Considering the low FODMAP diet? Here’s a complete low FODMAP foods list showing what you should eat, surprising foods you should avoid, plus helpful tips to successfully follow this elimination diet.
Food triggers are not one-size-fits-all. For some, symptoms from irritable bowel syndrome (IBS) and other gastrointestinal (GI) conditions are triggered by lactose. For others, lactose is digestible, but fructose or another food type causes flare-ups. The low FODMAP diet stands for foods that are low in “fermentable oligosaccharides, disaccharides, monosaccharides and polyols.” This elimination diet is a tool to help you discover which foods trigger your symptoms. It requires you to eat from a low FODMAP foods list for a certain period of time, and then slowly reintroduce high FODMAP ingredients in order to determine which are and aren’t causing your symptoms.
Since its creation in Australia over seventeen years ago, the low FODMAP diet has been met with international acclaim. While effective, the low FODMAP diet is recommended in short spurts, when someone understands what foods to eat and avoid, and when completed under the supervision of a registered GI dietitian.
Understanding the low FODMAP diet
As mentioned, FODMAP is an acronym for a few “lettered” subgroups: fermentable oligosaccharides, disaccharides, monosaccharides, and polyols. These four subgroups are carbohydrates that digest slowly in the small intestine.
These food groups can cause a number of uncomfortable digestive symptoms, such as:
- Bloating
- Constipation
- Cramping
- Diarrhea
- Discomfort in the stomach
- Gas
- Pelvic pain
A 2024 study also found high FODMAP foods can trigger symptoms of IBS, endometriosis, and diarrhea in some study participants. It may also reduce gastrointestinal symptoms associated with fibromyalgia.
The catch-22 is that FODMAPs also provide food for bacteria in the gut, strengthening overall gut health. “High FODMAP foods are in themselves nutritious foods that need not be avoided unless one has a sensitivity,” explains Sameer Berry, MD, MBA, Chief Medical Officer at Oshi Health.
The gut is highly personal and sensitive, meaning there aren’t blanket recommendations for which high FODMAPs to avoid and which it’s OK to indulge in. A nutritious meal for you may include a trigger for the next person, or vice versa.
To discover your personal triggers, a GI specialist may recommend the low FODMAP diet. This three-stage elimination diet highlights well- and poorly tolerated foods in about three quarters of those who try it.
Unlike other popular diets, such as the Mediterranean diet, the low FODMAP diet isn’t one to follow for life. Its primary purpose, Dr. Berry says, is to discover foods that cause GI symptoms and to deliver sustainable symptom relief, even after the elimination diet is complete.
Identifying high FODMAP foods
“FODMAPs can be found in a wide variety of plant foods and dairy products,” says Kaitlin Voicechovski, MS, RDN, LDN, Lead Registered Dietitian at Oshi Health. She adds that there’s not a clear pattern between low and high FODMAP foods, making it tricky to identify what you can and can’t eat on this diet.
Fortunately, you can refer back to this list of high FODMAP foods to avoid.
Disclaimer: this list provides general guidance, but labeling foods as high FODMAP can be complicated. Portion size greatly impacts whether a food is considered high FODMAP, which is another reason to complete this diet with guidance from a GI registered dietitian.
