Your stomach and back can hurt at the same time, for many reasons, and women may be especially likely to experience both types of pain simultaneously. Five common causes include: gastrointestinal (GI) issues like bloating or constipation, gallbladder issues, kidney stones or infection, pancreatitis, and menstrual cycle or hormonal changes.
When both back and abdominal pain strike, you might wonder what’s up. Did you tweak your spine? Is it a gut health issue? And if you’re assigned female at birth, you might point a suspicious finger at your menstrual cycle.
Some digestive diseases are more prevalent in females. Plus, a significant portion of female reproductive organs are internal, much more so than male reproductive organs. Both of these factors can make pinpointing the exact source of your pain a bit more complicated without the help of a knowledgeable healthcare provider.
Understanding common causes of co-occurring stomach and back pain can help you advocate for the care you need. If a doctor discounts your discomfort or other symptoms, seeking a second opinion is a great idea.
5 reasons women experience stomach and back pain together
1. GI issues such as bloating, gas, and constipation
Research suggests that people assigned female at birth who have two or three gastrointestinal symptoms—constipation, bloating, and gas, for example—are three times more likely to experience back pain.
There are a few potential mechanisms that can cause this. One is referred pain (when you feel discomfort in an area that’s not the source of the issue). Others are increased spinal loading from straining on the toilet, and/or issues with your abdominal muscle function. Straining involves the Valsalva maneuver, forced exhalation against a closed airway. This increases intra-abdominal and intrathoracic pressure, placing added pressure on the spine. Gas and bloating may also lead to tissue compression that causes pain.
Bloating, gas, and constipation are common features of irritable bowel syndrome with constipation (IBS-C), which is more prevalent in females.
The fix: A knowledgeable GI provider can help determine the causes of your symptoms. They can also address any dietary triggers and encourage lifestyle changes as needed. Increased walking can work wonders for gut motility, as can strategies for proper toileting positioning (and helpful tools such as a Squatty Potty). Your provider will also suggest tips to improve the communication route between your gut and brain—all of which will work to relieve constipation, gas, and bloating.
Experts in all GI symptoms and conditions
Care tailored to you, not just your symptoms

2. Gallbladder issues
Your gallbladder is located under your liver in your upper right abdomen. It stores bile, which breaks down fats to aid with digestion, and then releases it through various ducts. One gallbladder problem that can happen is developing gallstones, which are hardened deposits. Gallstones can cause blockage of the gallbladder outlet. Common symptoms of this include nausea and sharp pain in the upper-right area of your abdomen, which can radiate to your side and back.
Gallstones affect the female body at three times the rate of the male body. That’s likely due to the impact of female sex hormones (including changes during pregnancy and postpartum), especially estrogen, which increases the cholesterol content in bile. You may be more at risk for gallstones if you use hormone replacement therapy to alleviate menopause symptoms or take oral contraceptives.
The fix: Treatment for gallbladder issues will depend on factors unique to you. Some people need a cholecystectomy—surgery to remove the gallbladder. You may also need to make some dietary changes, such as reducing certain types of fat, as part of your treatment plan. Either way, the recommendations you receive from your healthcare provider should be tailored to you, your body, and your lifestyle. Many gallstones are also completely asymptomatic and often need no treatment.
3. Pancreatitis
Pancreatitis is inflammation of the pancreas. What’s that, you ask? The pancreas is a gland that sits just behind the stomach; it aids your digestion and blood sugar regulation. The main symptom of pancreatitis is intense upper abdominal pain that may radiate to your back. You may also experience fever, rapid heart rate, nausea and vomiting, and/or jaundice (yellow skin).
The top causes of pancreatitis include heavy alcohol consumption, gallstones, and hypertriglyceridemia, a condition where you have high levels of a certain type of fat in your bloodstream. Some medications can also affect the pancreas. And, while males are more likely to develop alcohol-related pancreatitis, females tend to develop the condition as a complication from gallstones.
When a gallstone blocks your bile duct, it prevents pancreatic enzymes from reaching your small intestine. This leads to an overload of enzymes in your pancreas, which can inflame the gland.
The fix: If you suspect pancreatitis, you should seek medical attention. Most cases of acute pancreatitis necessitate IV fluids, pain medication, and nutrition therapy (if you can’t keep foods down) in the hospital. Your provider will also recommend individualized dietary changes for management in the long term.
4. Kidney stones or infections
Kidney stones result from high levels of oxalate, phosphorus, and calcium in your urine. They then form into hard deposits that are anything but comfortable. Your diet can play a role in whether these baddies are going to form. When these small deposits enter your ureter (the tube that carries urine from the kidney to the bladder) and make their way toward your bladder, they typically cause pain, and can cause other issues too.
