Part of a treatment plan for gastroesophageal reflux disease (aka GERD) may include a specialized GERD diet to reduce exposure to trigger foods and increase intake of foods that promote a healthy gastrointestinal (GI tract). A GI Registered dietitian can help you develop a GERD diet plan that’s customized to your unique needs.
If you’ve got gastroesophageal reflux disease, commonly called GERD, a gastrointestinal (GI) registered dietitian can help you craft a GERD diet plan that prevents and alleviates symptoms.
Changing my diet and lifestyle has certainly helped me. Suddenly in my 20s, I began experiencing symptoms of GERD. I was lying in bed one night and felt a burning sensation in my throat and had difficulty swallowing and trouble breathing.
I thought my asthma was acting up. So I went to see my pulmonologist who examined me and told me I had GERD, which was triggering an asthma exacerbation. I was a bit surprised, since I’d never experienced the situation before. My next steps involved researching GERD and figuring out a plan to control my symptoms. I underwent a bit of trial and error before finally landing on a plan that works for me.
However, you can find relief faster with the help of a care team that may include a gastroenterologist, GI registered dietitian, gut-brain specialist, and more. Your care team will consider your specific symptoms, lifestyle, diet, any current medications, and other factors unique to you.
GERD is decidedly not fun, so finding a treatment plan sooner rather than later can help you ditch the burn and other potential symptoms. Plus, a treatment plan will help you protect the delicate tissues of your upper GI tract from damage.
Understanding gastroesophageal reflux disease (GERD)
What’s the difference between heartburn, acid reflux, and GERD? The first thing to understanding GERD is grasping the general terminology, which can be a little confusing.
“Heartburn is a symptom of acid reflux, when stomach acid travels up into the esophagus, often characterized by chest pain or burning,” says Brianna Olivieri, MS, RD, a GI registered dietitian with Oshi Health.
GERD, however, is a chronic gastrointestinal condition with frequent acid reflux over a long period of time. It may or may not include heartburn as a symptom. If you have GERD, the contents of your stomach backflow into your esophagus, aka your “food pipe.”
The lower esophageal sphincter is a valve that separates your esophagus from your stomach. This valve manages the downward flow of food and drink through your upper GI tract, and GERD is a signal that the valve isn’t doing its job properly. Your stomach’s contents include acid, so reflux can irritate the lining of your esophagus, leading to the characteristically uncomfortable symptoms.
Common symptoms of GERD
- Coughing
- Difficulty swallowing
- Heartburn
- Lump in the back of the throat
- Regurgitation of food or liquid
Less obvious symptoms
- Asthma exacerbations
- Bad taste in mouth
- Chest pain
- Dental erosions
- Laryngitis or hoarseness
- Nausea or vomiting
- Stomach pain
- Wheezing
GERD affects about 20% of the population in the United States, making it one of the most common digestive disorders. So you’re certainly not alone if you’re experiencing it.
Diagnosing and managing GERD
Now that you know the nitty-gritty details of what GERD is, you might be wondering how to get an official diagnosis and how to treat GERD.
How GERD is diagnosed
GERD can often be diagnosed just based on your symptoms, which limits unnecessary or invasive testing. But your care team may request that you undergo some tests, depending on various factors. For example, your clinician may want to check for esophageal damage.
“GERD may be diagnosed with an Also known as an upper endoscopy (or EGD for short), an esophagogastroduodenoscopy is a procedure used to diagnose and treat problems in your upper GI (gastrointestinal) tract, which includes your food pipe (esophagus), stomach, and the first part of your small intestine (the duodenum). (EGD),” Olivieri says, “which can identify possible damage to the esophagus or stomach lining that may have been caused by GERD.”
An EGD, also called an upper endoscopy, is a procedure to help your doctor look at your GI tract. Your physician will pass a flexible tube with a tiny camera attached through your mouth and down your throat. Other tests can also help diagnose or rule out GERD.
Testing for GERD
In addition to an EGD, other tests for GERD include:
- Ambulatory pH monitoring
- Esophagram
- Esophageal manometry
How GERD is managed
You can often manage GERD with dietary and lifestyle changes. Your care team can help you determine your GERD trigger foods and any lifestyle habits that can worsen GERD, such as late-night dinners or your sleeping position. The team can work with you to create a management plan.