Fruits
- Apples (including applesauce and apple juice)
- Any processed fruit juice
- Apricots
- Avocados
- Bananas (if ripe)
- Blackberries
- Dried fruits, such as
- Raisins
- Prunes
- Figs
- Lychees
- Mangos
- Nectarines
- Peaches
- Pears
- Pineapples
- Plums
- Watermelon
Vegetables
- Artichokes
- Asparagus
- Broccoli
- Brussels sprouts
- Butternut squash
- Cabbage
- Cauliflower
- Celery
- Fennel
- Garlic, in any form
- Green or yellow beans
- Leeks, other than the leaves
- Mushrooms
- Onions
- Sugar snap peas
- Summer squash
Proteins
- Beans
- Chickpeas
- Kidney beans
- Lentils
- Lima beans
- Marinated meats or seafood
- Pinto beans
- Soy beans
- Split peas
- Sausage
- Salami
Grains
- Cakes
- Couscous
- Cookies
- Bread
- Pasta
- Pastries
- Snack bars
- Any other products with barley, wheat, or rye
Nuts & seeds
- Black-eyed peas and their seeds
- Cashews
- Pistachios
Dairy and alternatives
- Cow milk
- Goat milk
- Ice cream
- Sheep milk
- Soft cheese, including
- Processed cheese
- Ricotta
- Soy milk (if made from whole soybeans)
- Yogurt
Condiments & sauces
- Any sauces with high fructose corn syrup
- Balsamic vinegar
- Molasses
- Most BBQ sauces
- Most ketchup brands (though low FODMAP ketchups exist)
- Teriyaki sauce
- Worcestershire sauce
Other
- Oolong
- Agave syrup
- High fructose corn syrup
- Honey
- Port
- Rosé wine
- Sherry
- Certain teas, including
- Chamomile
- Dandelion
- Fennel
Low FODMAP food options
While the list of high FODMAP foods is quite extensive, there are still plenty of great low FODMAP options. Below is a comprehensive list that even includes wine and ice cream (lactose-free, that is). For recipes with these ingredients, check out our free low FODMAP cookbook.
Disclaimer: remember when we said labeling foods as high FODMAP was complicated? The same is true of a low FODMAP foods list. Portion size will impact how much you can eat of the foods listed below.
Fruits
- Bananas (unripe)
- Blueberries
- Cantaloupes
- Clementines
- Dragon fruit
- Durian
- Grapes
- Honeydew
- Kiwi
- Lemon juice, no added ingredients
- Lime juice, no added ingredients
- Olives
- Oranges
- Pineapples
- Prickly pear fruit
- Rhubarb
- Strawberries
- Tangelo
- Yellow papaya
Vegetables
- Alfalfa sprouts
- Arugula
- Bamboo shoots
- Bean sprouts
- Bok choy
- Carrots
- Chicory leaves
- Chili pepper, red
- Chives, green part only
- Cucumber
- Eggplant
- Endive
- Fennel bulb
- Green bell pepper
- Green beans
- Kale, cooked
- Leek, leaves only
- Leaf lettuce
- Parsnip
- Pattypan squash
- Pickles, dill or sour, no garlic added
- Radishes
- Rutabaga/Swedish turnip
- Scallions/green onions, green part only
- Seaweed
- Spinach
- Sweet potatoes
- Tomatoes
- Tomato paste/concentrate
- Turnips
- Water chestnuts
