Ulcerative Colitis Overview
Ulcerative Colitis Overview
Ulcerative colitis (UC) is a type of inflammatory bowel disease (IBD) involving chronic inflammation and ulcers in the inner lining of your large intestine (also called the colon) and rectum.
People with UC typically experience a gradual worsening of symptoms over time. Even though most people alternate between periods with painful, uncomfortable symptoms (flares) and with no symptoms (remission), flare-ups can have a profound impact on your quality of life, making it tough to navigate social situations and other aspects of daily living.
Read on to learn about ulcerative colitis symptoms, causes, risk factors, and complications—and how we can help you find relief.
Ulcerative colitis symptoms
Wondering if your symptoms might be ulcerative colitis or looking to better understand your condition? Let’s explore some of the signs of ulcerative colitis and get you the answers you need, whether you’re newly concerned or already have a diagnosis.
Ulcerative colitis symptoms can come and go, with days, weeks, months, or years of remission between flare-ups.
Common symptoms of ulcerative colitis include:
- Diarrhea
- Blood in the stool or rectal bleeding
- Abdominal pain or cramping
- Mucus or pus in the stool
- Urgent need to have a bowel movement
- Tenesmus, a constant urge to poop, often despite having empty bowels
Living with ulcerative colitis symptoms can be uncomfortable, but it’s important to know that you’re not alone. Estimates suggest over 2.3 million adults in the U.S. have an IBD diagnosis like ulcerative colitis—and that doesn’t account for those who live with symptoms but have yet to seek help.
At Oshi Health, our GI specialists, including GI providers, registered dietitians, and gut-brain specialists, work together to address your ulcerative colitis symptoms.
I wasn't sure how comfortable I would be discussing my UC with a new doctor. But I was immediately put at ease and even learned something new—I was surprised since I have lived with this condition for 15 years. I really enjoyed my visit!
— Darcy, Oshi Health patient
Ulcerative colitis causes
It’s unclear exactly what causes ulcerative colitis in some people but not others, but evidence suggests an interaction between the following may be at play:
- Your genetics. Research shows that there may be a link between certain genes and ulcerative colitis. Your risk of developing ulcerative colitis is higher if a first-degree family member (parent or sibling) also has a form of IBD.
- Your immune system. Ulcerative colitis may involve an abnormal immune response—possibly triggered by certain gut microbes, causing the body to mistakenly attack cells in the digestive tract. This causes gut inflammation that leads to uncomfortable GI symptoms.
- Your environment. Researchers are also looking into how the world around you might interact with your unique genetic makeup, gut microbiome, and immune system to trigger conditions like ulcerative colitis.
And while stress isn’t a known ulcerative colitis cause, research suggests stress (hello, gut-brain connection) may worsen inflammation and trigger symptoms.
Ulcerative colitis risk factors
Just because you have a risk factor doesn’t mean you’re destined to get ulcerative colitis, but it can mean you’re more likely to develop the condition than someone else.
Ulcerative colitis risk factors include:
- Having a parent or sibling with an inflammatory bowel disease (IBD)
- Being younger than 35 (the typical age range when IBD gets diagnosed—but some people go longer without getting a diagnosis and onset can happen at any age)
- Being Caucasian, especially of Ashkenazi (Eastern European) Jewish descent, though ulcerative colitis can affect people of all ethnicities
- Taking nonsteroidal anti-inflammatory drugs (NSAIDs), which can also worsen ulcerative colitis
Where you live may also play a role in ulcerative colitis since it’s more likely to affect people living in northern climates, high-income countries, and big cities.
Ulcerative colitis complications
Before we dig into this scary stuff, we want to make sure you know that just because you have ulcerative colitis doesn’t mean you’ll develop complications. Seeking treatment for your ulcerative colitis and managing your symptoms can make you less likely to experience serious side effects.
Over time, untreated ulcerative colitis can damage the lining of your large intestine, leading to serious ulcerative colitis complications like:
- Anemia. UC can cause bleeding and inflammation, which can lead to a red blood cell deficiency known as anemia.
