There isn’t one exact best diet for people with ulcerative colitis: foods that help or hinder your condition will be unique to you, and may differ during your flares vs. periods of remission. But while the “right diet” varies, there are some helpful general guidelines about what to eat (and what to avoid) when living with this chronic gut health condition—such as focusing on soothing foods during a flare and following a Mediterranean diet in periods of remission in order to reduce inflammation.
Eating healthy can feel much more confusing than it should be. One website may tell you that eggs are a great source of protein, and another might warn of their high cholesterol. Some people thrive on a plant-based diet, and others become iron deficient. Throw in an ulcerative colitis (UC) diagnosis, and learning what you “should” and “shouldn’t” eat becomes even harder.
While there’s no single ulcerative colitis diet, there are foods that tend to work better for people during UC flares vs. periods of remission. The invaluable skill here? Learning what foods you can tolerate well and how to adjust your diet depending on your symptom severity, all while staying well-nourished. This skill will serve you and your unique UC needs—even though the “right diet” for you will likely be very different from your neighbor’s.
Understanding ulcerative colitis
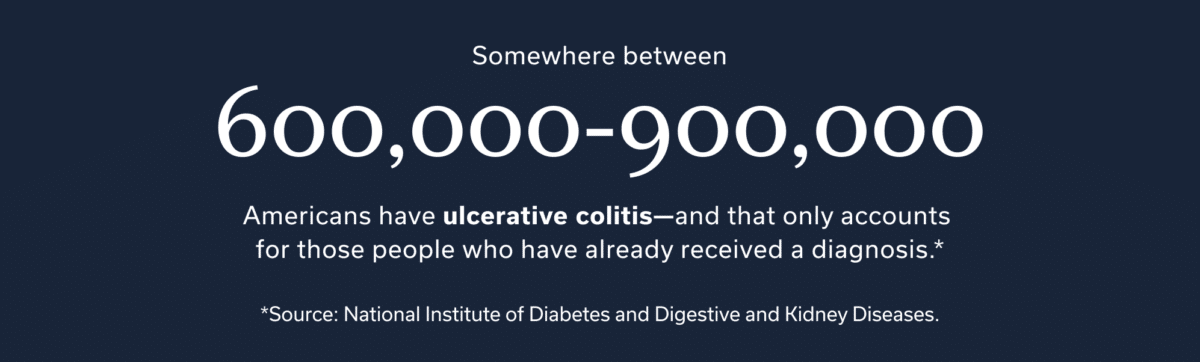
Somewhere between 600,000 to 900,000 Americans have ulcerative colitis—and that only accounts for those people who have already received a diagnosis! But while UC is a common inflammatory bowel disease (IBD), it’s not often talked about outside the IBD community. How about a quick refresher, then?
UC occurs when an abnormal immune system reaction causes ulcers and inflammation on the inner lining of the large intestine. These ulcers and inflammation can put quite a strain on your comfort level—and disrupt your entire GI system.
Plus, ulcerative colitis is tricky to diagnose, as symptoms can build gradually or start suddenly. The road isn’t clear after a diagnosis either. Instead, it can include both periods of disruptive symptoms (aka flare-ups) as well as days, weeks, or even years of remission.
Ulcerative colitis symptoms
So what exactly are the symptoms of ulcerative colitis? The most common include:
- Abdominal pain or cramping
- Blood in your stool
- Diarrhea
- Fever
- Gurgling sounds in your intestine
- Irritated eyes
- Mucus or pus in your stool
- Nausea
- Rectal bleeding
- Skin ulcers or bumps
- Swollen or painful joints
- Tenesmus (this means a frequent urge to poop, even if your bowels are already empty)
- Weight loss
Not everyone experiences every symptom on this list, and the scarier ones are less common. In fact, about half of individuals with ulcerative colitis only have mild symptoms, like diarrhea or irritated eyes. But while they may be “mild,” considering, these symptoms are not so nice for your overall health—and can interrupt your daily routine and social life.
Dietary recommendations for ulcerative colitis
Maybe it’s just me, but every once in a while, I’ll have a few weeks where I eat extremely healthy, hoping it will solve all my problems (spoiler alert: It never does). Then, life gets busy and I hop off the 100% healthy eating bandwagon and bring back some treats. This two-level tendency is natural, and it may actually help when it comes to managing UC. That’s because UC is marked by flares and periods of remission, which may require different dietary approaches.
