When constipation crops up, it can lead to dreaded discomfort, bloating, and cramping. But when do these symptoms become cause for concern? Constipation danger signs include abdominal pain, bleeding, inability to pass gas, and more. These issues warrant prompt medical evaluation.
Everyone will experience feeling a bit backed up at some point in their lives. You want nothing more than to “go,” but you simply can’t—or maybe a bowel movement feels incomplete, like there’s still something left behind.
Sometimes constipation can occur because of stress. Or it can be caused by a change in your diet, such as getting less fiber or fluids for a few days, or from a deviation from your routine, such as when traveling. Hey, it happens; one of my friends has even coined the hilarious yet accurate term, “home bowl advantage.” This describes the phenomenon of your intestines seeming to lock up the minute you get on a plane or head out on a road trip—but then, finally, you can go again when your body senses you’re back in the comfort of your own home.
Occasional constipation is relatively normal, but about 16 percent of adults in the United States experience frequent constipation; that rate goes up to 33 percent for those over age 65. Those assigned female at birth are also more prone to difficulty with going number two.
Although uncomfortable and certainly frustrating, constipation that occurs occasionally is not a medical concern. But you may be wondering when constipation or related gastrointestinal (GI) symptoms cross over into chronic territory, or when constipation warrants urgent or ongoing medical intervention. The distinction can be tricky, especially since everyone’s “normal” is a bit different when considering poop habits.
In this article, we’ll explore constipation danger signs and complications, what causes constipation and the different types, and how to find relief from constipation pain and discomfort.
What is constipation?
The concept of constipation might seem simple in that it means you are having difficulty with regularity, but the definition of constipation is a bit more involved than that. First, let’s explore the symptoms.
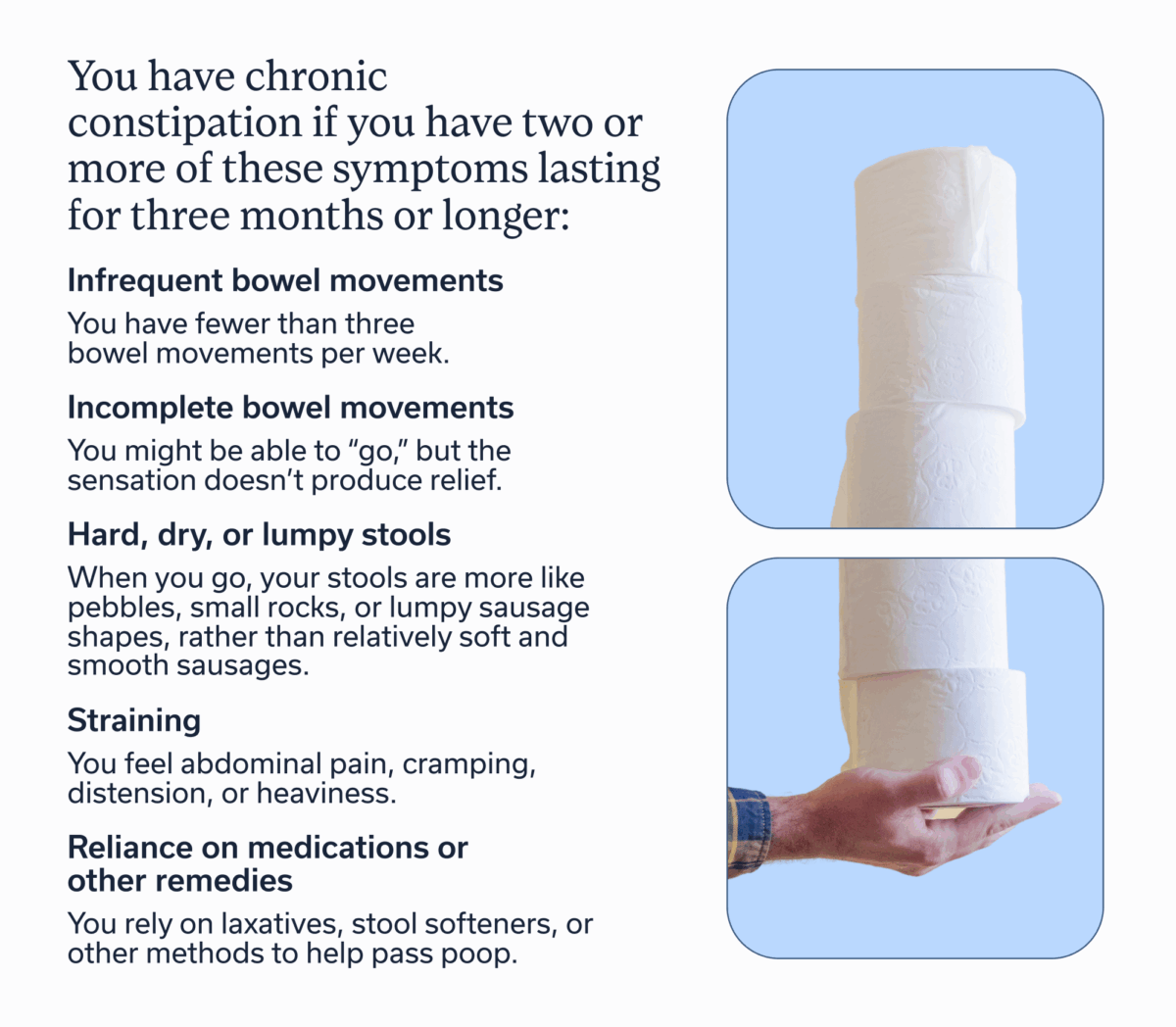
You have chronic constipation if you have two or more of these symptoms lasting for three months or longer.