These are some types of pain that may be a red flag you’re experiencing kidney stones: sharp pain below the ribs on your side or your back, pain that spreads across the pelvic area or groin, pain or burning with urination. Other symptoms of the stones include: red or brown urine, cloudy or foul-smelling urine, fever and chills, and nausea or vomiting.
Another kidney issue that can cause both stomach and back pain is a kidney infection (pyelonephritis). A kidney infection is a type of urinary tract infection (UTI)—something many women know far too well. Infections that begin in the urethra can travel to one or both of your kidneys. This can cause uncomfortable symptoms, including: pelvic and back pain, fever and chills, burning or pain during urination, frequent urination, blood or pus in the urine, foul-smelling or cloudy urine, and more.
Although kidney stones are more common in males, their prevalence is increasing in females. Kidney infections are actually more prevalent in the female body, though. That’s because our urethras tend to be shorter and located closer to the anus, making the migration of bacteria easier.
The fix: Treatment for kidney stones involves staying hydrated, taking medications that help dissolve the stone to make it easier to pass, taking pain medications as needed, and more. In some cases, procedures may be required to help remove or dissolve stones. Treatment for a kidney infection will require a course of antibiotics.
5. Menstrual and hormonal triggers
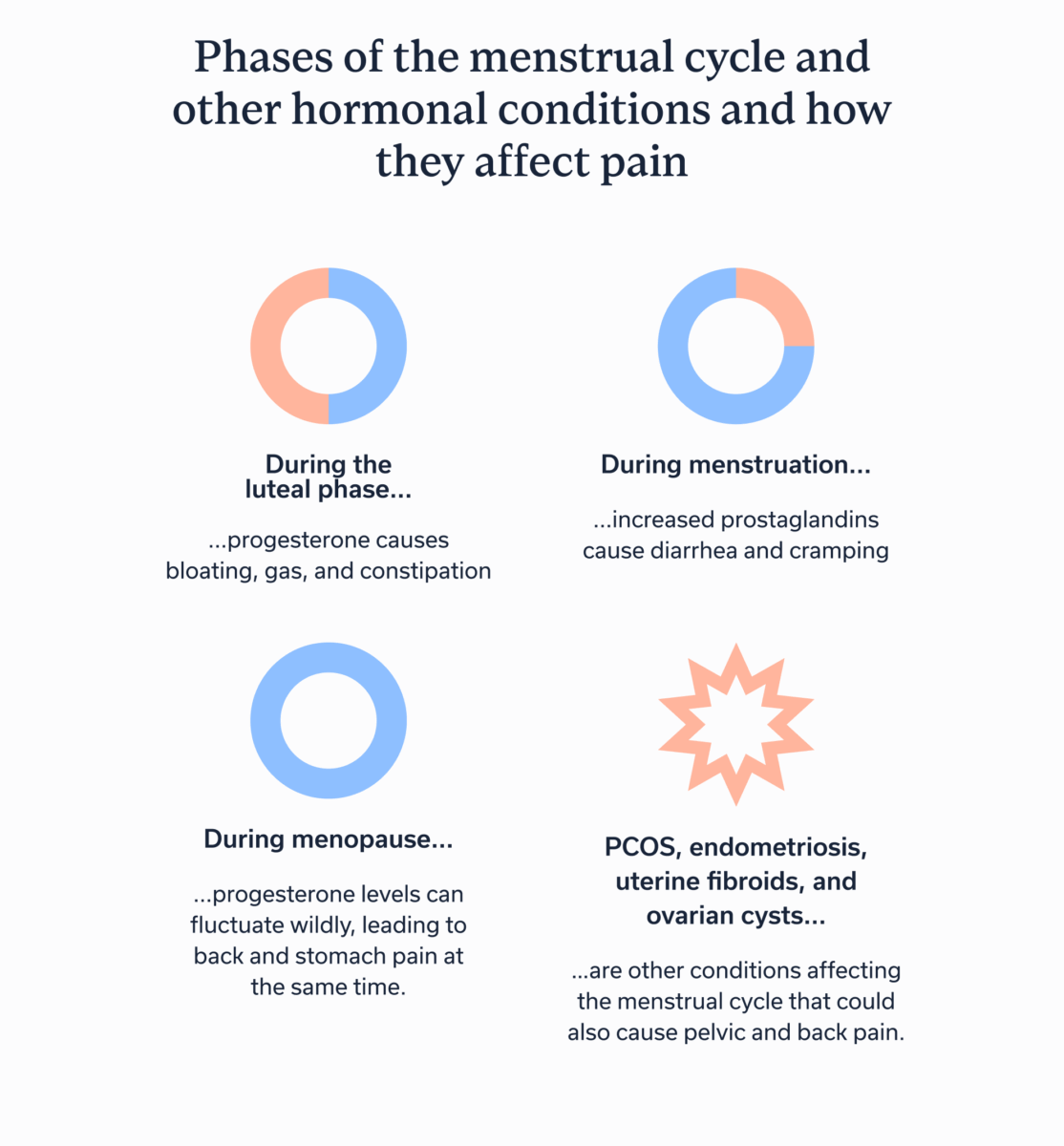
Your menstrual cycle—or hormonal changes due to the menopause transition—may be a culprit behind co-occurring abdominal and back pain. Both types of pain are symptoms of premenstrual syndrome and dysmenorrhea (painful periods).
