Bloating, diarrhea, and abdominal pain are never fun, but they can be easier to manage when you know what’s causing them. One potential cause is Crohn’s disease, a type of inflammatory bowel disease (IBD) that impacts the gastrointestinal (GI) tract.
The Centers for Disease Control and Prevention (CDC) estimates that somewhere between 2.4 and 3.1 million people in the U.S. have Crohn’s (or ulcerative colitis, another form of IBD.) And that’s only counting the cases that are already diagnosed!
But what exactly is Crohn’s disease? Ahead, we’ll dive into this condition, the most common symptoms, and how this condition is diagnosed. We’ll also discuss lifestyle modifications and treatments that can help control or prevent Crohn’s flare-ups and help manage the stress that comes from living with a chronic disease. With the right care and lifestyle, people with Crohn’s can manage their symptoms and live a fulfilling life.
What is Crohn’s disease?
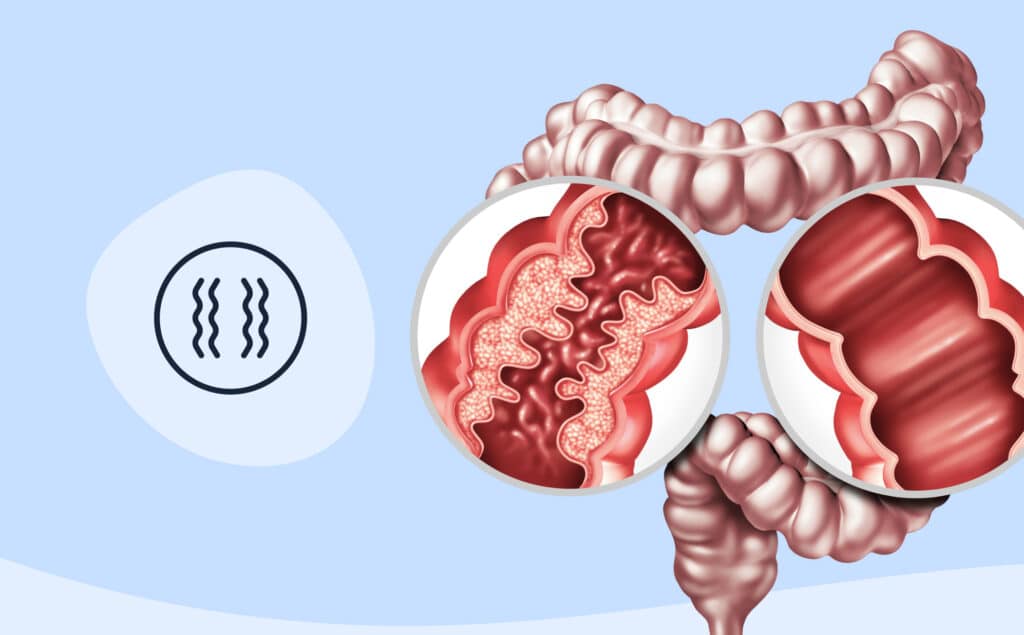
“Crohn’s disease is an autoimmune disease where your immune system attacks your digestive tract,” says board-certified gastroenterologist Geetanjali Akerkar, MD. The name comes from one of the three scientists (Burrill Crohn, Leon Ginzberg, and Gordon D. Oppenheimer) who first described Crohn’s in 1932—you can probably guess which one.
This attack manifests as inflammation and irritation in the GI tract, often in the small intestine or large intestine. While the small and large intestine are the most commonly affected places, Crohn’s disease can impact any part of the GI tract, from the mouth to the anus. In fact, there’s about a 50/50 split between patients with ileocolonic Crohn’s (when the disease is isolated in the small and/or large intestine) and Crohn’s that isn’t isolated to the intestines.
Crohn’s disease risk factors
Irregularities in the immune system are the primary reason for Crohn’s disease, though researchers are unsure what causes these irregularities to begin with.
While more research is needed, the leading theories suggest a combination of genetics, environment, and external triggers are at play. In fact, your risk of developing Crohn’s is higher if a close family member, such as a parent or sibling, has any form of IBD. Emerging research suggests genetics may play a role in the disease’s progression too, though more studies are required to confirm this idea. Studies have consistently shown that cigarette smoking is also associated with Crohn’s disease.