Complications of GERD if left untreated
Acid by its nature is corrosive, meaning it can cause damage. So you can imagine how all that stomach acid in the wrong place can wreak havoc on your throat, esophagus, and tooth enamel.
“Frequent reflux of acid into the esophagus can cause esophagitis,” Olivieri says, “which is inflammation of the esophagus. The symptoms of this may include sore throat or hoarse voice on top of other preexisting reflux symptoms. Esophageal ulcers or an esophageal stricture may even occur.” A stricture means the esophagus is narrowed, causing difficulty swallowing.
People with chronic GERD do have a small increased risk of developing esophageal cancer over time, according to the American Cancer Society. However, most people who have GERD do not develop esophageal cancer.
Another concern with untreated GERD is the development of Barrett’s esophagus. This is when tissue that is like your intestinal lining replaces the tissue lining your esophagus. The condition puts people at a higher risk for esophageal cancer.
Untreated GERD, as in my case originally, can also cause bronchospasms, commonly known as asthma attacks. GERD can worsen other lung conditions, such as chronic obstructive pulmonary disease (COPD), as well.
The role of diet in managing GERD
When life gives you literal lemons, sometimes those lemons will give you GERD. That’s my goofy way of saying that what we eat matters for managing GERD. Although I love it, citrus can be a culprit.
“Diet is important when managing GERD,” says Idequiz Paez, RD, a GI registered dietitian with Oshi Health, “because the right dietary modifications can help to greatly reduce symptoms and avoid long-term use of medications, which may have undesired side effects.”