Progesterone rises during the second half of your menstrual cycle (known as the luteal phase). This hormone is a common cause of bloating, gas, and constipation. Then, when you get your period, or just beforehand, you may experience diarrhea (which can also cause cramping) as a result of increased prostaglandins. Those are the helpful lipids that produce contractions to help expel the endometrium, aka period blood. These bowel changes may also cause abdominal and back discomfort at the same time, and you might also experience cramping from uterine contractions.
Progesterone levels can also fluctuate wildly during the menopause transition, leading to back and stomach pain at the same time. An unfortunate “bonus”? Female hormones tend to decline the closer you are to menopause, which can increase joint pain and lower your overall pain threshold.
Other conditions affecting the menstrual cycle could also cause pelvic and back pain. These include polycystic ovary syndrome (PCOS), endometriosis, uterine fibroids, and ovarian cysts.
Finally, sacroiliac (SI) joint and pelvic floor dysfunction are common causes of low-back and abdominal pain. Hormonal shifts from menstruation and menopause can exacerbate these issues by altering pain signals, ligament function, and more.
The fix: The solution for relief will depend on the underlying cause of your pelvic and back pain. The important thing: If you are experiencing painful periods, pain at other times during your cycle, or extreme pelvic or back pain for any reason, you should consult a healthcare provider. Although society tends to normalize period pain, intense pain is not normal, and you deserve relief.
Other non-digestive possibilities
Of course, back pain can result from issues that aren’t related to your digestive tract or reproductive organs. For example, muscle strains or sprains, posture, arthritis, disc herniation or degeneration, and more, can also cause discomfort.
When to see a clinician
You should consult with a clinician if you have ongoing back or abdominal pain that doesn’t resolve with at-home care. You should seek emergency medical attention for severe abdominal or back pain, whenever you notice blood in your urine or stool, or if you have an unexplained fever, which could signal an infection.
Key takeaways
- Stomach and back pain may occur together because of digestive issues, hormonal issues, or both.
- Those assigned female at birth may be more at risk for experiencing dual pelvic and spinal discomfort for various reasons.
- If you are experiencing abdominal and back pain, or one or the other, you should consult with a healthcare provider who can help you get to the root cause.
- Reach out to Oshi Health for a consultation.
FAQ
-
As discussed above, your stomach and back can hurt at the same time for numerous reasons. Common causes include bloating or constipation, gallbladder issues, kidney stones or infection, pancreatitis, and menstrual cycle or hormonal changes.
-
Common causes include those mentioned above, such as bloating or constipation, gallbladder issues, kidney stones or infection, pancreatitis, and menstrual cycle or hormonal changes. However, other possibilities include PCOS, endometriosis, uterine fibroids, and complications from an ovarian cyst. If you have intense stomach or back pain or this is an ongoing issue, be sure to consult a healthcare provider.
-
You should seek emergency medical attention for severe abdominal or back pain, whenever you notice blood in your urine or stool, or if you have an unexplained fever, which could signal an infection.
-
Pain from pancreatitis often feels like a dull, but intense, ache in the upper abdomen just below the ribs. However, this type of pain can also radiate to other areas, including the side, back, or even the shoulder blade.
Personalized care for the whole you
Did you know women are more likely to experience gastrointestinal (GI) symptoms and conditions than men? That’s because hormones and reproductive health have a major impact on the gut-brain connection—and vice versa!
At Oshi Health, we work with you to understand your unique situation, including how your cycle might impact your GI symptoms. Our goal is to create a personalized care plan that fits your lifestyle.
Here’s what you’ll get:
✔ A personalized care plan tailored to you
✔ Nutrition guidance rooted in scientific research
✔ Proven techniques to calm your gut and ease discomfort
✔ Compassionate, whole-person care
✔ And so much more!
Ready to find lasting symptom relief?