Sometimes your menstrual cycle or period may bring along some unpleasant gastrointestinal symptoms, such as diarrhea, constipation, bloating, and more. These symptoms may result from hormonal changes and increases in prostaglandins, which coordinate different bodily functions. However, if you are experiencing ongoing or severe bowel changes, talk to a healthcare provider for an evaluation.
Have you ever felt bloated and stopped up in the days leading up to menstruation only to experience period diarrhea when Aunt Flow finally showed up? Me, too. Sometimes I couldn’t wait for my period just so that the bloating would end. But then I’d have to face additional pelvic discomfort—and stay close to the bathroom.
“Many people notice changes in their digestion around their period—and there’s a scientific reason why,” says Treta Purohit, MD, a gastroenterologist and hepatologist and Executive Medical Director at Oshi Health. “The hormones that regulate the menstrual cycle, especially estrogen and progesterone, also affect the digestive tract.”
Symptoms may include period constipation or diarrhea, bloating or distention, abdominal discomfort, gas, and more. If you, like me, have an existing gastrointestinal (GI) condition, such as irritable bowel syndrome (IBS) or inflammatory bowel disease (IBD), your cycle may also trigger flares of that condition.
“For people with conditions like IBS,” Dr. Purohit, says, “these hormonal shifts can heighten gut sensitivity, making everyday digestive processes feel more intense or uncomfortable.”
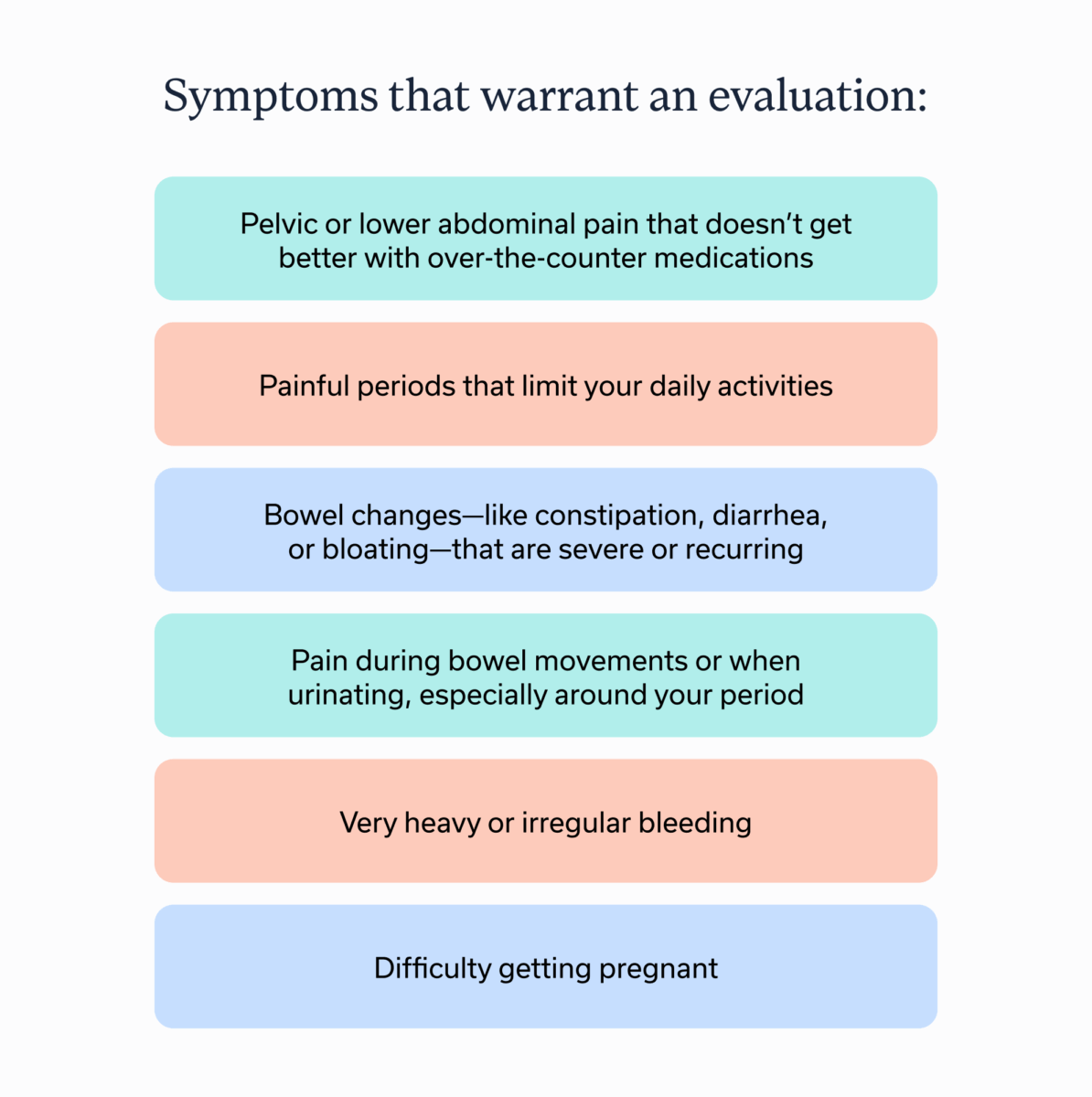
A note before we dig in: Society has a habit of normalizing intense menstrual symptoms, which can make us think we should just “suck up” menstrual pain or GI discomfort that coincides with our cycles. But severe or ongoing symptoms are anything but normal. Ultimately, minor bowel changes occur in the context of hormonal shifts, but anything more than that warrants an evaluation.