Here, we’ll explore common trigger foods, foods that are typically more GERD friendly, and more.
Foods that trigger GERD symptoms
Don’t despair if you see a favorite food on the below list, like coffee, which is my morning bestie. A GI registered dietitian can often help you figure out ways to enjoy a favorite while mitigating GERD symptoms.
Keep in mind that these are only common triggers, and triggers will be different for everyone, Olivieri says. Large portions of any food can be a trigger as well, Paez adds.
Common GERD trigger foods
- Alcohol
- Carbonated beverages
- Chocolate
- Citrus
- Coffee
- Fried foods
- Garlic
- High-fat foods
- Onion
- Peppermint
- Red sauces or condiments
- Salty foods
- Spicy foods
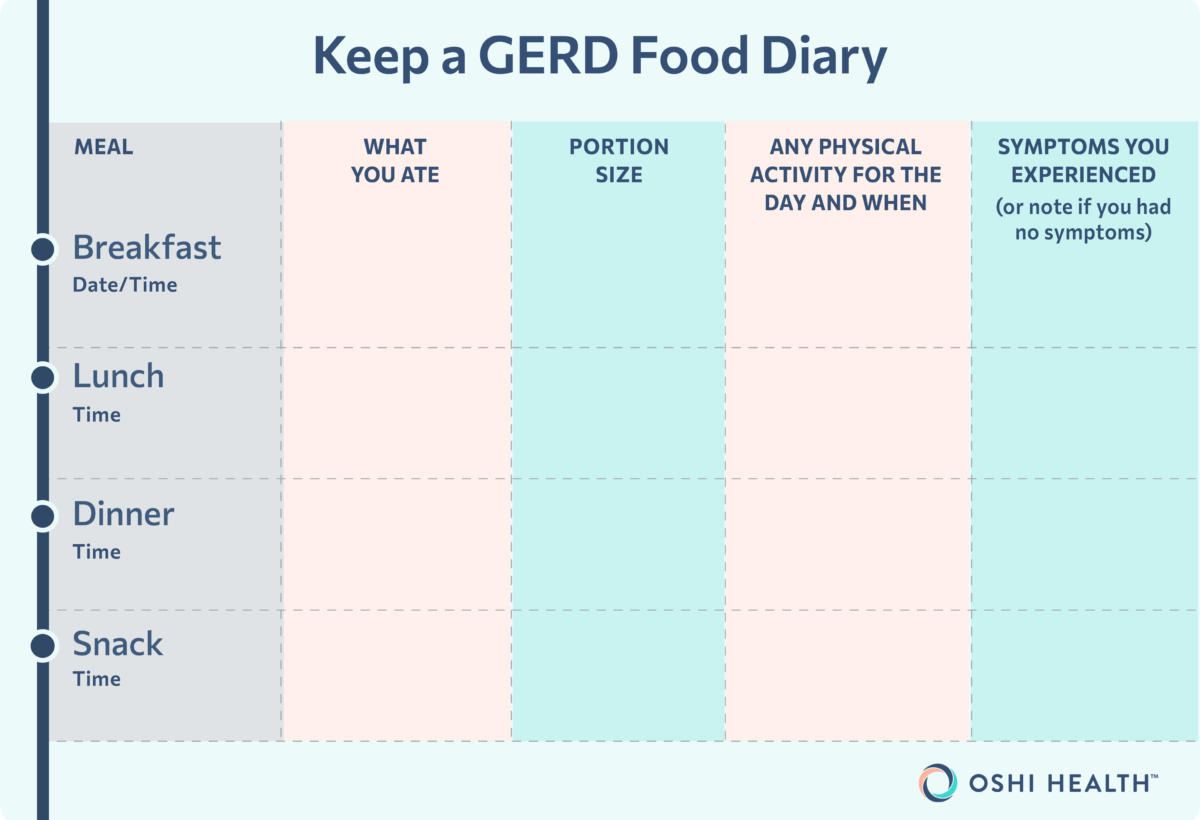
You may wish to keep a food symptom log for a week or more to track trigger foods. Such a log can be helpful for when you see a GI provider.
What to include on your food symptom log
- Day/time
- What you ate
- Portion size
- Any physical activity for the day and when
- Symptoms you experienced (or note if you had no symptoms)
Foods that can help alleviate GERD symptoms
“A GERD-friendly diet may look different for everyone,” Olivieri says. However, some foods may help reduce GERD symptoms or help prevent them.
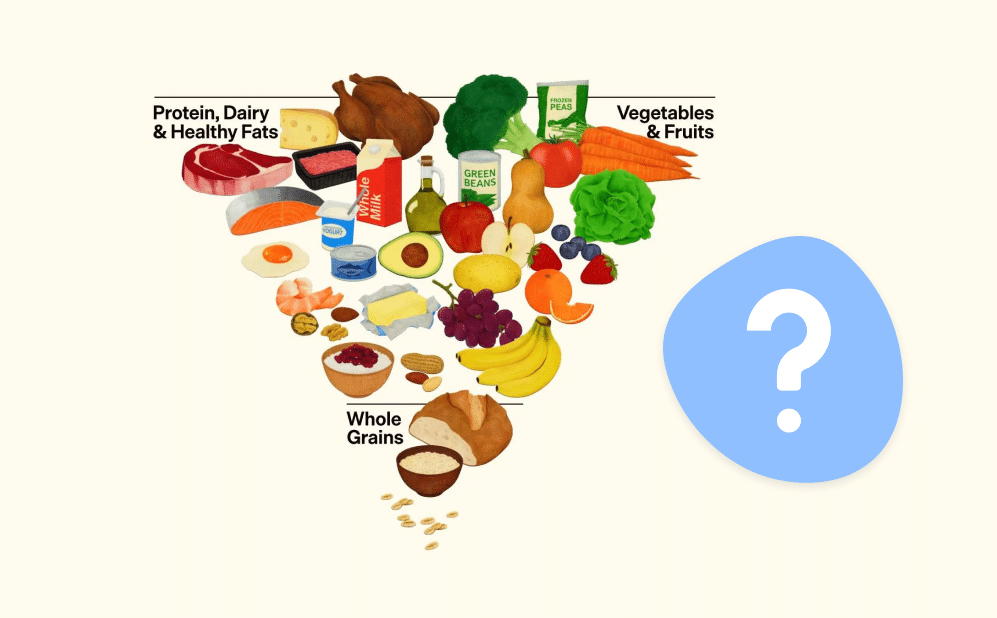
Common GERD-friendly foods
- Fruits (except citrus and tomato)
- Lean protein sources
- Legumes
- Vegetables (except onion, garlic, and spicy peppers)
- Whole grains
This list helps you focus on high-fiber and calcium-rich foods, all of which have been shown to help reduce GERD symptoms.
