Menstruation isn’t the easiest time of the month. For many people, uncomfortable symptoms like bloating, cramping, and mood swings can be downright disruptive to daily life. But for those living with inflammatory bowel diseases (IBD), period-related symptoms like cramping, bloating and gastrointestinal (GI) upset, are sometimes reported to be much more severe—and last much longer.
“I hear it all the time from Crohn’s patients,” says Katherine Freeman, MD, a gastroenterologist at Mount Sinai Hospital in Manhasset, New York. [Women usually experience] the trifecta of abdominal pain, bloating or diarrhea—or all of the above—during their period, and right before.”
How your period affects your digestive tract
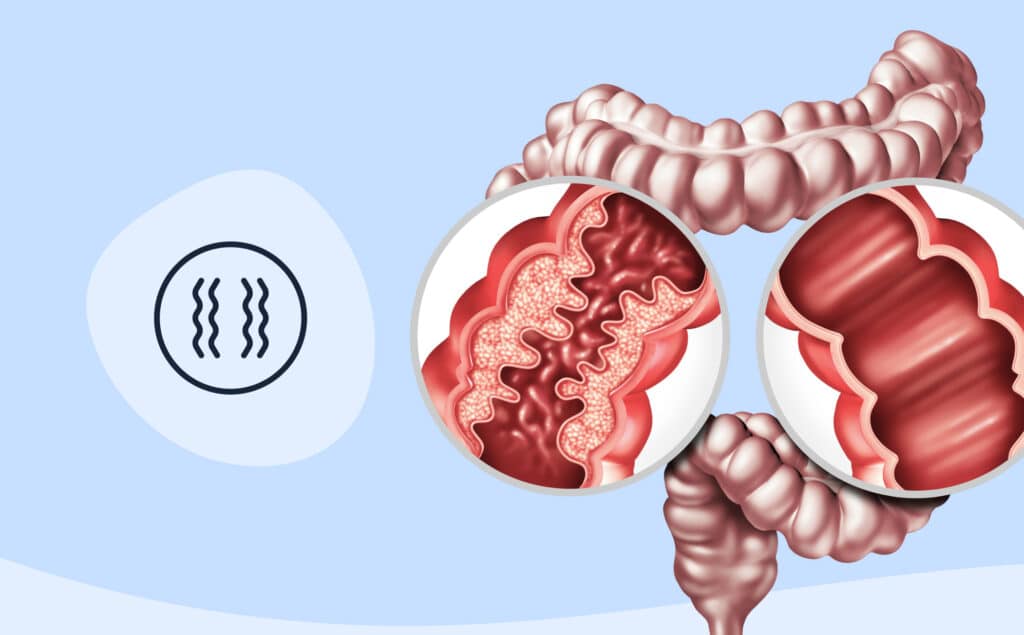
So, why do some people experience a worsening of GI symptoms during their period? More research is needed, but some evidence suggests that fluctuations in hormones throughout the menstrual cycle—such as estrogen, progesterone and prostaglandins—may be to blame.
Prostaglandins, for example, are responsible for the smooth muscle contractions that help the uterus shed its lining during menstruation, so they may also trigger muscle contractions in the intestines, according to Freeman. Other data says that, among those with slow-transit constipation, progesterone receptors in the GI tract may respond to fluctuations in prostaglandin levels.
Dr. Freeman adds, “Even in women who don’t have Crohn’s, there tends to be a prolonged GI transit time during the luteal phase [the time after ovulation that ends just before a period] of their cycle. That means you tend to have worsened gastrointestinal symptoms during this phase.”
Ways to feel better during your period
While many people with (and without) Crohn’s experience worsened GI symptoms with their periods, it’s important to note that not everyone will. If you do have severe cramping, bloating, or diarrhea, however, there are ways to manage your symptoms—and feel better during your period.
1. Skip the NSAIDs
Certain nonsteroidal anti-inflammatory drugs, like ibuprofen or naproxen, are often the go-to treatment for period pains. In people with Crohn’s, however, these drugs can make GI symptoms worse.
