The best GI expert-recommended foods to eat during an ulcerative colitis flare-up

This article has been medically reviewed by Michael Bass, MD, and Idequiz Paez, RD. It was written by Jennifer Chesak.
Often, nutrition and dietary advice about inflammatory bowel disease (IBD) focuses on what foods to avoid. But you may be wondering about the best foods to eat during a Crohn’s or ulcerative colitis flare-up.
If you’ve got a chronic condition (*raises hand in solidarity!*) you’re likely all-too aware that life when you’re feeling great, or when you’re in remission, is vastly different from life when a flare-up strikes. During a flare, many of us must change parts of our routines, engage in even more self-care, and often change our nutrition plans.
Flare-ups do inevitably occur, despite our best efforts to manage a chronic condition, which—not going to lie—can feel like a full-time job. But flares aren’t our fault. They can simply be part of the disease process.
When a flare does happen, having a plan in place to mitigate symptoms and get you back to feeling better as quickly as possible can be immensely helpful. Part of that plan will likely include adjusting what you eat.
An exact nutrition plan to tame IBD flares doesn’t exist, and what’s well-tolerated during a flare can vary from person to person. However, a few guidelines can help you and your care team craft a flare-friendly diet.
What is IBD?
IBD stands for “inflammatory bowel disease.” This is an umbrella term to describe a group of chronic diseases that affect the gastrointestinal (GI) tract. IBD is thought to result from an interaction between your genes and the environment that triggers an abnormal immune response. The two main types of IBD are ulcerative colitis and Crohn’s disease.
IBD has no cure. However, many people with IBD can manage their symptoms with a combination of medication, nutritional changes, and other proactive steps.
Ulcerative colitis
The most common type of IBD is ulcerative colitis. It causes complete damage to the inner lining of the colon and rectum. Symptoms often include blood or mucus in your stool and an urgent need to move your bowels. People with ulcerative colitis may also experience nutritional deficiencies or malnutrition.
Crohn’s disease
Crohn’s disease can affect any part of your GI tract, from mouth to anus. Crohn’s inflames the intestinal walls, causing damage, and damaged patches can extend to the outer lining. Symptoms range from mouth sores to diarrhea and nutritional deficiencies or malnutrition can also occur.
What are the signs of an IBD flare?
Maybe it’s just me, but when I think of the word “flare,” I picture one of those emergency safety flares you might need if you were fixing a flat on the side of the road in the dark or were lost in the wilderness and signaling for help.
When you’re in a chronic disease flare, your body is sending you a signal. Your symptoms may be worse than usual or may have returned after a time of remission during which you were feeling relatively well.
Your flare symptoms will be different from the next person’s with IBD. The Crohn’s and Colitis Foundation recommends making a list of your specific symptoms the next time you experience a flare. You can share these with your care team so that you can develop a flare plan.
A flare generally indicates the need to get in touch with your care team, change certain aspects of your routine, and switch to your “I’m in a flare” diet or nutrition strategies. Your GI provider can help you address a flare from all angles, which may include working with a registered dietitian to address nutrition.
Foods to avoid during an ulcerative colitis or Crohn’s flare
Megan Koistinen, MS, RD, Lead Registered Dietitian at Oshi Health, recommends eliminating GI-stimulating foods when you’re in a flare.
“This is where a GI dietitian can play a vital role,” she says. “Your dietitian will work to help you identify your specific triggers as well as help to tailor your diet to ensure you are meeting both your macronutrient and micronutrient needs in combination with the proper fiber and fluid balance.”
Every person is different and will require different interventions, she adds. However, some triggers are relatively common among people with IBD. So here’s what to temporarily skip in your diet. Remember; These are general guidelines, and you should discuss any dietary changes with your care team.
Avoid high-fiber foods
Fiber is considered good for the general population, but during an IBD flare, it may be a frenemy you can’t trust. Koistinen recommends reducing fiber and steering clear of higher-roughage foods.
“When the rougher fibers—generally the insoluble fiber, such as those found in raw fruits and vegetables—make their way to the colon,” she says, “they are still intact and can be irritating and painful in areas that are already inflamed.”
Avoid foods with rough textures
Some foods can be irritating because of their size and texture. So ditch the popcorn, corn, nuts, and seeds if you find that these exacerbate your symptoms during a flare.
Avoid dairy
For some people with IBD, dairy can worsen a flare, Koistinen says. This is likely because of a correlation between IBD and lactose intolerance.