- Dehydration. Frequent severe diarrhea can lead to dangerous dehydration that may require intravenous (IV) rehydration in the hospital.
- Inflammation elsewhere in the body. UC can also cause inflammation in other parts of the body, including your joints, skin, eyes, and liver.
- Developmental problems. In kids, UC can impact growth and even delay puberty—which is why it’s commonly diagnosed before most people hit their 30s.
- Osteopenia or osteoporosis. Both UC and certain UC treatments, like corticosteroids, can impact bone health.
- Blood clots. Having UC can put you at a higher risk of developing blood clots.
- Strictures. Recurrent inflammation can cause narrowing of the colon known as strictures.
- Fulminant ulcerative colitis. This is complication causes frequent bloody bowel movements, severe anemia, fever, and rapid heart rate.
- Intestinal perforation. Inflammation can eat away at the lining of your large intestine, creating a hole or perforation.
- Severe bleeding. Heavy bleeding from or through the rectum may require emergency surgery.
- Toxic megacolon. Left untreated, inflammation can spread and cause severe swelling of the large intestine, preventing it from emptying.
- C. difficile infection. A bacterial infection that can cause symptoms similar to IBD flares.
Having ulcerative colitis may also increase your risk of developing colorectal cancer—the risk is higher with untreated ulcerative colitis.
Read more about this link in our blog: How IBD affects your colorectal cancer risk.
Curious about your colon cancer screening options? Connect with an Oshi Health GI specialist to find which screening option is right for you.
Ulcerative colitis diagnosis
The first step toward an ulcerative colitis diagnosis is a thorough medical history. At Oshi Health, our multidisciplinary GI specialists consider the whole you when working together to make a diagnosis, including your medical history, symptoms, and lifestyle.
An integrated team of GI specialists, working together for you
Our expert gastroenterologists, GI providers, registered dietitians, and gut-brain specialists are leaders in their fields, with advanced education and training in gastroenterology. Our comprehensive team approach is personalized to meet your unique needs and address the root cause of your symptoms.
Your providers will ask you questions about your symptoms, like when diarrhea typically occurs or whether certain foods or behaviors tend to make certain symptoms worse.
They’ll also consider the following:
- Your family history
- Your diet
- Lifestyle habits
- Any medications or supplements you’re taking
- Stress and behavioral health
- Previous surgeries or medical procedures
And while you don’t need to have had previous testing to meet with an Oshi provider and benefit from our integrated GI care, your provider will review any previous testing you’ve gone through, if any.
They may also recommend additional testing if you have a combination of risk factors, including a family history of colorectal cancer, or serious symptoms like:
- Unexplained weight loss
- Blood or blood clots in your stool
- Severe abdominal pain that doesn’t go away
- A high fever
- Diarrhea at night
Further testing might include:
- Blood tests for ulcerative colitis can check for signs or complications of UC, including low red blood cell count, which may signal anemia.
- Stool tests for ulcerative colitis look for other potential underlying causes that may explain your symptoms, like an infection. Stool tests can also help determine whether there is inflammation in your lower digestive tract.
-
Two types of endoscopy for ulcerative colitis help healthcare professionals visualize the large intestine: colonoscopy and flexible sigmoidoscopy.
These tests can:
- Check for signs of UC
- Determine UC severity
- Rule out other GI conditions
While some forms of testing, like a colonoscopy, might be necessary for diagnosis, we try to avoid putting you through unnecessary and repeat testing. If our providers recommend diagnostic or other testing, we take a concierge approach to help you find a convenient and in-network location.
Ulcerative colitis treatment
We take a comprehensive approach to ulcerative colitis treatment, by treating the disease and addressing diet and lifestyle factors that can contribute to symptom flare ups.
In-network with most major health plans
Unlike traditional healthcare providers, we don’t bill on a per visit basis. With insurance coverage, most Oshi Health patients get a year of unlimited care and only pay for four in-network specialist visits. For those four visits, copays and deductibles apply based on your plan benefit details.