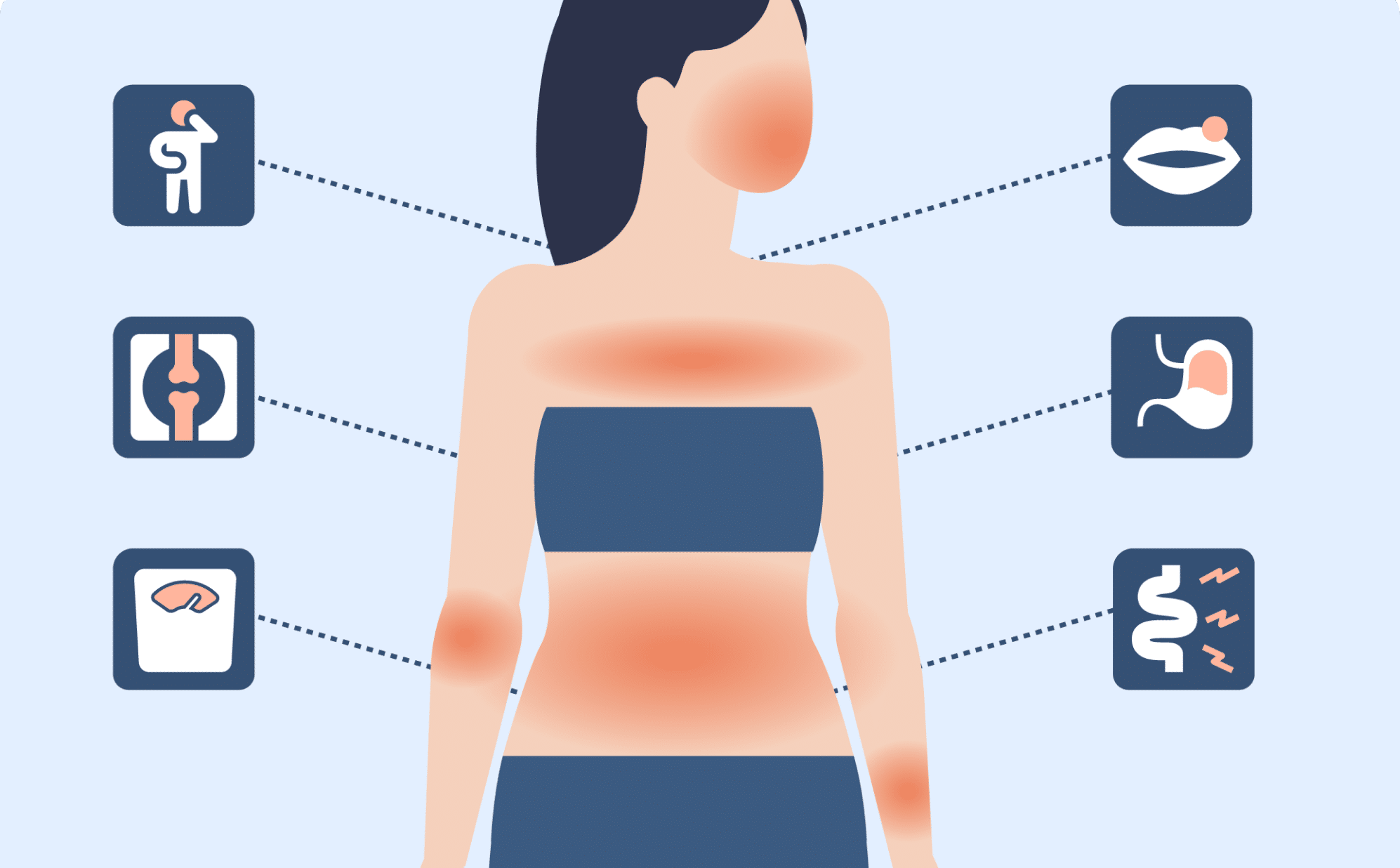
Symptoms of Crohn’s disease
“Common symptoms include abdominal pain, bloating, and diarrhea,” says Dr. Akerkar. She adds that you might confuse these symptoms with those of other conditions, such as irritable bowel syndrome (IBS) or even appendicitis. “Some patients are thought to have appendicitis to later find out they have Crohn’s disease,” she adds.