IBD doesn’t make you lactose intolerant. However, research from 2020 shows that people with IBD have nearly three times the risk of being lactose intolerant when compared to people without IBD.
Avoid spicy foods
Spicy foods can certainly add some fun to your diet. But they are best avoided if you have IBD, especially during a flare.
In a 2020 survey of more than 300 people with IBD, more than half of participants with ulcerative colitis and more than half of those with Crohn’s reported that spicy foods could lead to relapse for them.
Avoid ultra-processed foods
Ultra-processed foods are typically those that are packaged and loaded with added sugars, processed seed oils, preservatives, and other additives. For these reasons, they can be inflammatory and contribute to IBD symptoms.
Ultra-processed foods are associated with an increased incidence of Crohn’s disease and an increased need for IBD-related surgery, according to 2023 research. And research from 2024 suggests that eliminating these foods from the diet may help minimize symptoms of those with ulcerative colitis.
Avoid FODMAPS
In some cases, a low FODMAP diet may be helpful in the short term. This is a diet that reduces intake of fermentable oligosaccharides, disaccharides, monosaccharides and polyols—hence the acronym.
FODMAPs are fibers and sugars that can cause GI tract irritation. Temporarily minimizing intake of these foods might help lessen discomfort during a flare, but the Crohn’s and Colitis Foundation says that such a diet hasn’t been shown to reduce IBD inflammation.
Working with a GI dietitian can help you determine whether temporarily avoiding FODMAPs is appropriate for you.
Avoid caffeine
Research is still on the fence as to whether caffeine may be beneficial or harmful for people with IBD. However, many people with IBD report that coffee has a negative effect on their symptoms.
If this is the case for you, avoid caffeinated beverages, including coffee, tea, soda, and more, as well as caffeine-containing foods such as chocolate.
Avoid alcohol
Alcohol can disturb the gut microbiome, which refers to the fungi and bacteria that take up residence in your GI tract. Beer, wine, and spirits can also disrupt the protective intestinal barrier and lead to intestinal inflammation.
Researchers also report that alcohol can impact the metabolism of some medications you may take for the management of IBD. This could affect how well they work.
Foods to eat during an IBD flare
When a flare strikes, your focus might wholly be on what to avoid, leaving you feeling like you’ll be staring down an empty plate at mealtime. But you can switch your focus to foods that are gentle on your GI tract and methods of cooking and food prep that also help.
Once your flare resolves, you will likely be able to transition back to the nutrition plan you typically follow when in remission. So hang in there.
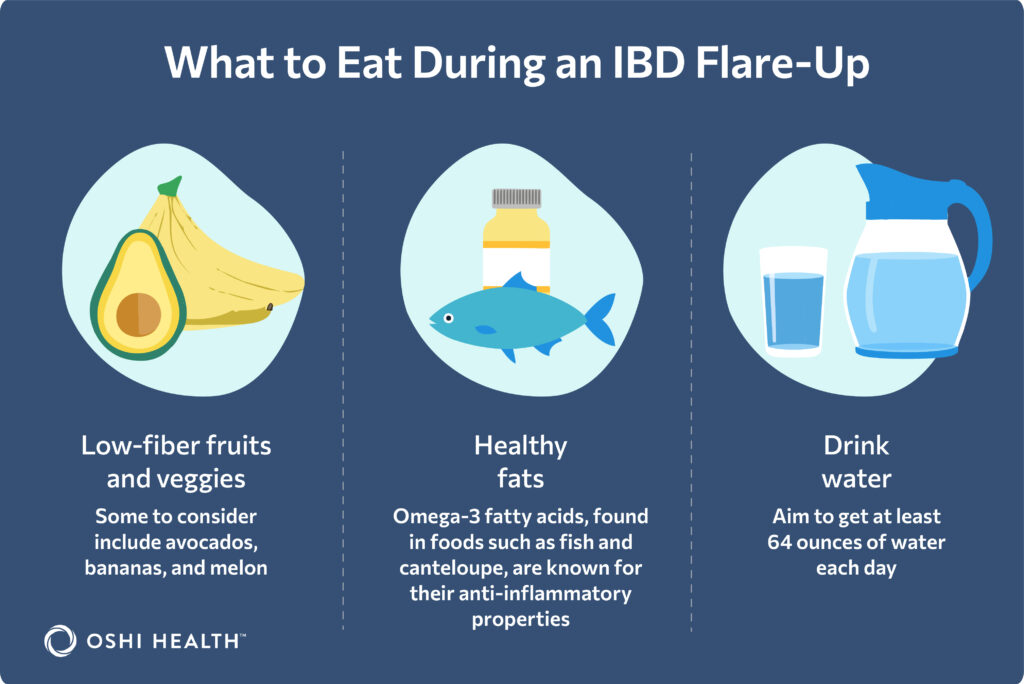
Eat soft, soluble fiber sources
“Often a low-fiber diet is recommended,” Koistinen says. “However this may not be the most beneficial, especially if you are seeing fluctuations in your typical bowel patterns. There are times we recommend a diet with more soluble fibers that tend to be softer.”