- Infrequent bowel movements: You have fewer than three bowel movements per week.
- Incomplete bowel movements: You might be able to “go,” but the sensation doesn’t produce relief.
- Hard, dry, or lumpy stools: When you go, your stools are more like pebbles, small rocks, or lumpy sausage shapes, rather than relatively soft and smooth sausages.
- Straining: You have to bear down extensively to have a bowel movement.
- Bloating and discomfort: You feel abdominal pain, cramping, distension, or heaviness.
- Reliance on medications or other remedies: You rely on laxatives, stool softeners, or other methods to help pass poop.
Keep in mind that bowel habits are a bit different for everyone. While one factor of constipation is having fewer than three bowel movements per week, you might feel uncomfortable with fewer than five. That’s why shape and texture (stool type) may be a more helpful indicator. You can determine your stool type on the Bristol Stool Form Scale, which categorizes seven types of stool. Types 1 and 2 indicate constipation.
Oddly, diarrhea can also sometimes be a sign of constipation if it’s paradoxical (aka overflow) diarrhea. This occurs when a hard mass of stool blocks the rectum, but feces and mucus build up behind the blockage, sometimes leading to the leakage of watery stool around the mass.
Constipation falls into three sub-categories:
- Functional: You have infrequent and difficult bowel movements that have no structural cause. Instead, various non-structural factors may be contributing, such as miscommunication between the gut and brain.
- Chronic idiopathic: You have irregular and difficult bowel movements but with no evident underlying factors or causes.
- Secondary constipation: You experience constipation from specific causes, whether medications, underlying conditions, dietary factors, and more.
Common causes of constipation
The causes of constipation also fall into several categories:
- Primary or idiopathic: This type of constipation, where the cause is unknown and not a symptom of another disease, falls into three categories.
- Normal-transit constipation: Stool moves through the colon at a normal rate, but you still experience bowel movement trouble. This is often a sign of disrupted gut-brain communication.
- Slow-transit constipation: Stool moves through the colon at a slower-than-normal rate.
- Pelvic floor dysfunction: The pelvic floor muscles do not work correctly as a result of pregnancy or childbirth, obesity, pelvic surgery or injury, etc.
- Dietary: Inadequate fiber or water intake can cause constipation, as can overconsumption of certain beverages, such as coffee, caffeinated tea, or alcohol.
- Anatomical: Structural causes—including hemorrhoids, a narrow anal canal, a tumor, etc.—can sometimes lead to constipation. Even a retroverted or incarcerated uterus can be a culprit.
- Abnormal musculature: Some underlying conditions or congenital abnormalities that affect abdominal muscles can cause constipation, including Down syndrome, muscular dystrophy, gastroschisis, and more.
- Neurological: Neurological conditions—such as Parkinson’s disease, multiple sclerosis (MS)—and abnormalities in neurological structure of the intestines can also lead to difficulty with bowel movements.
- Medications: Constipation can be a side effect of a medication or recreational drug.
- Metabolic or endocrine: Some metabolic or endocrine disorders, including diabetes, can contribute to constipation.
- Miscellaneous: Other causes of constipation get lumped into the miscellaneous category and include, celiac disease, inflammatory bowel disease (IBD), cystic fibrosis, and more.
When is constipation considered dangerous?