Alongside stomach pain, diarrhea, and bloating, other potential symptoms include:
- Weight loss
- Pain or redness in the eye
- Fatigue
- Fever
- Nausea
- Loss of appetite
- Red, tender bumps on the skin
- Joint soreness or paint
- Frequent bowel movements
What can make Crohn’s even more difficult to diagnose is that symptoms come and go. Most patients experience flare-ups and periods of remission that can last weeks or even years.
Complications of Crohn’s disease
While Crohn’s impacts the gut, you may have noticed that the list of symptoms transcends the GI tract. That’s because Crohn’s influences overall health, including putting individuals at risk for other complications, such as:
- Abscesses: Chronic inflammation can cause painful abscesses, which are collections of pus, in the lining of the GI tract.
- Anemia: A red blood cell deficiency that can be caused by bleeding and inflammation related to Crohn’s.
- Anal fissures: Small tears in the anal tissue may cause bleeding, pain, and itching.
- Bowel obstructions: An obstruction in the large and/or small intestine that blocks the movement of food to the bowels.
- Fistulas: Holes in the intestinal lining that are caused by chronic inflammation and often become infected.
- Higher risk of blood clots: Having Crohn’s places someone at higher risk of blood clots.
- Increased risk of colon cancer: Crohn’s, can increase someone’s risk of colon cancer, especially if left untreated and if Crohn’s impacts the colon.
- Malnutrition: Crohn’s can make it difficult to absorb nutrients, and up to 85 percent of those with Crohn’s experience some sort of nutritional deficiency.
- Viral infections: There is a correlation between having Crohn’s disease and a higher risk for certain viral infections, including Epstein-Barr virus, hepatitis B-virus, and COVID-19.
Reading through these complications can be intimidating, but there are steps to mitigate the risk of developing them. The best step you can take? Seeing a gastroenterologist or a team of GI specialists who can help manage Crohn’s disease symptoms—but more on that, and on managing Crohn’s, ahead.
Experience GI care the way it should be
Oshi Health is where medical, dietary, and gut-brain treatments come together under one virtual roof, all provided by leading GI specialists. Our whole person approach is clinically proven to help patients find relief from the full spectrum of GI symptoms and conditions, including Crohn’s disease.
Crohn’s disease in children and adolescents
The most common time to be diagnosed with Crohn’s disease is in your 20s or early 30s. That said, Crohn’s disease can come at any age. Since children are still growing, they may also experience growth defects and are more likely to experience bowel obstruction. Due to these key differences, children and adolescents diagnosed with Crohn’s disease should work with a pediatric gastroenterologist. (Please note that Oshi Health treats people ages 18 and older.)
Crohn’s disease and mental health
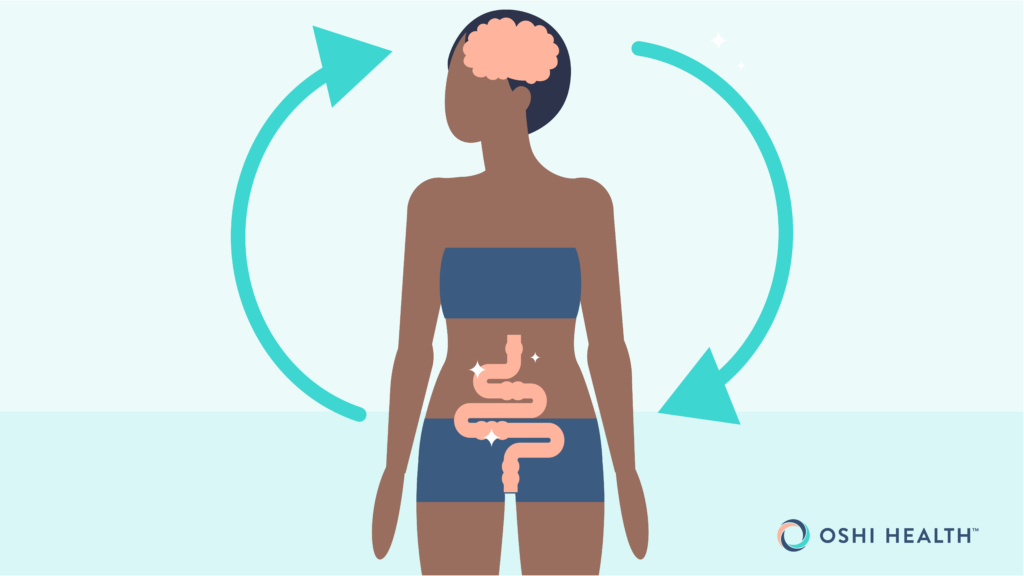
Let’s say your stomach is in knots before a presentation at work or during a first date. Both are signs of the gut-brain connection—a relationship that is highly relevant for people living with Crohn’s. “There is a direct relationship between mental health symptoms and Crohn’s. As one disease increases in intensity, so does the other, in a vicious cycle that leads to increasing GI system distress,” says Steve Feinstein, PhD, a GI clinical health psychologist and gut-brain specialist at Oshi Health.