Some to consider include avocados, bananas, cantaloupe, and melon. Likewise, you can make some foods softer during the cooking process, such as potatoes and squash.
“Depending on the severity of symptoms or dietary preference,” Koistinen says, “we may also recommend pureeing or blending foods to further break down the fibers that can be irritating.”
Smoothies and pureed soups can still pack in fiber and other nutrients during a flare, and they may be required when a flare is particularly bad.
“In more extreme flares,” Koistinen says, “a fully liquid diet for a week or so may prove to be the most beneficial. This further highlights the need to work with a specially trained GI registered dietitian to help tailor the diet to the individual.”
Eat healthy fats
While avoiding a high-fat diet can be beneficial during an IBD flare, some healthy fats can be super helpful. Omega-3 fatty acids are known for their anti-inflammatory properties.
Some research shows these tend to reduce intestinal inflammation in people with ulcerative colitis and Crohn’s disease. Fish, such as salmon, mackerel, sardines, mussels, and more are high in omega-3s.
As a bonus, omega-3s are abundant in the Mediterranean diet. “A Mediterranean diet is also often recommended,” Koistinen says, “as this has shown promising results in helping to reduce inflammation. However all components of a Mediterranean diet may not be tolerated until individuals have moved out of a flare.”
Your GI registered dietitian can help you craft a Mediterranean diet nutrition plan that works for you when you’re experiencing symptoms.
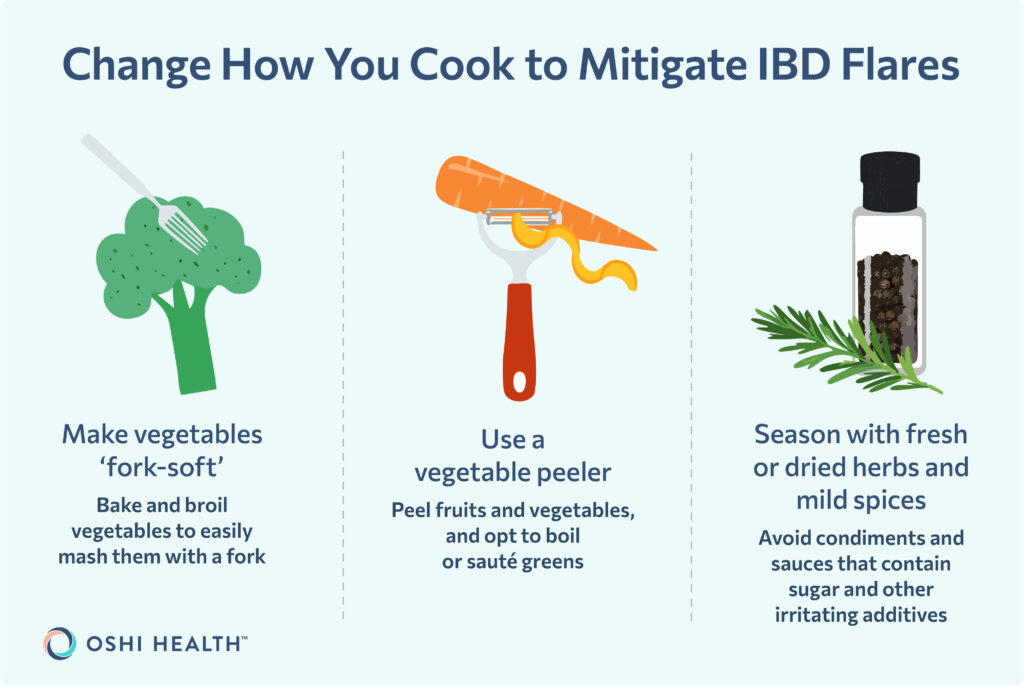
Change how you cook
In addition to changing what you eat, you might be able to lessen flare symptoms by changing cooking methods.