As a rule of thumb, we should all strive to eat tasty foods that make us feel good. But feeling good can mean different things—and require different dietary approaches—depending on if you’re experiencing remission or a flare. If navigating this feels overwhelming, working with a registered dietitian—particularly one with experience treating GI conditions—could be helpful.
What to eat during a flare
A flare may be the time to pull a GI gentle diet from your UC toolkit. This diet emphasizes soft-textured food and moderate fiber intake, which can help ease digestive symptoms like cramping, stomach pain, and bloating.
The primary pillars of this way of eating include:
- Consume smaller, more frequent meals throughout the day.
- Get fiber from cooked vegetables, whole grains, and skinless fruit.
- Avoid leafy greens and fruits/veggies that are stringy, have skin, or contain lots of seeds.
- Opt for leaner sources of protein, such as roasted chicken, fish, or scrambled eggs. A UC flare may not be the time to splurge on a steak (or fried meat).
- Choose softer breads over loaves with seeds or ones that are crusty.
- Sub in some liquid meals (think soups and smoothies).
- Get nuts and beans from softer sources (i.e. instead of a handful of almonds, choose some almond butter).
- Adjust your fiber intake to what best suits you—and/or skew toward soluble fiber, which is often better tolerated.
What to eat in periods of remission
Remission is similar to an athlete’s pre-season: It’s the time to establish good habits and create a starting line-up of healthy recipes you enjoy. One effective “pre-season” choice to consider for ulcerative colitis is the Mediterranean diet.
I often think of the Mediterranean diet as the Taylor Swift of the nutrition world—it’s a widespread favorite because it works hard, is relatively accessible, and appeals to more than one type of fan. This diet consists of foods that carry anti-inflammatory properties which may in turn help to manage your symptoms and maintain your periods of remission. It’s also sustainable, since it’s an easy diet to stay consistent with.
But while the word “Mediterranean” may conjure images of drinking Aperol spritzes on an Italian beach, the Mediterranean diet looks a bit different. The basics of this diet include:
- An emphasis on plant-based foods, including vegetables, fruits, and legumes
- Whole grains that are minimally processed
- Sources of healthy fats, like olive oil and oily fish
- Lean protein and minimal red meat
- Small amounts of cheese
- Yogurt and other sources of probiotics
- Low alcohol intake, predominantly from wine
This nutrition plan can be customized to meet your dietary preferences—and yes, that could mean an occasional Aperol spritz. Better yet, you can also incorporate healthy options that are not in the “official” Mediterranean diet. Let’s say you enjoy a good miso soup (*raises hand*) Miso can easily be added to your version of the Mediterranean diet, since it’s a healthy source of probiotics.
Customizing an ulcerative colitis diet
The dietary tips above are great sources of inspiration, but you should think of them like Pinterest boards: Aspirational, but not 100% tailored to your unique life and circumstances. Ulcerative colitis impacts everyone differently, so any changes you need to make in terms of what you eat should be unique, too.
While we’d love to provide a single list of what foods everyone with colitis should avoid and what to eat instead, we can’t. What we can do is point you in the direction of someone who can help you figure that out: a GI-specialized registered dietitian (RD). RDs, such as those at Oshi Health, can help you understand your unique food triggers and can help tailor your diet during flare-ups. A main benefit of working with an RD is that they can ensure you stay well-nourished during flare-ups, something that’s quite tricky on your own.
Meet Oshi's GI registered dietitians
Find relief—and stay nourished
When you work with an Oshi GI registered dietitians (RD), you’ll get personalized nutrition guidance, including help with finding and avoiding potential food triggers, choosing gut-friendly supplements and recipes, and more.
Keep a food journal
For many, a food journal is a great way to hold yourself accountable to eat the right foods—either as a standalone strategy or a collaborative tool you can use with your RD. During flares, many people lose their appetite (which we totally understand!). But eating enough nutrients is essential to flare recovery and remission. Smaller, digestible meals combined with the accountability a food journal can help you get the nutrients your body needs.