While this cycle can be difficult to break, it’s definitely possible. Dr. Feinstein takes a two-pronged approach with his patients: educate and intervene. “Understanding of the brain-gut axis, and nervous system involvement in the brain’s ability to regulate the gut, is often an important first step to understanding the forces behind this vicious cycle,” explains Dr. Feinstein.
Diagnosis and testing for Crohn’s disease
“Crohn’s can often take years to diagnose and turn a life upside down in the process,” says Dr. Feinstein. Working with a team of GI specialists can often speed up a diagnosis.
To start, a doctor will ask about your medical history, including your symptoms, any medications you take, and your family history. Afterwards, they will conduct a physical exam. A physical exam and your medical history can’t definitively diagnose Crohn’s. From there, they will order a biopsy of the GI tract to confirm a Crohn’s diagnosis. Sometimes, they’ll order other diagnostic tests, such as:
- Blood tests
- Stool tests
- Endoscopy, which can include a colonoscopy, capsule endoscope, or upper endoscopy
- Imaging procedures, such as a CT scan or MRI
Some tests, like a colonoscopy, are vital to diagnosing Crohn’s disease. Others may be recommended as a supplemental test by a doctor.
Crohn’s disease treatment options
When it comes to treatment options, there’s good and bad news. The bad news: Crohn’s disease has no known cure. The good news: There are multiple options that can help manage symptoms, prevent future flare-ups, and those with Crohn’s can have long periods of remission.
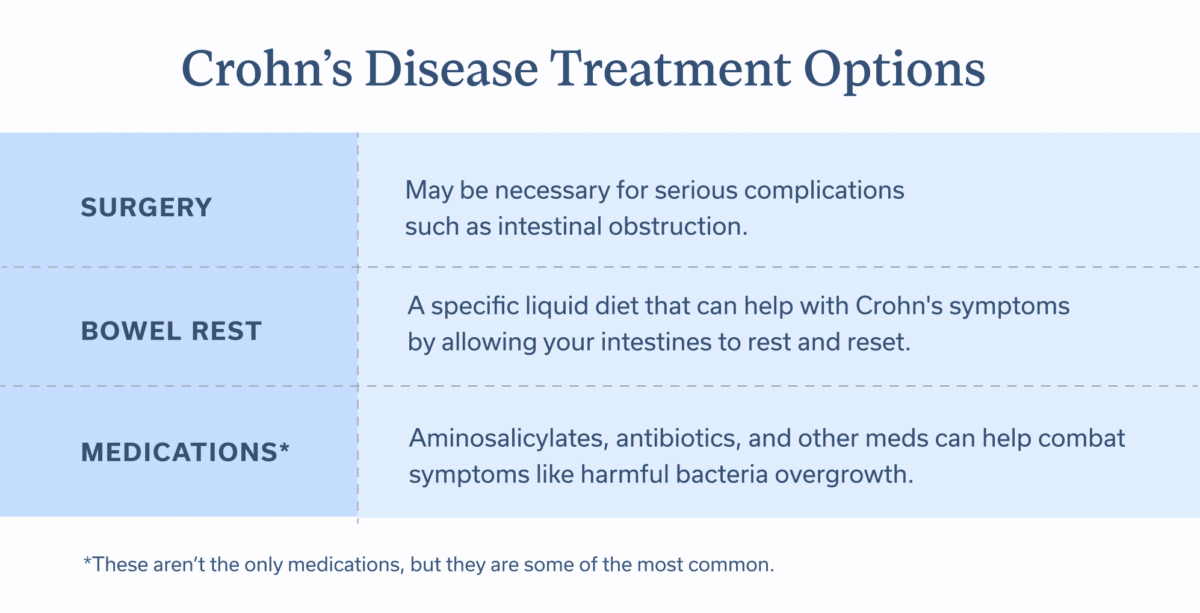
Medications
Medications can’t cure Crohn’s, but some drugs can reduce the inflammation involved in Crohn’s disease. In this way, they can help prevent or heal intestinal damage. Commonly prescribed ones include:
- Aminosalicylates: A class of anti-inflammatory medications that can help people with moderate to mild Crohn’s disease.
