treatment focuses on reducing the excess bacteria rather than simply rebalancing the gut microbiome. To do so, there are a few must-haves to add to your plate (or supplement line-up):
- Vitamin B-12: “Individuals with SIBO are at a higher risk for B12 deficiency, so focusing on foods rich in B12 such as fish, beef and nutritional yeast or supplementing as needed until levels return to normal should be considered,” says Voicechovski.
- Fiber: Fiber is your gut’s best friend. It can support healthy gut bacteria and can reduce symptoms of many GI conditions. A soluble fiber supplement may be recommended to reduce SIBO symptoms. A registered dietitian can help you choose which type of soluble fiber may work best for your body.
When it comes to supplements, however, you and your RD should be discerning. “There are many supplements on the market touted as a solution for SIBO, and while they may sound enticing, evidence to support them falls short,” says Voicechovski.
One supplement she points out? Probiotics. While probiotics can prevent or treat other GI conditions, including IBS and IBD, most strands are unlikely to help treat SIBO. Some bacteria-based strands may put you at risk of a SIBO recurrence.
Lifestyle and SIBO management
Other SIBO management strategies include improving meal hygiene, starting a food diary, and staying hydrated.
Improve meal hygiene
When Voicechovski works with individuals diagnosed with SIBO, she not only focuses on what they eat, but how they eat. Good meal hygiene can improve digestion and reduce GI symptoms. More specifically, she recommends staying present while eating.
Mindful eating hygiene can include:
- Listening to hunger and fullness cues
- Sitting down to eat
- Not watching TV while eating
- Focusing on the smell and taste of what you’re eating
- Chewing food slowly
- Setting down utensils between bites
- Eating from a well-portioned plate
“While these changes sound simple, they can often be really effective for better digestion and management of unwanted symptoms,” says Voicechovski.
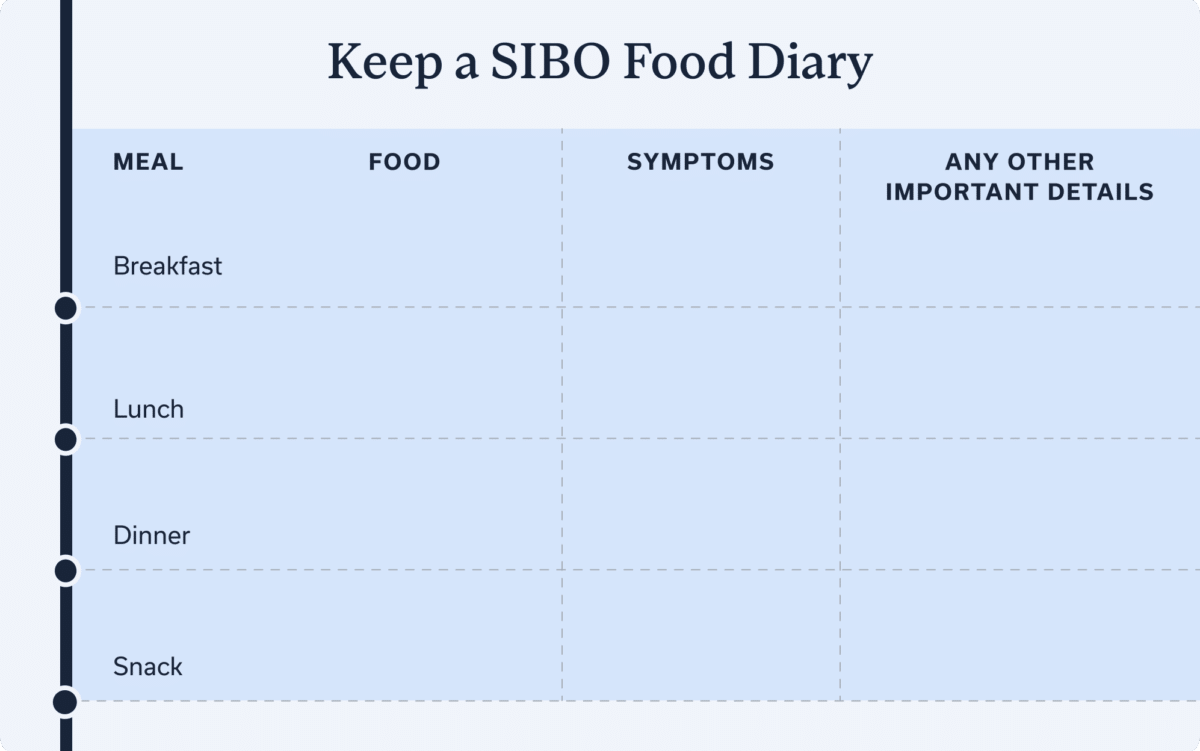
Keep a food diary
When one of Oshi’s patients undertakes a new nutrition program, our RDs often recommend starting a food diary. A food diary is a great way to track when SIBO symptoms occur and which foods you ate around that time.
This food and symptom log can help identify patterns.
You can write in your food diary at each meal or once a day, depending on your preference. Logging intake of food/ beverages and GI symptoms daily (or multiple times a day) is a great way to increase awareness of your symptoms and what you eat.