Why does your period affect digestion?
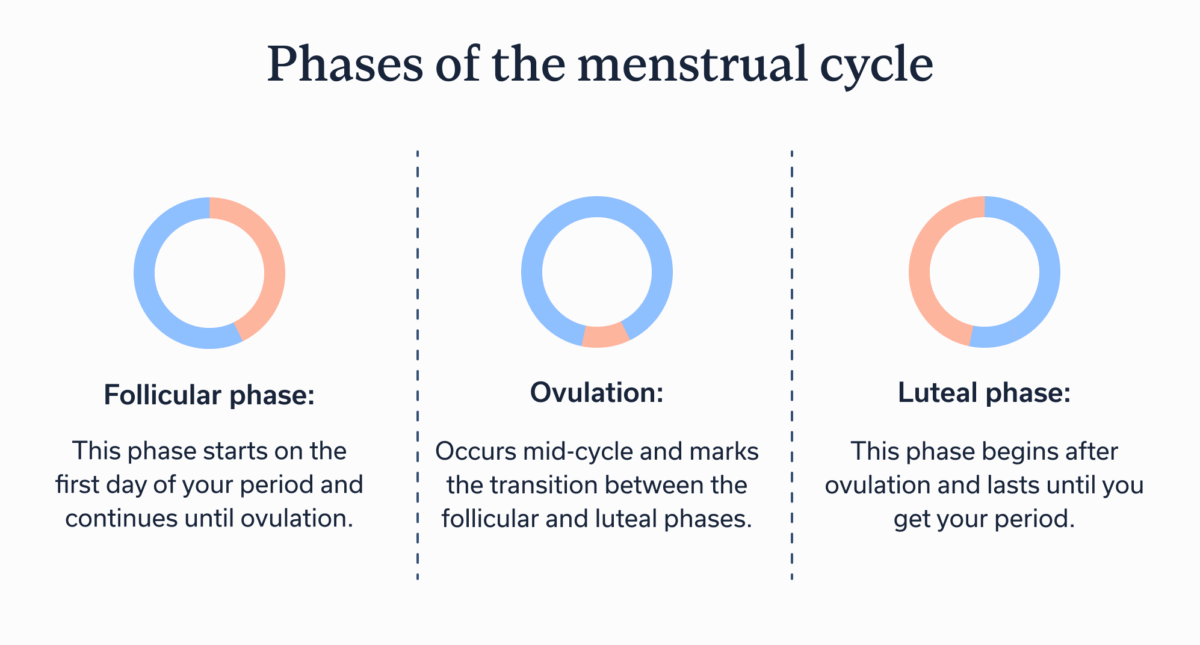
To explain why menstruation can affect the digestive tract, we must explore the phases of the menstrual cycle first. Your cycle occurs because your brain and ovaries communicate via a feedback loop called the hypothalamic pituitary gonadal (HPG) axis. This is why you have two main phases of your menstrual cycle, with ovulation sandwiched between.
- Follicular phase: This phase starts on the first day of your period and continues until ovulation.
- Ovulation: Occurs mid-cycle and marks the transition between the follicular and luteal phases.
- Luteal phase: This phase begins after ovulation and lasts until you get your period.
So why does your digestive system act wonky as you get closer to your period or as you’re menstruating?
“In the second half of the cycle (the luteal phase), progesterone levels rise,” Dr. Purohit says, “This hormone can slow down gut motility, often leading to bloating and constipation.”