“We recommend cooking methods that will make vegetables ‘fork-soft,’ meaning you can easily mash it with a fork, after cooking,” Koistinen says. For this reason, baking and broiling might be your best options.
“Dietitians are typically hesitant to recommend strictly avoiding foods,” she adds. “However during times of a flare, it is a good idea to be cautious of things like the skins of fruits and raw green leafy vegetables.” So a vegetable peeler can be your friend, and you can opt to boil or sauté greens.
How you flavor your food during a flare may also matter. Consider fresh or dried herbs and mild spices in lieu of condiments and sauces, which may contain sugar and other irritating additives.
Drink water
When you’re experiencing an IBD flare, you’re at risk of becoming dehydrated, so it’s important to drink lots of water.
Aim to get at least 64 ounces of water each day. You know you’re well-hydrated by checking the color of your urine. It should be light yellow. If it’s very dark or yellow, that may be a sign you need to drink more water. But keep in mind that some supplements can alter urine color.
Consider caloric intake
Some people with IBD have increased caloric requirements. During a flare, symptoms like nausea can reduce your appetite, and when you’re dealing with diarrhea, you may shy away from eating to make it stop.
However, avoiding food altogether increases your risk of malnutrition—and if your body isn’t getting the nutrients it needs to function, it will have a harder time healing from a flare.
Your GI registered dietitian can help make sure you are getting all the nutrients your body needs for proper healing and health during a flare as well as in remission.
Diet is only one part of the equation
“Diet alone will not help you navigate a flare,” Koistinen says. Minimizing stress is also crucial, since stress can play a role in IBD exacerbations. This is because our brains and guts are intricately connected via the gut-brain axis. Medical management is also important when treating an IBD flare, and you can find out more about your care options below.
“Oshi Health made me feel like I had a whole team behind me. I now feel more equipped to handle medical, mental health, and diet decisions than ever before.”
—C.P., living with ulcerative colitis
FAQ
What foods should you eat during an ulcerative colitis flare up?
What works for you during a flare may be different than what works for someone else. Above are some common foods and food-prep tips that may help mitigate symptoms. But talking to a GI registered dietitian is best. They can develop a plan that is customized to your unique needs and tastes.
What foods soothe inflamed intestines?
If you’re experiencing an intense flare, sometimes a temporary liquid diet of smoothies and pureed soups may be necessary. But this is best done under the guidance of a GI registered dietitian to ensure adequate nutrition to help your body heal the flare.
How do you settle an ulcerative colitis flare up?
Settling an ulcerative colitis or Crohn’s flare may involve temporarily changing your diet to one that is less irritating. Some common triggers and go-to foods are listed above. Plus, we’ve included what to eat during a flare.
What are the worst foods to eat if you have ulcerative colitis?
When you’re in the middle of an IBD flare, some common trigger foods include those that are processed, fried, sugary, or spicy. Additionally, sometimes raw fruits and vegetables and other foods that are high in fiber may be too irritating. Rough-textured foods, such as nuts and seeds, may also cause trouble. Likewise, dairy, caffeine, and alcohol can worsen symptoms as well.
What foods should you eat when ulcerative colitis is in remission?
When your IBD is in remission, you can typically return to your usual healthy diet. However, you’ll want to continue to avoid foods that are known flare triggers for you. Working with a GI registered dietitian can help you determine what those are and how to maintain optimal nutrition, whether you’re in a flare or remission.
Should I follow a low-fiber diet during an ulcerative colitis flare?
In many cases, high-fiber foods can be too irritating during a flare. But fiber is still an important nutrient, and you might find that low-fiber fruits and veggies are tolerable. Consider items like banana, cantaloupe, squash, potato and sweet potato, and more.
Takeaway
At Oshi, we understand that no matter how much we do our best to take care of ourselves, flares from chronic conditions, including IBD, can show up. That’s why having a flare plan in place can be beneficial. Such a plan may involve changes to your diet.
Switching to a gentle diet that is less GI-stimulating can help mitigate symptoms and support healing so that you can get back to feeling better.
Oshi Health offers a comprehensive care plan. Your gastroenterologist and GI registered dietitian can help you tailor a treatment and nutrition plan that works for you while you’re in remission to lessen the chance of flares and create a plan that best supports your health during a flare.