Stay hydrated
Hydration is key, especially if you have SIBO. A 2022 study looked at how water origin and daily intake impacted gut health in the US and the UK. The researchers’ conclusion: drinking ample water and opting for tap, filtered, or bottled water over well water supports strong gut health. It’s also important to avoid drinking contaminated water (which can include tap water in certain regions in the U.S. and abroad).
Drinking “enough” water can be difficult to define. While there’s a common myth that you should drink 64 ounces a day, one size doesn’t fit all. Instead, the amount of water you need depends on your gender, activity levels, and age.
Sugary drinks and caffeine may also be triggers for SIBO symptoms. If this is the case for you, consider swapping your afternoon coffee or coke out for something more hydrating, like water or tea.
SIBO recovery and relief
As we’ve discussed, nutritional changes alone won’t treat SIBO. Your GI provider may also recommend antibiotics, the first line of defense against SIBO. Talk to your GI provider about which antibiotic may be right for you.
These antibiotics are a short-term, quick fix, not something you’ll utilize for months or years. To complement these temporary solutions, a provider may also recommend the nutritional and lifestyle changes mentioned above.
However, there isn’t one SIBO treatment plan; instead, SIBO recovery should reflect your individual needs and take into account the many aspects of your life and what you eat.
Frequently Asked Questions
-
While there is no official SIBO diet, a nutrition plan with targeted food changes can help manage your SIBO symptoms. What changes you’ll need to make, however, are highly personal. An RD will work with you to identify and avoid your food triggers, which you can do by following an elimination diet. An RD may also recommend supplements containing B-12 or soluble fiber.
-
Foods that trigger SIBO are personal. Fried foods, for example, may make SIBO symptoms worse for one person, but not another. Consulting with an RD can help you determine your personal triggers and help to guide you towards following a diet that is easier for your body to tolerate. A low FODMAP diet is one example of an elimination diet that may help you to identify your food triggers.
-
It is not scientifically proven that you can “starve” bacteria to eliminate SIBO, but reducing individual food triggers can help manage symptoms. Food triggers vary from person to person, making individualized approaches important. An elimination diet, when followed under the guidance of a RD, can help identify which foods worsen your SIBO symptoms and assist in achieving better symptom control.
-
Consuming low FODMAP fruits instead of high FODMAP fruits can help manage SIBO symptoms. Low FODMAP fruits include strawberries, blueberries, cantaloupe, honeydew, kiwi, oranges, pineapple, and rhubarb.
-
The worst foods for SIBO vary from person to person. In general, it’s best to avoid highly processed foods, dairy products (if you are sensitive to lactose,) high-fat foods, and food and drinks that are high in sugar—alongside any other foods that trigger your symptoms personally.
-
One of the most effective diets for managing SIBO symptoms is the low FODMAP diet, but there are many elimination diets that may help. Temporary elimination diets help you and your RD identify food groups and ingredients that trigger your SIBO symptoms. Once identified, you can avoid these triggers, which may reduce symptoms associated with SIBO and prevent future symptom flare-ups.
-
Since our gut microbiome is a complex ecosystem with so many factors in play, It’s not possible to 100% prevent SIBO. If you do experience SIBO, however, it’s possible to prevent future flare-ups. Typically, this is done through short-term antibiotics use and long-term nutritional and lifestyle adjustments. These adjustments vary from person to person, and working with GI specialists can help identify the changes you should make.
-
Technically, no. Though SIBO is treatable, a cure is difficult, since symptoms often come back. But the good news is you can alleviate those symptoms through a combination of nutritional support, lifestyle changes, and sometimes a short course of antibiotics. Since SIBO is a microbial imbalance in your gut, restoring the gut balance can help you successfully treat your symptoms.
-
Elimination diets to pinpoint and avoid your food triggers are temporary. The eventual goal is for every individual to have a wholesome healthy diet without sacrificing many food choices. With these diets, you’ll work with your RD to eliminate potential food triggers for two to six weeks. Over the next six to eight weeks, you will re-introduce those foods, noticing which trigger symptoms and which don’t. Then, you’ll avoid or reduce your intake of foods that trigger symptoms moving forward.
Final takeaways
“SIBO can be successfully treated and gut microbial balance can be restored, though there is risk of recurrence,” concludes Voicechovski, “A GI-focused care team can help individuals with a history of SIBO better understand and address their risk factors to decrease the chance of recurrence.”
If you’re looking for a GI-focused care team, consider signing up for Oshi Health. Our specialists take a whole-person approach to SIBO, which results in 87% of our patients reporting an improved quality of life in less than three months.
Oshi is your partner in digestive health
Feel like your digestive concerns are running your life? You’re not alone—and we’re here to help you find lasting relief.
Oshi Health GI providers, gut-brain specialists, and registered dietitians work together to address your symptoms and find solutions that actually work for you.
Whether you’re dealing with chronic digestive issues or unpredictable symptom flare-ups, our GI specialists deliver:
✔ Personalized care plans tailored to your lifestyle
✔ Science-backed strategies to calm your gut
✔ Compassionate, whole-person care
✔ And so much more!
Ready to take control of your gut health?