Specific things to note in your food journal include:
- What you eat
- How you feel after eating
- How much you eat
- What times of day you eat
- Any other information about a meal, such as if you ate quickly due to a shorter lunch break or if you were out with friends

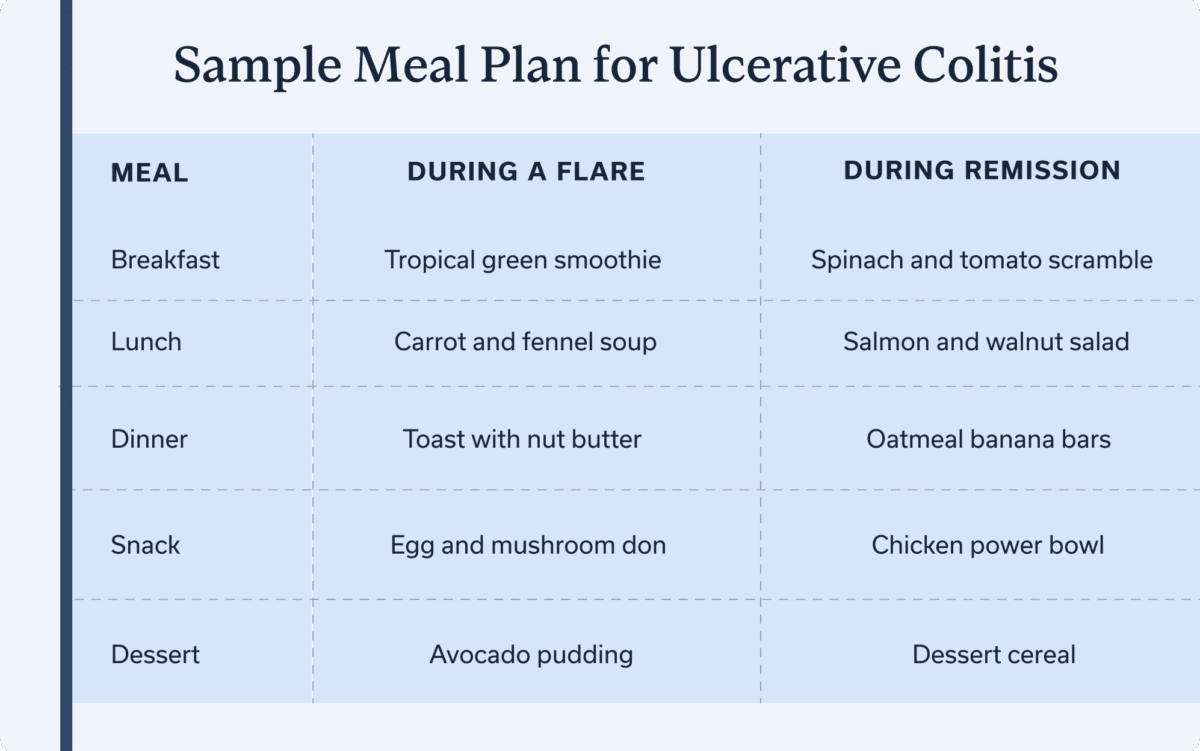
Meal plan for ulcerative colitis
If you’re anything like me, you might find healthful recipes much easier to work with than a list of foods to eat and avoid. Here’s what an average “day of eats” could look like during a flare and period of remission:
| Meal | During a Flare | During Remission |
| Breakfast | Tropical green smoothie | Spinach and tomato scramble |
| Lunch | Carrot and fennel soup | Salmon and walnut salad |
| Snack | Toast with nut butter | Oatmeal banana bars |
| Dinner | Egg and mushroom don | Chicken power bowl |
| Dessert | Avocado pudding | Dessert cereal |
These recipes are just the tip of the iceberg. For a well-rounded colitis diet plan, consult a GI specialist, such as a registered dietitian or GI provider. They can provide more recipe ideas and help tailor them to your personal triggers and symptoms.
Managing ulcerative colitis symptoms
Focusing on your diet is a great start, but it’s just one piece of the puzzle—and managing UC symptoms is definitely a 2,000-piece puzzle (without a photo on the box). Here are some other puzzle pieces to help manage your UC symptoms.