Here’s how our providers work together to put you on a path to better digestive health:
1. Prescribing or recommending medications
Medications are often part of personalized treatment plans for ulcerative colitis at Oshi Health.
Your provider will recommend medications based on disease severity and location, and other factors unique to you.
The following prescription medications may help relieve symptoms during an ulcerative colitis flare and prevent future flares:
- Steroids. Corticosteroids help calm your immune system and decrease inflammation in your large intestine, helping with moderate to severe ulcerative colitis symptoms. Because steroids come with side effects, they’re not ideal for long-term use.
- Aminosalicylates. These medications help control inflammation and may help keep you in remission. They’re typically recommended for people with mild to moderate UC.
- Immunomodulators. These medications help control your body’s immune response, limiting the inflammation that triggers ulcerative colitis symptoms. Your provider may recommend immunomodulators if you have severe symptoms or haven’t had success with other treatments.
- Biologics. These medications neutralize specific proteins produced by your immune system to help limit inflammation. They’re typically prescribed to treat moderate to severe ulcerative colitis.
- Targeted synthetic small molecules. These medications target parts of the immune system to decrease inflammation. They’re prescribed to treat moderate to severe ulcerative colitis.
- Surgery. People with severe symptoms or complications from ulcerative colitis who haven’t seen success with other treatments may benefit from surgery.
Your provider can also prescribe medications to help manage uncomfortable symptoms, like mild pain.
Medications are just one piece of the journey to symptom relief. Our whole-person approach to GI care also looks at lifestyle factors such as diet and stress that may be contributing to symptom flares.
2. Identifying triggers & making dietary and lifestyle adjustments
What does your typical diet look like? Do you have dietary triggers that seem to make your symptoms worse?
What you eat can’t cause ulcerative colitis, but some foods can aggravate symptoms. Our registered dietitians will help you identify your ulcerative colitis-trigger foods and find ways to modify your diet without necessarily giving up the foods you love.
Your diet might look different depending on whether you’re in a flare or remission. Our RDs offer personalized recommendations based on your unique needs to make sure you’re well-nourished.
Depending on what triggers ulcerative colitis symptoms for you, management might also involve:
- Focusing on boosting your soluble fiber intake to ease diarrhea
- Eating smaller, more frequent meals
- Chewing more thoroughly to reduce your risk of bowel obstruction
- Limiting FODMAPs in your diet
- Incorporating a GI-gentle diet when you’re experiencing a flare
- Adopting a Mediterranean diet
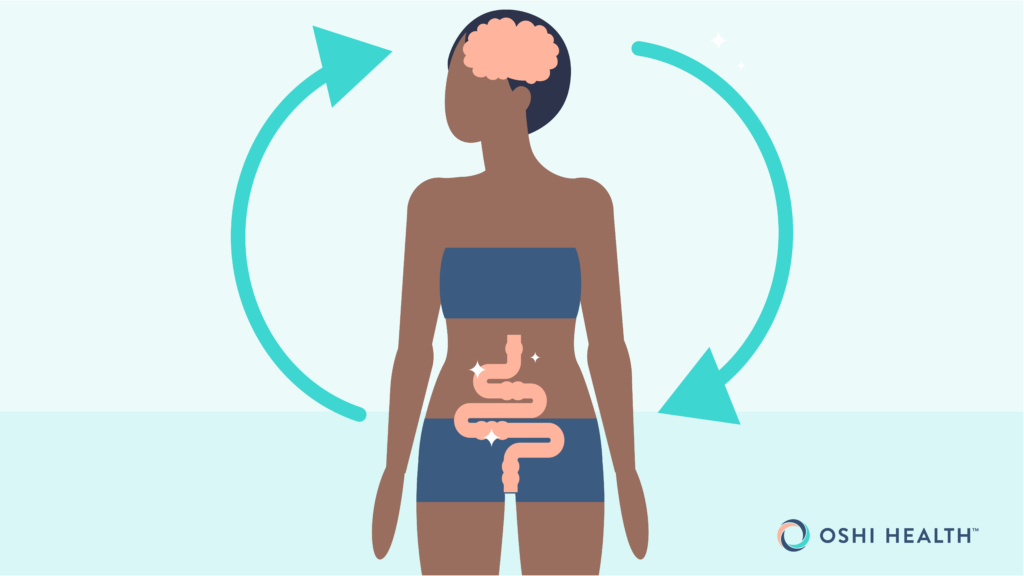
3. Working on the gut-brain connection
Did you know your brain and digestive system are in constant communication? It’s why you might feel butterflies in your stomach when you experience heightened emotions like stress or excitement.