She adds, “As the period begins, progesterone drops and levels of prostaglandins rise. These compounds stimulate uterine contractions—but they can also affect the intestines, sometimes triggering diarrhea, cramping, and abdominal discomfort.”
Now let’s explore these issues a bit more.
Period diarrhea: Causes and symptoms
Period diarrhea is exactly what it sounds like: diarrhea that Aunt Flow brings along for the party, though diarrhea may even arrive before your period does.
Symptoms of period diarrhea
- Abdominal cramping and urgency
- Frequent bowel movements
- Loose or watery stools
Dr. Purohit notes that prostaglandins are a likely culprit. “Prostaglandins are natural chemical messengers that play a key role in inflammation—and they can directly impact your gut,” she says.
Prostaglandins are not hormones, but they act like them. In reality, they are lipids (fats), but they are involved in pain and inflammation, blood clotting and flow, pregnancy and labor, and—you guessed it—menstruation. During menstruation, prostaglandins cause your uterus to contract and then shed the uterine lining, aka period blood.
One type, prostaglandin E2 (PGE2), is implicated in diarrhea. “When inflammation occurs (from your period, an infection, or a condition like IBD), PGE2 levels rise in the gut,” Dr. Purohit explains. “This activates certain receptors on the cells lining your intestines, triggering the release of fluids—particularly chloride and water—into the bowel. This results in softer or more frequent stools.”
Prostaglandins also impact your gut-barrier function, adding to the effect. “PGE2 weakens the ‘tight junctions’ between the cells in your gut lining, making it more permeable (‘leaky’),” she says. “That allows even more fluid to move into the intestines, adding to the diarrhea.”
As if these factors weren’t enough to cause loose stool, based on early studies conducted on mice, we have reason to believe that PGE2 also boosts nerve signals that further increase fluid secretion.”As if these factors weren’t enough to cause loose stool, PGE2 also boosts nerve signals that further increase fluid secretion, according to early studies in mice. “While this can be a helpful defense mechanism in short-term infections,” Dr. Purohit adds, “it can also contribute to chronic symptoms in conditions like IBS, IBD, or even some hormone-related tumors.”
Additionally, some people have a higher level of prostaglandins. I’m raising my hand here because of my endometriosis, a chronic condition linked to higher prostaglandin levels, contributing to pain and other symptoms. Although endo pain can occur at any time during one’s cycle, it’s more prevalent right before and during your period.
Managing period diarrhea
Now that you know the chemical messengers responsible for your period diarrhea, you may be wondering how to gain better control over the onslaught. The solution involves focusing on lifestyle changes while mitigating triggers.
“A diet high in processed foods and sugar, chronic stress, poor sleep, and underlying gut or mental health conditions can all contribute to worse diarrhea during your period,” Dr. Purohit says. “Taking a whole-person approach to wellness—including food, sleep, stress, and mental health—can help ease the burden.”
However, personalization is key. “Because everybody is different, these suggestions work best when tailored to you,” she says.
Expert-led care, tailored to you
Here to tackle your GI symptoms from all angles
Make dietary changes
“Eating a lot of refined carbs, processed meats, and sugary foods,” Dr. Purohit says, “has been linked to more severe menstrual symptoms, including digestive issues like diarrhea. In contrast, diets rich in whole foods, fiber, and anti-inflammatory nutrients may help ease symptoms.”
A GI registered dietitian like those at Oshi Health can help you build a nutritional plan that addresses your unique needs and preferences, but here are a few of Dr. Purohit’s general recommendations:
- Eat regular meals: “Skipping meals or eating irregularly can disrupt digestion,” she says. “Try to maintain a consistent eating schedule.”
- Limit caffeine, alcohol, and fizzy drinks: “These can stimulate the gut and worsen diarrhea,” Dr. Purohit notes. “Opt for non-caffeinated, hydrating beverages instead.”
- Drink plenty of water: “Staying hydrated is key—especially when you’re losing fluids from diarrhea,” she adds.
- Adjust fiber intake: “Reducing insoluble fiber (like bran, raw vegetables, or whole grain cereal) may help,” Dr. Purohit says. “Instead, try incorporating small amounts of soluble fiber, starting with 1 to 2 teaspoons per day and adjusting as needed.”
- Watch for artificial sweeteners: “Ingredients like sorbitol or mannitol (found in sugar-free gum and snacks) can cause loose stools in some people,” she adds.
- Try a low FODMAP approach: “Some find relief by limiting fermentable carbs (like certain fruits, dairy, or sweeteners),” says Dr. Purohit. “A food diary can help you track patterns and identify personal triggers.”