Manage stress
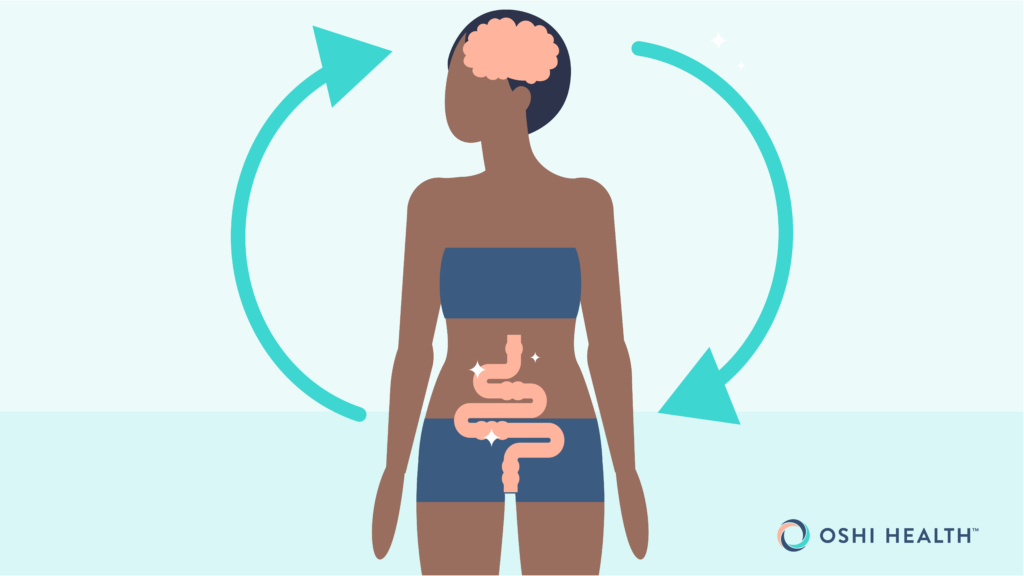
The brain and digestive system are close friends. Think back to the last time you felt knots in your stomach after receiving an email from your boss or an unexpected phone call from your kid’s school. Both of these examples demonstrate how our mind and gut work together.
And when someone has ulcerative colitis, that gut-brain connection can impact UC symptoms, too. More specifically, UC often causes stress levels or anxiety to increase, since dealing with symptoms is awkward, to say the least.
To ensure the gut-brain connection works for (not against) you, stress management techniques are a good call. Some of the most effective are box breathing and guided meditations with a GI focus.
When you lower your stress levels, your mind sends calmer vibes to your gut, which in turn can alleviate UC symptoms like cramping. I know, it sounds woo-woo, but there is actual research to back this up! If you’re unsure where to begin, consulting a professional gut-brain specialist can be a great starting point.
Sleep
Few things in life feel better than seven to nine hours of sleep. While I could wax poetic about sleep’s many benefits for hours (well, at least until my 9pm bedtime), I’ll stick to how sleep directly impacts UC. A recent study in Japan found that participants who consistently got poor sleep had more UC flares, while quality sleep reduced the number of flares. It’s important to note the researchers not only considered time spent asleep, but also sleep quality.
So while sticking to a bedtime is important, creating an environment that’s optimal for rest matters, too. Try to:
- Sleep in a dark, cool space
- Keep your bedroom quiet
- Turn off screens at least 30 minutes before bed
- Avoid large meals before bedtime
- Don’t drink alcohol or coffee close to bedtime
- Have a wind-down routine that signals to your body that it’s time to rest
Move your body
It’s never a bad day to go for a walk or have a solo dance party in your kitchen, especially if you have UC. Exercise may help reduce UC activity and inflammation, as well as improve your overall quality of life.
But before you sign up for a marathon or try to bench press your bodyweight, rest assured that light to moderate exercise works wonders for UC. In fact, lighter or moderate exercise—think long walks or a pilates class—may be the best option for managing UC symptoms (and definitely emphasize the light exercise during flares).
Experience GI care the way it should be
Oshi Health is where medical, dietary, and gut-brain treatments come together under one virtual roof, all provided by leading GI specialists. Our whole person approach is clinically proven to help patients find relief from the full spectrum of GI symptoms and conditions, including ulcerative colitis.
Complications and considerations
Untreated ulcerative colitis damages the large intestine’s inner lining. Sometimes, this damage can lead to complications, including:
- Anemia: A red blood cell deficiency
- Colon cancer: Individuals with UC are two to three times more likely to develop colon cancer, meaning that people with longstanding UC should get regular surveillance colonoscopies.
- Developmental issues: Children with UC may experience slower growth.
- Fulminant ulcerative colitis: A more serious form of UC marked by bloody stool, fever, and a fast heart rate. The “fulminant” classification indicates these symptoms are more severe .
- Inflammation outside the GI tract: UC may cause inflammation in the joints, liver, eyes, skin, and other parts of the body.