“The first thing I always recommend is to not take any nonsteroidal anti-inflammatory drugs. They can exacerbate Crohn’s and colitis whether or not women have their periods,” says Dr. Freeman. Over-the-counter painkillers containing acetaminophen may offer some relief.
2. Apply heat
“Heating pads are my best friend!” says Stacy Ransom, 28, from Corona, California. “They relax crampy muscles and feel comforting.” Whether you opt for a heating pad or warm bath, applying heat to achy muscles can soothe period pains and may relax tight muscles.
3. Stay active—if you’re up to it
When you’re dealing with painful symptoms, exercise may be the last thing you want to do—but it can help reduce stress, a common trigger for IBD.
“Staying active can sometimes feel difficult when living with a chronic illness—there are some days it just isn’t going to happen! I listen to my body, and on days when I need to rest, I am sure to rest,” says Eleanor Meghan, 26, from Colorado Springs, Colorado. She underwent surgery for a permanent ileostomy in 2016, and dealt with extremely painful periods prior to her procedure. Meghan adds, “Staying active through yoga and biking on a recumbent bike allows me to exercise without overdoing it.”
4. Practice self-care
We all know that self-care is vital to physical, emotional and mental health. Dr. Freeman recommends practicing self-care to manage severe period and GI symptoms.
During her period, Emma Illingworth, 21, from Leeds, UK, gets plenty of sleep; reduces her caffeine intake, which can worsen symptoms; wears loose clothing to deal with uncomfortable bloating; and stays hydrated. She adds, “I tend to take a few days to practice self-care and ease myself back into the normality of chronic illness.”
5. Give your body rest
When you have a chronic illness, it’s important to listen to your body’s cues. Stephanie Dawn, 31, New York, New York, was diagnosed with Crohn’s at age 9 and has found that rest can dramatically improve her symptoms: “The most important thing is to rest. Pushing yourself when your body is already struggling is only going to make things worse.”
“During my period, I focus on relaxing and try to create as calm an environment for myself as I can,” adds Dawn.
6. Manage your stress
Stress has been linked to a number of chronic conditions—as well as body-wide inflammation—and Crohn’s disease is no different.
For many people, stress can be a major trigger for uncomfortable period symptoms: “My biggest trigger was (and still is) stress. Learning how to manage my stress has really helped me manage my disease,” says Meghan. Stress management techniques like meditation, belly breathing, journaling, listening to music, and practicing self-care may help you get your daily stressors under control.
7. Take care of your mental health and connect with others
If your period leaves you feeling alone, confused, or angry, try reaching out to other people living with Crohn’s. Dawn says, “One of the biggest things that helped me mentally cope with my illness was finding a community. [Using] applications like Instagram, I’ve met so many wonderful people fighting the same battle I am. So please, if you’re struggling or you feel lost and alone, reach out to some of us.”
Meghan adds, “There is a huge community of other people dealing with the same symptoms, disease flares, discomfort, and mental upset that you may be facing. The best thing you can do? Connect with them!”
8. Talk to your doctor
If you start to experience new or worsened symptoms, tell your gastroenterologist ASAP. “My best piece of advice is to get the disease under control as quickly as possible. It’s a lot harder to play catch-up when the disease gets out of control, and medications can only go so far. If you can get it under control in its infancy, you’ll be a lot better off,” says Dr. Freeman.
If you’re experiencing severe period symptoms or want to try a new treatment for painful periods, don’t hesitate to talk to your gastroenterologist or gynecologist. Your provider will be able to help you determine the right course of treatment for your Crohn’s disease and lifestyle.
Medically reviewed by Jenny Blair, MD
Oshi is your partner in digestive health
Feel like your digestive concerns are running your life? You’re not alone—and we’re here to help you find lasting relief.
Oshi Health GI providers, gut-brain specialists, and registered dietitians work together to address the root cause of your symptoms and find solutions that actually work for you.
Whether you’re dealing with chronic digestive issues or unpredictable symptom flare-ups, our GI specialists deliver:
✔ Personalized care plans tailored to your lifestyle
✔ Science-backed strategies to calm your gut
✔ Compassionate, whole-person care
✔ And so much more!
Ready to take control of your gut health?