High-fiber foods. High-fiber foods may aid with digestive motility, or movement. Improved motility helps to reduce the pressure on the esophageal sphincter, decrease reflux, and lessen some symptoms. Consider adding more whole grains and root or green vegetables to your diet.
Meet Oshi's GI registered dietitians
Find relief—and stay nourished
When you work with an Oshi GI registered dietitians (RD), you’ll get personalized nutrition guidance, including help with finding and avoiding potential food triggers, choosing gut-friendly supplements and recipes, and more.
Dining out with GERD
If you’ve got GERD, dining out can feel a bit tricky. But you’ve got options. Again, your trigger foods will be different than the next person’s. But here are few foods that are generally considered to be GERD friendly.
GERD-friendly foods for dining out
- Grilled rather than fried foods
- Lean meats, fish, and white poultry
- Steamed rather than fried or sautéed veggies
- Clear broth-based soups, rather than creamy or tomato-based versions
Modified GERD diet and alternative options
One diet that may help ease GERD symptoms is the Mediterranean diet. This diet is based on a high intake of fruits, veggies, and whole grains, and moderate intake of lean sources of protein, all of which tend to be GERD friendly. Some research shows that people who eat a Mediterranean diet report a reduction in GERD symptoms.
Lifestyle changes that can help manage GERD
In addition to modifying your diet, some lifestyle changes can help you manage GERD. What works for you may be different from what works for someone else, but here are a few to consider.
Eat at least three hours before lying down
In studies, those who report longer intervals between eating and lying down report fewer GERD symptoms. Lying down soon after a meal can cause reflux. Try eating dinner at least three hours before bedtime to lessen the chances of the contents of your stomach traveling the wrong way, which could also interfere with your sleep.
Sleep with your head elevated at night
When you do go to bed, elevating your head slightly may help. You can do this using pillows or by buying a specially designed wedge to go under your mattress that provides a natural and comfortable rise.
Eat smaller meals
You may need to eat smaller, more frequent meals throughout the day to combat GERD. Keeping your portions small may help to reduce stomach pressure. Pressure can exacerbate GERD symptoms.
Avoid tight-fitting clothing
If you need an excuse to wear your comfy pants, here’s one. Tight belts, waistbands, and more can all contribute to GERD by increasing abdominal pressure, especially after a meal. So stick to looser styles as much as possible. This tip has been a game-changer for me.
Avoid tobacco and alcohol use
If you smoke or use other tobacco products, quitting will likely alleviate some of your GERD symptoms. Tobacco can have a negative effect on saliva production. Saliva is rich in bicarbonate, which can help neutralize and clear acid.
Also try reducing or eliminating alcohol consumption. Alcohol can harm the delicate mucosal lining of your esophagus, increasing your risk for GERD damage.
Maintain a healthy weight for you
Having obesity is a risk factor for the development of GERD. This is because obesity can impair the motility of food through the GI tract, cause dysfunction of the esophageal sphincter, and increase intragastric pressure. Obesity is a complex chronic condition that may require more than just lifestyle changes to treat. Working with an obesity medicine specialist may be helpful.
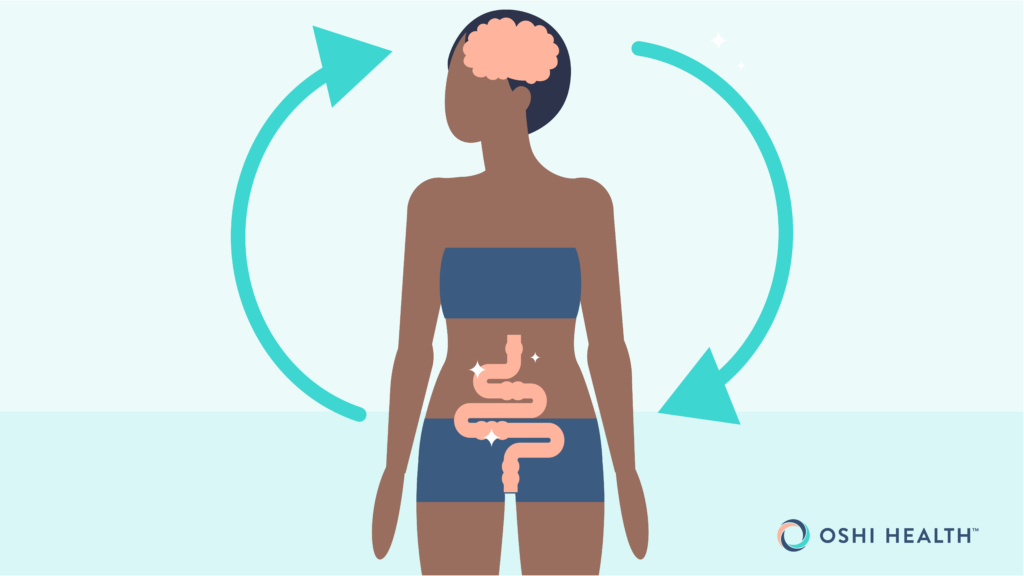
Work on your gut-brain connection
The brain and the gut are connected via what’s called the gut-brain axis. This means that stress, anxiety, depression, and more may also be a factor leading to worsened GERD symptoms.