The close link between your gut and mind can also play a role in conditions like ulcerative colitis.
Living with a chronic condition like ulcerative colitis can be incredibly stressful. Stress can actually make your symptoms worse, creating a vicious cycle where stress and GI discomfort feed off each other.
Our gut-brain specialists can help you identify potential stress-related triggers causing excess inflammation that leads to symptom flares. They can also help you cope with the emotions that come hand in hand with living with a chronic condition.
Gut-brain specialists are trained and licensed behavioral health professionals with specific experience treating GI concerns like ulcerative colitis. Working alongside GI providers and registered dietitians, they can help you take control of your symptoms by providing you with the skills and tools to cope with distressing thoughts, feelings, and physical reactions that may be contributing to GI distress.
This might include:
- Relaxation strategies to manage stress, including diaphragmatic breathing exercises and mindfulness meditation
- Cognitive behavioral therapy (CBT) for GI symptoms to help you better cope with negative emotions relating to your condition, including feelings of embarrassment and shame
- Acceptance and commitment therapy (ACT) for GI conditions to move towards a place of acceptance and identify the ways you might be avoiding certain situations, which could make it more challenging to cope with symptoms
Oshi Health gut-brain specialists are here to support you as you navigate living with a chronic digestive health condition, helping to normalize and validate your GI-related concerns—so you never feel alone in your journey to symptom relief.
4. Whole-person care for ulcerative colitis
At Oshi, no two treatment plans are the same.
Our GI specialists work together to create a personalized treatment plan to address the root cause of your symptoms. We consider the whole you—not just your ulcerative colitis diagnosis. That means taking into account diet, lifestyle, and the gut-brain connection, ensuring you get the individualized care you need.
Already seeing a GI provider? We can provide support between visits and work with your existing gastroenterologist as an extension of your care.
- decrease in unnecessary (and expensive) procedures and tests
- of undiagnosed patients get a clear diagnosis within 3 months
- of patients report better quality of life, with less stress and anxiety, within 3 months
Source: Results of a clinical trial conducted in partnership with a national health plan
Oshi is your partner in digestive health
Feel like your digestive concerns are running your life? You’re not alone—and we’re here to help you find lasting relief.
Oshi Health GI providers, gut-brain specialists, and registered dietitians work together to address the root cause of your symptoms and find solutions that actually work for you.
Whether you’re dealing with chronic digestive issues or unpredictable symptom flare-ups, our GI specialists deliver:
✔ Personalized care plans tailored to your lifestyle
✔ Science-backed strategies to calm your gut
✔ Compassionate, whole-person care
✔ And so much more!
Ready to take control of your gut health?
Frequently Asked Questions
-
There’s no cure for ulcerative colitis, but it’s possible to manage your condition and experience lengthy periods of remission where you have no symptoms. Working with a GI specialist to find a treatment plan that works for you can help you spend more time in remission.
-
What you eat doesn’t cause ulcerative colitis, but some foods can aggravate symptoms.
Not everyone with ulcerative colitis will have the same trigger foods. Examples of foods that may worsen symptoms include:
- Foods high in insoluble fiber, like sunflower seeds
- High-fiber foods like beans, cabbage, and cauliflower
- Fatty foods
- Dairy products, if you’re lactose intolerant
- Caffeinated drinks
- Alcohol
- Spicy foods
-
Your ulcerative colitis symptoms might change as you age, but they don’t always worsen, especially if you’ve found a treatment plan that works for you.
Last medically reviewed October 2025