Get adequate sleep, reduce stress, and focus on mental health
“Emotional stress and poor sleep are common triggers that can worsen both GI symptoms and menstrual discomfort,” Dr. Purohit says. “High stress levels can activate gut-brain pathways that make the digestive system more reactive.” Aim for at least seven hours of quality sleep per night, and reduce stress through mindfulness, deep breathing, or other calming routines, she recommends.
“Anxiety, depression, and health-related worries have all been associated with heightened menstrual and gastrointestinal symptoms,” Dr. Purohit adds. “These conditions may amplify how the body perceives pain or discomfort, particularly during hormonally-sensitive times.”
A gut-brain specialist like those at Oshi Health can help you improve communication along the gut-brain axis, the system by which the gut and brain communicate with each other. Mental health conditions, whether depression, anxiety, or chronic stress, can negatively affect the gut, and vice versa. That’s why improving gut-brain communication and reducing stress may help ease period diarrhea.
Period constipation and bloating: Why it happens
While period diarrhea tends to occur right before or during menstruation, period constipation and bloating tend to wreak their havoc in the days or the week leading up to menstruation.
Symptoms of period constipation and bloating
- Abdominal discomfort or cramping
- Bloating or distention
- Feeling as if bowel movements are incomplete
- Gas
- Hard, pebble-like stool
- Less frequent bowel movements
- Straining on the toilet
In the case of these symptoms, the culprit is potentially progesterone, a hormone that rises shortly after ovulation before falling again before your period.
“One of [progesterone’s] lesser-known effects is how it slows down the movement of your digestive system,” Dr. Purohit says. “It relaxes the muscles in your gut, which means food and waste move more slowly through your intestines. This slower movement—called reduced gut motility—can lead to harder stools and constipation.”
Progesterone impacts receptors in the gut lining and changes the normal signals that tell intestinal muscles to contract. “It increases levels of nitric oxide, a chemical that relaxes smooth muscle, and shifts the balance of signaling proteins to favor relaxation over contraction,” Dr. Purohit explains. “This results in lesser contractions (peristalsis) needed to keep stool moving through the colon.”
These same mechanisms can also lead to bloating, but progesterone may also contribute to bloating by causing fluid retention.
Some people, including me, have a heightened sensitivity to progesterone (aka progesterone intolerance), as well, which could compound the issue with pre-period constipation and bloating.
How to relieve period constipation and bloating
If progesterone appears to be giving you period problems, some solutions—many of which are similar to those for diarrhea, while others are different—may help.
Make dietary changes
Dietary changes are highly personal, and what improves—or worsens!—your symptoms will be different from the next person’s. Working with a GI registered dietitian can help you develop a dietary plan that eases premenstrual constipation. Strategies may include increasing fiber, avoiding trigger foods, eating to increase the diversity of the microbes in your gut, and more.
Stay hydrated
Hydration is linked to a lower risk of constipation. Drinking water helps keep things, such as fiber, moving through the digestive tract. So drink up throughout the day.
Get plenty of physical activity
Engaging in physical activity may also reduce your risk for constipation. Exercise increases blood flow and encourages the natural contractions of your GI tract that help move waste on through, speeding up gut motility.
Prioritize sleep, stress reduction, and mental health
Getting good quality sleep is a tenet of health, but if you need another reason to tuck yourself in early, keep in mind that poor quality and inadequate sleep may increase your risk for constipation. Aim for at least seven hours per night of relatively uninterrupted slumber.
Chronic stress, anxiety, depression, and other mental health concerns all share links with worsened GI symptoms, including constipation and bloating. Improving gut-brain communication can help. One option is to enlist the help of a gut-brain specialist such as a GI psychologist.
Consider over-the-counter options
Some over-the-counter medications or supplements may be able to help. For example, you might wish to take a stool softener or osmotic laxative (e.g., MiraLAX or magnesium citrate), as your progesterone levels increase. Cycle lengths vary from 21 days to 35, but if you have a 28-day cycle, your progesterone level will begin to rise just after ovulation, peaking around day 21 or 22.
A knowledgeable GI specialist can help determine what over-the-counter options are best for you and strategies for including them based on factors unique to your cycle. Or they may even prescribe a medication where necessary.
When to see a doctor
“It’s very common to notice digestive changes during your menstrual cycle—things like bloating, constipation, loose stools, or cramping,” Dr. Purohit says. “These symptoms are often related to normal hormonal shifts, and for many people, they’re mild and manageable. But if your symptoms are more intense, frequent, or affecting your daily life, it’s important to talk to your doctor.”