- Antibiotics: These may be prescribed when there’s a viral illness or other complication related to Crohn’s.
- Biologics: These medicinal therapies neutralize specific proteins produced by the immune system. Unlike other options on this list, biologics are administered in a hospital or outpatient clinic, not at home.
- Immunomodulators: These medications reduce GI tract inflammation by calming the immune system.
- Pain medications: Over-the-counter pain medications, like acetaminophen, may be recommended during intense flare-ups.
- Steroids: Also known as corticosteroids, these medications can reduce inflammation and immune system activity.
- Targeted synthetic small molecules: A medication class that targets parts of the immune system with the aim of decreasing inflammation. Usually, they’re prescribed for moderate to severe cases of Crohn’s disease.
Based on Crohn’s severity, location, and other factors unique to you, a doctor may prescribe the best medication(s) from the list above.They may also recommend supplements to prevent or treat nutritional deficiencies.
Surgery
When Crohn’s disease is severe or leads to complications, surgery may be required. Surgery is often recommended for life-threatening bleeding, fistulas, intestinal obstructions, and when medications don’t work.
About 60 percent of those with Crohn’s disease will need surgery at some point. That percentage is decreasing year-over-year, and emerging research suggests lifestyle modifications, like quitting smoking, can reduce the likelihood of surgery.
Bowel rest
In severe cases, a doctor may prescribe bowel rest for a few days, a week, or even longer. Bowel rest is when an individual doesn’t eat or drink, except specific liquids that contain nutrients. Typically, these nutrients are delivered through a feeding tube inserted into the stomach or small intestine. Receiving these liquids via an IV may also be an option.
Managing and preventing Crohn’s disease
You can also take actions to minimize the chance of flare-ups and complications. A team of GI specialists can identify what lifestyle modifications make the most sense for you, but some of the most common target your diet, mental health, and smoking habits.
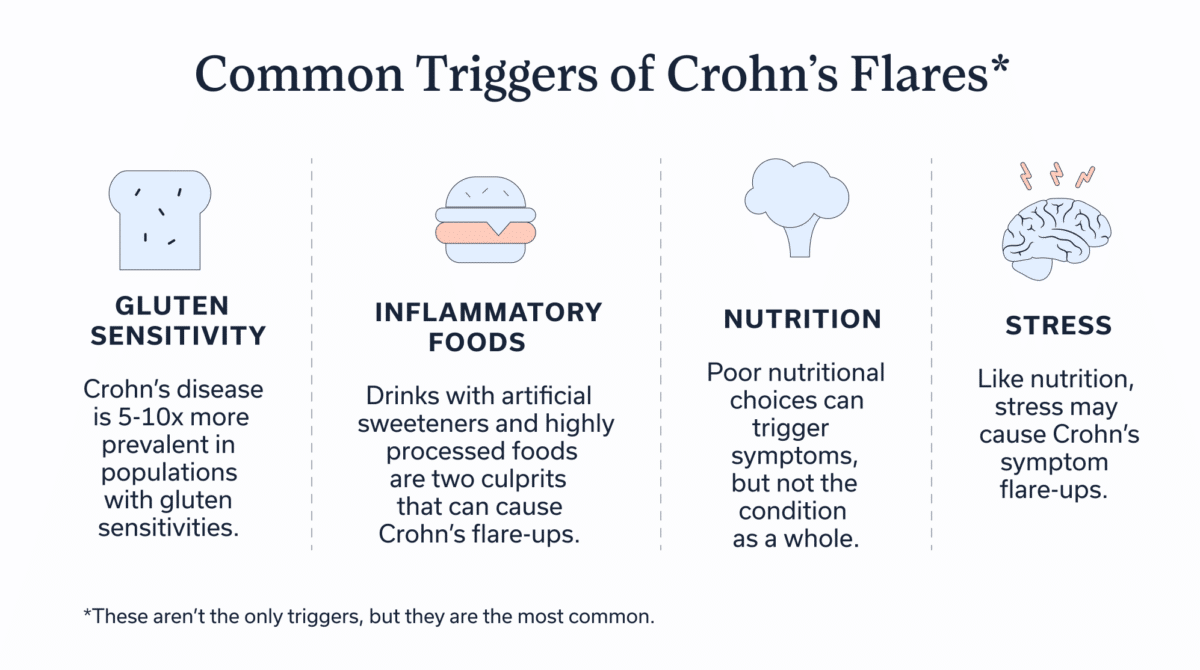
Diet
People with Crohn’s disease may find that what they eat affects how they feel—and may modify their diet to minimize symptoms, especially during flares. Those with Crohn’s often focus on avoiding any dietary triggers.