- Winter squash
- Zucchini
Proteins
- Beef
- Buffalo
- Chicken
- Duck
- Eggs
- Egg substitute
- Goat
- Lamb
- Pork
- Quorn (Grounds/Mince only)
- Seafood, any kind
- Tempeh
- Tofu, firm only
- Turkey
Grains
- Amaranth
- Buckwheat cereal
- Buckwheat flour
- Corn, rice or quinoa pasta
- Corn tortillas
- Crackers, rice or corn
- Cornmeal/polenta, dry
- Gluten-free pretzels
- Gluten-free bread
- Grits
- Millet, cooked
- Oatmeal/porridge, cooked
- Oat bran, cooked
- Oat flour
- Popcorn
- Potato chips
- Quinoa, cooked
- Rice or corn cakes
- Rice
- Rice bran
- Soba noodles (100% buckwheat)
- Sourdough spelt or wheat bread
- White potatoes
Nuts & seeds
- Almond butter
- Chia
- Nuts, any kind besides cashews and pistachios
- Peanut butter
- Pumpkin seeds
- Seeds
- Sunflower
Dairy and alternatives
- Almond milk
- Butter
- Hard cheese, regular or reduced-fat, including
- Cheddar
- Swiss
- Parmesan
- Brie
- Mozzarella
- Feta
- Coconut cream
- Cottage cheese, lactose-free
- Cream cheese
- Dry curd cottage cheese
- Goat cheese/chevre
- Half-and-half
- Heavy cream, whipped
- Kefir, lactose-free
- Milk, lactose-free
- Ricotta cheese, regular
- Sour cream
- Sour cream, low-fat
- Yogurt, lactose-free
Condiments & sauces
- Mayonnaise
- Soy sauce
- Tartar sauce
- Tahini
Other
- Beer
- Candy/chocolate made with allowed ingredients
- Corn syrup (not high-fructose)
- Coffee, black, limit one per day
- Ice cream, lactose-free
- Jam
- Jelly
- Maple syrup, 100% pure (not “pancake syrup”)
- Margarine
- Oil, any type, including
- Soybean
- Coconut
- Garlic-infused
- Rice milk
- Spirits, 1 1⁄2 oz. (not rum)
- Certain teas, such as
- Black
- Green
- Ginger
- Peppermint
- Rooibos
- Licorice
- Wine, red, white, or sparkling
- Sorbet with allowed ingredients
- Some sugar types, including
- Brown
- Cane
- Palm
- Confectioner’s
- Granulated
- Syrups, including
- Cane
- Sugar
- Golden
Healthy eating on a low FODMAP diet
“The Low FODMAP diet is not intuitive and involves a lot of nuance,” says Dr. Berry. Not only is it difficult to identify high and low FODMAP foods, it can be hard to get the necessary nutrients to support overall health.
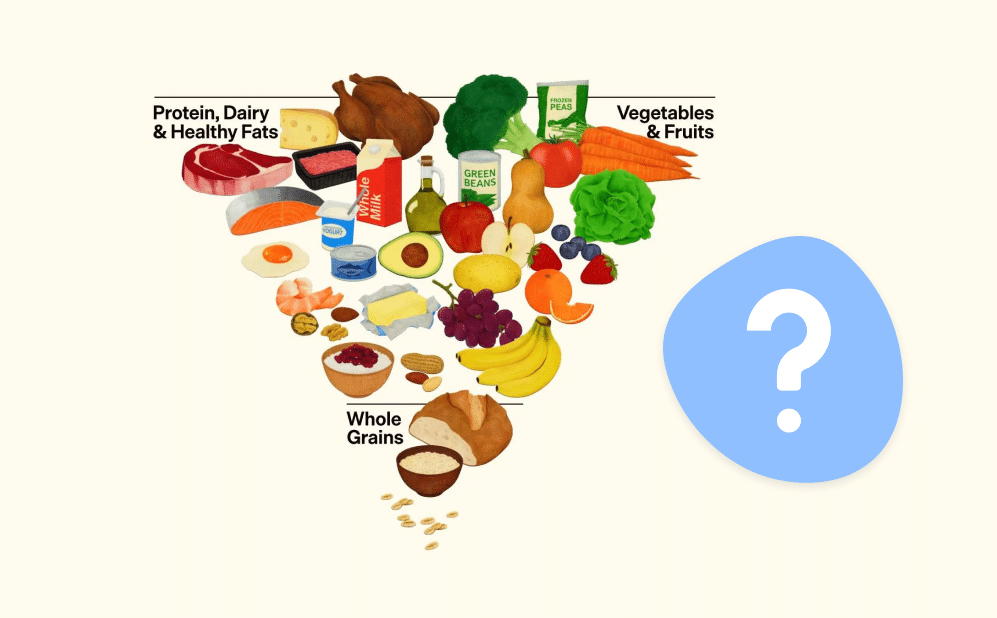
But the keyword is hard, not impossible. With proper guidance, your low FODMAP plate can include the key aspects of a well balanced diet, such as:
- A variety of fruits, vegetables, proteins, and whole grains
- Enough fiber to feel full and satisfied
- Healthy fats like nut butter or margarine
- Fruits and veggies of all colors
- Unprocessed foods whenever possible
In the elimination stage, Voicechovski finds getting enough fiber to be the biggest challenge. Blueberries, papaya, kiwi, carrots, lettuce, and potatoes are some of her favorite low FODMAP fiber sources.