She says she considers several factors to assess whether symptoms are “normal” or part of a greater issue. For example, if symptoms change or get worse over time, interfere with everyday activities, or are accompanied by other symptoms like pain or bleeding, it could be indicative of something more serious. The following are symptoms Dr. Purohit says warrant an evaluation:
- Pelvic or lower abdominal pain that doesn’t get better with over-the-counter medications
- Painful periods that limit your daily activities
- Bowel changes—like constipation, diarrhea, or bloating—that are severe or recurring
- Pain during bowel movements or when urinating, especially around your period
- New or worsening pain with intercourse
- Very heavy or irregular bleeding
- Difficulty getting pregnant
“When GI symptoms cycle with your period—especially when they’re severe or accompanied by pelvic pain—we also consider conditions like endometriosis,” she says. “It’s not uncommon for endometriosis to affect the bowel or mimic IBS, and in some cases, it can take years to diagnose without the right attention.”
This was the case for me. My endometriosis symptoms began with the start of my period at age 11, but I did not receive a definitive diagnosis of endo until I was 21. Why? As mentioned earlier, society tends to normalize period pain, so I thought extreme pain was normal. When I did consult my doctor about the pain, he did not express concern, so I endured it until it got so extreme I could barely function.
Yes, premenstrual syndrome (PMS) does occur, which may include some cramping, but extreme pain is not normal and should be evaluated. Experts consider endometriosis to be among the 20 most painful conditions. If a doctor does not take your symptoms seriously, seek another opinion.
The American College of Obstetricians and Gynecologists (ACOG) recommends further evaluation if menstrual pain doesn’t improve after three to six months of trying first-line treatments like nonsteroidal anti-inflammatory (NSAID) medications or hormonal birth control. Like Dr. Purohit, they also recommend investigating symptoms if they are persistent, getting worse, or raising concern for other underlying conditions.
“You don’t have to navigate this alone,” Dr. Purohit says. “We’re here to listen, investigate, and support you in getting the right care and referrals.” She recommends keeping track of your symptoms and when they happen in your cycle and then sharing that info with your provider at your appointment.
Key takeaways
- Your period may produce GI symptoms, such as constipation and bloating or diarrhea.
- Often constipation and bloating show up before your period, resulting from an increase in progesterone.
- Diarrhea, on the other hand, could be a result of chemical messengers called prostaglandins, which increase just before and during your period.
- If you have ongoing or severe bowel changes with your menstrual cycle, talk to a healthcare provider. A GI specialist, such as those at Oshi Health, can evaluate you for any underlying conditions and help you find relief from digestive symptoms.
FAQ
-
Many people experience diarrhea during their period or even in the days just before menstruation. This is likely because of an increase in prostaglandins, chemical messengers that cause your uterus to contract and then shed the uterine lining, aka period blood. Prostaglandins also affect the digestive tract, increasing fluid in the intestines and altering nerve signaling. Although minor bowel changes are a normal part of menstruation, severe or ongoing issues are not normal and could be symptoms of an underlying condition, such as endometriosis.
-
If you have irregular cycles, missed cycles, pain that goes beyond mild cramping, severe bowel changes that coincide with your cycle, heavy bleeding, or bleeding when you’re not on your period, you should seek an evaluation with a healthcare provider. These issues can signal underlying conditions, including endometriosis.
-
If you experience loose stool during your period, your body may be reacting to prostaglandins, which we’ve explained are chemical messengers that cause your uterus to contract and then shed your uterine lining. Prostaglandins also affect your digestive tract, increasing fluid in the intestines and altering nerve signaling, which could produce loose stool.
-
Many things can cause your period to be late or to not come at all, including pregnancy, stress, or underlying conditions. You might also occasionally skip a period. As detailed above, diarrhea may result from an increase in prostaglandins, chemical messengers involved in uterine contraction during menstruation. Increased cramping or loose stool could indicate your period is on its way. However, if you continue to have an absence of a period along with bowel changes, consult your healthcare provider.
Personalized care for the whole you
Did you know women are more likely to experience gastrointestinal (GI) symptoms and conditions than men? That’s because hormones and reproductive health have a major impact on the gut-brain connection—and vice versa!
At Oshi Health, we work with you to understand your unique situation, including how your cycle might impact your GI symptoms. Our goal is to create a personalized care plan that fits your lifestyle.
Here’s what you’ll get:
✔ A personalized care plan tailored to you
✔ Nutrition guidance rooted in scientific research
✔ Proven techniques to calm your gut and ease discomfort
✔ Compassionate, whole-person care
✔ And so much more!
Ready to find lasting symptom relief?