- Intestinal perforation: When inflammation creates a hole in the large intestine’s lining.
- Nutrient deficiencies: Many people with UC lose their appetite or have trouble absorbing nutrients.
- Osteopenia or osteoporosis: UC treatments, especially corticosteroids, increase the risk of developing these conditions.
- Severe bleeding: Episodes of severe bleeding through the rectum.
- Toxic megacolon: Swelling in the large intestine that is so severe, the intestine is unable to empty and could burst.
We don’t bring up these complications to scare you—and having UC doesn’t mean you’ll experience any of them. By seeking treatment, you can minimize the likelihood of complications or serious side effects.
Typically, meeting with a team of GI specialists on a regular basis to monitor treatment (and adjust when necessary) works. Sometimes, an emergency intervention may be required. Signs that you should visit the emergency room or call 911 include:
- Ongoing stomach pain
- A persistent fever
- Increased or new bleeding
If your symptoms don’t get better (or get worse) with treatment, contact a GI provider to set up an additional appointment. In that appointment, they can assess your symptoms and help modify your treatment plan.
Final thoughts
Even if there’s not one set “ulcerative colitis diet,” certain nutritional guidelines can help. As you continue on your UC journey, remember:
-
Start with a sustainable, healthy diet: A well-rounded diet, like the Mediterranean diet, often works well during periods of remission.
-
Adjust your diet during a flare: Your diet may look different during a UC flare. When symptoms get worse, opt for a GI gentle diet—think soothing and soft textured foods.
-
Personalize your nutrition plan: The foods you should and shouldn’t eat are entirely unique to your UC symptoms and lifestyle. Don’t be afraid to customize any recipes or dietary guidelines, with the help of your RD or another provider.
To work with a RD and other GI specialists on the best diet and treatment plan for ulcerative colitis, contact Oshi Health.
Frequently asked questions (FAQs)
-
People with ulcerative colitis should avoid eating trans fats, as well as unpasteurized dairy products (even those without UC should avoid unpasteurized dairy!). Trans fats can include most ultra processed foods while unpasteurized dairy products are any that haven’t undergone pasteurization, including raw milk. During a flare, you’ll likely want to opt for foods that are gentle on your GI tract, like applesauce, cooked beans, and skinless fruits and veggies.
-
The GI gentle diet can help soothe inflamed intestines. This diet focuses on soft textured foods and moderate fiber. It also emphasizes smaller, more frequent meals, cooked vegetables, and more tender meats or eggs for protein.
-
Ulcerative colitis flares are normal, but that doesn’t mean you have to suffer through them without treatment. A GI specialist should be able to create a treatment plan specific to your symptoms. While your plan will be personalized, it may include taking or adjusting medications and lifestyle adjustments to support symptom management and healing.
-
A good dinner for someone with colitis depends on if they are in remission or experiencing a flare. For the former, a well-balanced meal with lean protein or legumes, whole grains, and an abundance of vegetables cooked in olive oil is a great option—especially when paired with fruit for dessert. During a flare up, it’s important to consume foods that are easier on your GI tract, such as a soup with skinless, cooked vegetables and a side of soft bread without seeds.
-
The prevalence of lactose intolerance is higher in those with IBD compared to the general population. Those with UC and a lactose intolerance should consider lactose free options, including lactose free cows milk or plant-based milks such as almond or oat milk.
-
If you have ulcerative colitis, you can totally eat chicken, with one big caveat: the chicken should be lean and not ultra-processed. A slice of lean chicken on a bed of couscous and vegetables is an excellent choice, while fried chicken served with a side of fries may cause symptoms to flare.
-
Comfort foods are highly subjective and depend on the individual. That said, you may want to steer clear of less-than-healthy standbys like fried foods or mac and cheese. Instead, soups are a great comfort food option for someone with ulcerative colitis.
Oshi is your partner in digestive health
Feel like your digestive concerns are running your life? You’re not alone—and we’re here to help you find lasting relief.
Oshi Health GI providers, gut-brain specialists, and registered dietitians work together to address your symptoms and find solutions that actually work for you.
Whether you’re dealing with chronic digestive issues or unpredictable symptom flare-ups, our GI specialists deliver:
✔ Personalized care plans tailored to your lifestyle
✔ Science-backed strategies to calm your gut
✔ Compassionate, whole-person care
✔ And so much more!
Ready to take control of your gut health?