Common diet-related symptom triggers (which are not causes of the disease itself) include:
- Processed Foods: Drinks with artificial sweeteners, concentrated sweets, and high fat, highly processed foods are common culprits that can increase symptoms.
- Caffeine & Alcohol: Both are known to impact digestion & for many wreak havoc during flares.
- Lactose: Lactose intolerance is also common, having been reported in 44-70% of the IBD population.
- Gluten: Additionally, Crohn’s disease has been reported as five to ten times more prevalent in populations with celiac disease—these folks must avoid gluten.
While common, these triggers don’t impact everyone with Crohn’s disease, and the approach you take may look different based on your personal observations, preferences, and disease activity.
In addition to minimizing intake of specific diet triggers, other strategies that may help to manage symptoms include:
- Utilizing the GI gentle diet during flare-ups, which involves taking a soft-texture approach to food choices. Texture can have a big impact on tolerance to a given food, and soft options are often less irritating to an inflamed gut.
- Chewing food more thoroughly can improve digestion and cause less irritation
- Eating smaller but more frequent meals may improve tolerance and help to ensure nutrient needs are met.
Lastly, a word on fiber: While those with IBD may have been warned against high fiber foods, there’s limited data to support this stance. In fact, recent research suggests fiber likely plays a protective role in IBD. During flares, fiber tolerance may be lower or restricted more to the “GI Gentle” options discussed above. In periods of remission many people with IBD can work toward a dietary pattern with as much dietary fiber as can be tolerated.
For Oshi patient Justin Z, diet modifications were key to calming his Crohn’s symptoms. He reflected, “My improvement was really set in motion when my Oshi registered dietitian recommended a GI gentle diet. That calmed my physical symptoms (pain, nausea, bloating, etc.) within a couple of days.”
Smoking
If you don’t smoke, don’t start. If you already smoke, know that current smokers are more likely to develop Crohn’s. For those who already have Crohn’s disease, smoking can increase the risk of hospitalization.
If looking to quit, know you’re not alone. The United States Department of Health and Human Services has developed free resources for quitters, and your doctor can provide additional support during your quitting journey.
Acceptance-based therapy
As we’ve discussed, mental health can influence (and be influenced by) Crohn’s. To manage living with a chronic GI condition, many patients find it useful to work with a gut-brain specialist. Typically, these specialists focus on addressing emotions and feelings that stem from having Crohn’s disease.
Dr. Feinstein often uses acceptance-based strategies to accomplish this goal. Acceptance-based therapy “is a specific cognitive strategy that helps members learn how to accept their condition and reality,” he explains. These strategies help build psychological flexibility by accepting tricky emotions and thoughts related to Crohn’s symptoms. This approach can reduce stress, foster resilience, and enhance coping strategies, all of which enhance someone’s quality of life.
Stress management
Stress is one of the most prevalent risk factors for experiencing more severe Crohn’s flare-ups. Before you panic (or stress), it’s important to know that stress management techniques can play a huge role in preventing Crohn’s flare-ups.