Another tricky factor is portion size, Voicechovski adds. Eating an entire apple, for example, will have a higher FODMAP load than eating one apple slice. However, a full apple is often a recommended portion size for someone who is not on the low FODMAP diet. While nutrition labels provide recommended portion sizes, these quantities may be too large for the low FODMAP diet.
To determine the correct portion for you during the low FODMAP diet, work with a GI registered dietitian.
Meet Oshi's GI registered dietitians
Find relief—and stay nourished
When you work with an Oshi GI registered dietitians (RD), you’ll get personalized nutrition guidance, including help with finding and avoiding potential food triggers, choosing gut-friendly supplements and recipes, and more.
Managing food triggers
A low FODMAP diet can be broken down into three stages. These are referred to as elimination, reintroduction, and personalization. Together,the stages allow you to identify and manage food triggers so you can alleviate digestive symptoms.
Stage 1: elimination
To begin the low FODMAP diet, swap all high FODMAP foods with low FODMAP alternatives. “The goal of the elimination phase is to reduce overall FODMAP intake to the greatest extent possible,” says Voicechovski.
She adds that this phase won’t last forever. Typically, it takes two to six weeks. If symptoms improve, it’s beneficial to move on to step two. If they don’t, Voicechovski advises to abandon the diet and try another solution.
Stage 2: reintroduction
“Everyone has their own unique set of FODMAP sensitivities, and the goal of the reintroduction phase is to better understand an individual’s tolerances to each of the FODMAP subgroups,” says Voicechovski.
During this stage, most aspects of the low FODMAP diet are maintained. The lettered subgroups (fermentable oligosaccharides, disaccharides, monosaccharides and polyols) are phased back one at a time, so the individual can learn more about how their body responds to each isolated FODMAP type.
Many people find it useful to keep a food diary when reintroducing foods. In it, you can add notes on what you ate, portion sizes, how you felt overall, and any specific symptoms you experienced.
Six to eight weeks after starting this phase, an individual should have a better idea of what foods are safe, what can be consumed in moderation, and which foods to avoid, says Voicechovski.
Stage 3: personalization
“During this phase, the learnings from the reintroduction phase are applied and higher FODMAP foods of well-tolerated subgroups are introduced back into the diet alongside all of the low FODMAP foods already being enjoyed,” says Voicechovski.
While a registered dietitian will probably have feedback on what an effective dietary plan looks like moving forward, it’s important to ensure you can sustain that diet. The end result should be a flavorful diet and sustainable symptom relief.
Overcoming common challenges
“Navigating the diet alone is cumbersome, often leading to unnecessary struggle and the risk of going through the effort only to implement the diet incorrectly,” says Voicechovski, “A GI registered dietitian can help you better determine whether a trial of the low FODMAP diet is right for you, and if so, guide you through the diet with greater ease and a higher chance of success.”
At Oshi, we ensure patients have a whole-person approach and support for their mental and physical health while undergoing the low FODMAP diet. Oshi patient S.C. reflected on their experience, explaining that “the service provided by Oshi for my IBS issues is unique in that it covers three focus areas: physiological (doctor), dietary, and psychological.” They added that “this rounded approach combined with personalized guidance is effective. The providers have been excellent at actively listening to my specific situation and then tailoring strategies going forward.”
Specific challenges a GI registered dietitian can help you work through include:
- Identifying high FODMAP foods
- Identifying and managing food triggers
- Maintaining a balanced diet throughout
Along with having a great team for support, it’s important to stay positive and focused on eating well-balanced meals. A low FODMAP diet isn’t easy, but it can ease symptoms for years to come.