“Many people also suffer stress from the long-term impact of having had adverse childhood experiences (ACEs),” says David D. Clarke, MD, a board-certified gastroenterologist and president of the Psychophysiologic Disorders Association.
“ACEs can cause the development of stressful personality traits, triggers in your present-day life, and unrecognized but powerful negative emotions,” he adds. “Stress from these issues is a common cause of burning chest pain even in the absence of GERD.”
ACEs change the body’s natural stress response and may cause visceral hypersensitivity, which is when the usual functioning of your organs causes unexplained pain. Some people experiencing reflux may have reflux hypersensitivity. In these cases, a person may experience GERD symptoms, such as heartburn, but they have normal test results. Working on your gut-brain connection with a GI psychologist can help.
FAQ
-
Foods that are GERD-friendly to you may trigger someone else. In general, however, sticking to high-fiber foods can help.
-
Common GERD-trigger foods include alcohol, carbonated beverages, chocolate, citrus, coffee, garlic, onion, peppermint, red sauces or condiments, and fried, high-fat, salty, and spicy foods.
-
In research, eggs have been reported as a trigger food, but they’ve also been reported to lessen symptoms of GERD. The best way to tell if eggs are a trigger for you is to test them out and keep a food log regarding other triggers.
-
Acid reflux is when the contents of your stomach backflow into your esophagus. Heartburn is a symptom of acid reflux. Gastroesophageal reflux disease (GERD) is a chronic condition characterized by reflux.
When should I see a doctor about GERD?
If you’re experiencing the symptoms listed in this article, you should see a clinician for an evaluation. If you do have GERD, treating it early can help protect the delicate tissue of your esophagus.
As in my case, a breathing issue was a reason to talk to a doctor. If you are experiencing unexplained coughing or worsening symptoms of asthma or another lung condition, seek medical attention.
Managing GERD symptoms may include changes to your diet and lifestyle. Working with a comprehensive GI team, like you’ll find at Oshi Health, can help. Oshi’s practitioners can help you determine the best approach to treating and managing GERD. Your care plan may include medication, dietary or lifestyle changes, gut-brain support, and more, based on your unique circumstances.
“Oshi’s registered dietitians can help individuals determine likely symptom triggers and come up with a plan for any dietary adjustments that may help to improve symptoms,” Olivieri explains. “Oshi’s RDs will work with individuals to determine a plan that works for their lifestyle and dietary preferences.” Your preferences may include foods typically enjoyed in your culture or region.
Finally, Oshi’s gut-brain specialists can teach you tools that may help to reduce stress and other triggers to help manage GERD symptoms. Imagine a life without constant GERD symptoms. A team approach to your care sets you up for the best results, making fewer symptoms a reality.
Oshi is your partner in digestive health
Feel like your digestive concerns are running your life? You’re not alone—and we’re here to help you find lasting relief.
Oshi Health GI providers, gut-brain specialists, and registered dietitians work together to address your symptoms and find solutions that actually work for you.
Whether you’re dealing with chronic digestive issues or unpredictable symptom flare-ups, our GI specialists deliver:
✔ Personalized care plans tailored to your lifestyle
✔ Science-backed strategies to calm your gut
✔ Compassionate, whole-person care
✔ And so much more!
Ready to take control of your gut health?