One of the most evidence-backed ways to reduce stress? Mindfulness. MBIs (aka mindfulness based interventions) cultivate awareness and acceptance of the present moment, improving mental well-being and offering valuable support when facing the challenges of living with Crohn’s.
Living with Crohn’s disease
“The good news is that with a proper diagnosis, there are many treatments available to control your immune system and symptoms so you can live well,” says Dr. Akerkar. While Crohn’s disease is a lifelong condition, lifestyle and dietary modifications can reduce flare-ups.
Sara Levitt, a Crohn’s and ostomy advocate, adds that having the right community and medical team also makes it easier to live with Crohn’s. “The journey can be very long and feel hopeless at times, but keeping an optimistic outlook is what got me through my most challenging times,” she says, “I know it’s easier said than done, but that’s why connecting with your community is so important. Having a medical team you feel safe and confident in is such an important part but having a circle that can understand you, your emotions, and how you feel directly goes miles, too.”
- of patients find relief in 10 weeks or less
- of patients report better quality of life within 3 months
- decrease in unecessary (and expensive) procedures and tests
Source: Results of a clinical trial conducted in partnership with a national health plan
When to see a doctor
If you think you have Crohn’s disease or that the disease is progressing, there are some signs to look out for:
- Blood in stool
- Constipation
- Significant weight loss
- Fever
- Unable to pass gas
- Nausea or vomiting
- Severe abdominal pain
- Uncontrollable diarrhea
- Weakness or fatigue
If experiencing any symptoms, contact your doctor to test for Crohn’s disease or to modify your current treatment plan. An ER trip may be necessary if experiencing uncontrollable diarrhea, severe abdominal pain, weakness that won’t go away, or significant blood in stool or in vomit.
Before going to the doctor’s, brainstorm any questions or concerns to discuss. Possible questions to ask include:
- Do I have Crohn’s disease or is another condition causing my symptoms?
- What’s the best treatment plan for the severity and location of my Crohn’s disease?
- What lifestyle modifications can I make to prevent flare-ups?
- What dietary changes should I consider, if any?
- What medications may help—and which should I avoid?
- Can my family take steps to lower their risk of Crohn’s disease?
IBD experts working together for you
Meet Oshi’s GI providers, registered dietitians, and gut-brain specialists.
Final thoughts
Crohn’s disease is a serious condition that can decrease your quality of life. But it doesn’t have to. To make Crohn’s more manageable, heed these key takeaways:
If you’re ready for an accurate diagnosis and to develop an effective treatment plan alongside a provider that listens, get started with Oshi Health today.
Frequently asked questions (FAQs)
-
There is no known cause for Crohn’s disease. Irregularities in the immune system and genetics appear to play a role, but researchers have yet to determine the exact cause of this condition.
-
According to recent data, the life expectancy for women with IBD is 75.5 to 78.4 years old. For men, it’s 72.2 to 75.5 years. This is about the same as average life expectancy for all Americans.
-
Dietary triggers for Crohn’s symptoms are highly personal; what triggers symptoms for one person may not for another. That said, some common triggers for Crohn’s symptoms include lactose, concentrated sweets, insoluble fiber, caffeine, alcohol, and FODMAPs, a group of carbohydrates that move slowly through the small intestine, are the most likely to trigger Crohn’s.
-
Crohn’s flare-ups have many triggers, including infections, dietary choices, stress, and smoking. Working with a team of GI specialists can help you find your specific triggers.
-
Crohn’s disease occurs when your immune system starts attacking the GI tract, often the small intestine. This attack leads to irritation and inflammation, which can manifest as symptoms such as diarrhea, abdominal pain, and nausea.
Supportive, expert-led care for Crohn's
Crohn’s disease symptoms can often turn life upside down. And it can be tough to navigate medical care when you’re constantly dealing with the unexpected.
We’re here to help.
Oshi Health GI providers, gut-brain specialists, and registered dietitians work together to address complex conditions like Crohn’s.
Our GI specialists will work with you to reduce flare-ups through:
✔ Personalized care plans tailored to you
✔ Evidence-based IBD nutrition guidance
✔ Science-backed treatments
✔ Ongoing virtual care when you need it, including evenings and weekends
✔ And so much more!
Ready to feel more in control of your Crohn’s?