Getting started with a low FODMAP diet
Before starting this elimination diet, brainstorm what the three steps may look like (to recap: elimination, reintroduction, and personalization). For each phase, mark a start and end date on a calendar. This helps make the diet more tangible;written goals with specific timelines are often easier to achieve.
Other steps to prepare include:
- Create a list of your favorite meals using low FODMAP foods
- Consider which foods you may introduce for each lettered category
- Journal about what success will look like for you. This could even be the first entry in your FODMAP food journal.
Once ready, start with phase one: eliminating high FODMAP foods for two to six weeks before gradually introducing one group at a time and monitoring symptoms. Working with a healthcare professional or registered dietitian can make it easier to develop a personalized low FODMAP diet plan.
For B.P., working with the right GI specialists and treatment plan made all the difference. B.P. said, “After over 15 years of suffering, more than 25 doctors of all specialties, and tens of thousands of dollars, I FINALLY have an answer and a treatment plan! I highly recommend Oshi Health to anyone who has lost hope.”
Frequently asked questions (FAQ)
-
If experiencing Gi symptoms, like bloating, cramping, or constipation, but you can’t figure out what foods are to blame, the low FODMAP diet may be a good choice. Completing the diet, however, can be quite tricky, and should be done under the supervision of a GI specialist.
-
A low FODMAP diet is one that avoids foods that are high in fermentable oligosaccharides, disaccharides, monosaccharides, and polyols. Low FODMAP foods to add to your plate include animal proteins, eggs, almond milk, rice, quinoa, and certain fruits and veggies, including grapes, eggplants, and potatoes.
-
Low FODMAP foods can be tricky to identify. With other diets, such as the paleo or vegetarian diet, it’s easy to identify what to avoid (grains and processed foods or meat, respectively). Instead, high and low FODMAP choices hail from all food groups. Some surprising low FODMAP foods include lactose-free ice cream, cream cheese, and brown sugar.
-
A registered dietitian can (and should) guide how long you stay on the low FODMAP diet. For most, the elimination stage lasts two to six weeks and reintroduction is six to eight weeks.
-
Vegetables to avoid on the low FODMAP diet include onions, garlic, snow peas, cauliflower, and asparagus. This list is nonexhaustive, and identifying high FODMAP vegetables is difficult. To make it easier, consult with a GI registered dietitian who can advise you on what vegetables to eat or avoid.
-
All FODMAPs (fermentable oligosaccharides, disaccharides, monosaccharides, and polyols) can trigger digestive symptoms such as bloating and diarrhea. That doesn’t mean all high FODMAP foods cause these symptoms in every individual. Some particularly common FODMAP triggers include lactose (which is found in dairy products like most cheeses and cow milk), and fructose (a common sugary add-on to drinks and many processed desserts).
Final thoughts
The low FODMAP diet can be a powerful way to identify and control GI symptom triggers. This diet consists of three steps: a total elimination of high FODMAP foods, reintroduction of different FODMAP categories, and personalizing your everyday diet to avoid foods that trigger your symptoms. While effective, enacting a low FODMAP diet can feel overwhelming, confusing, or lonely, and that’s normal.
Oshi provides a supportive team with GI-specific expertise to hold you accountable. Plus, Oshi offers extra resources and a supportive community so you feel more confident and less lonely on your low FODMAP journey. If looking for a personalized approach to the low FODMAP diet, schedule an appointment with an Oshi GI specialist today.
Take charge of your gut health with expert dietary support
Your nutrition plays a powerful role in your digestive well-being. But figuring out what to eat can be overwhelming, especially if you’re dealing with chronic or occasional digestive symptoms.
Oshi’s registered dietitians have specialized knowledge in all GI symptoms and conditions. They work closely with you to:
✔ Identify foods that help—not hurt—your gut
✔ Develop personalized meal plans that fit your lifestyle
✔ Guide you through small, sustainable changes for symptom relief
✔ And so much more!
Ready to make mealtime less stressful and feel in control again?