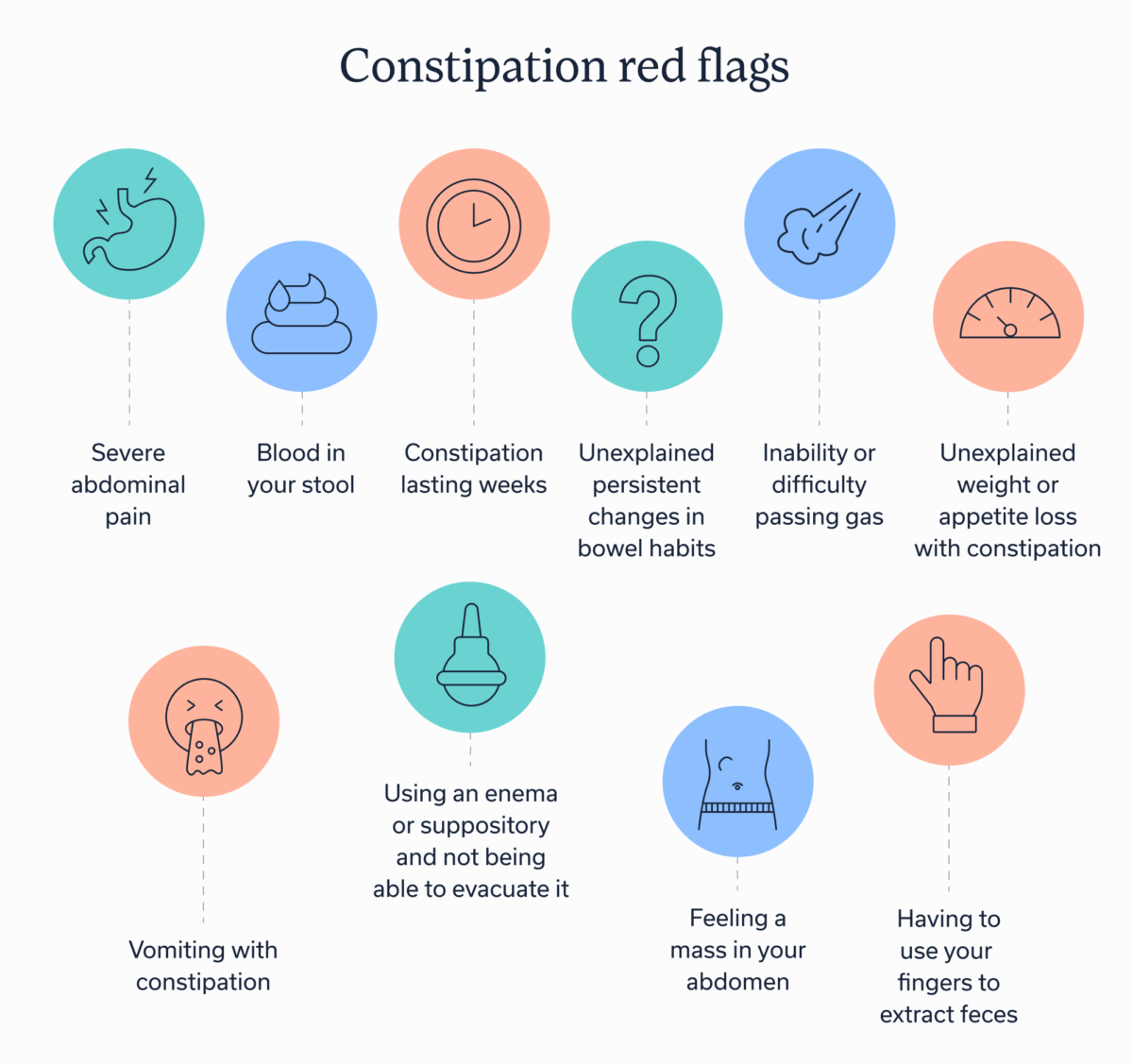
You may be wondering what are the red flags, or even yellow caution signs, of constipation that warrant seeking prompt medical attention.
Of course, you don’t have to have warning signs to talk to a provider about your bowel habits. If you frequently deal with constipation or have discomfort, talking to a knowledgeable provider is always a good idea. They can evaluate your symptoms, medical history, and more—and then formulate a treatment plan to help you find relief. An even more comprehensive way to get care is to consult with a team of GI specialists, such as those at Oshi Health, who are trained to take a whole-body approach to addressing your symptoms.
But if you have any of these red flags, don’t wait.
Constipation red flags
- Severe abdominal pain
- Blood in your stool
- Constipation lasting weeks
- Unexplained persistent changes in bowel habits
- Inability or difficulty passing gas
- Unexplained weight or appetite loss with constipation
- Vomiting with constipation
- Feeling a mass in your abdomen
- Having to use your fingers to extract feces
- Using an enema or suppository and not being able to evacuate it
Possible complications of severe constipation
When it comes to changes in your bowel habits, seeking treatment early is important because severe and chronic constipation can lead to the following complications.
- Hemorrhoids: swollen veins in the anus or rectum
- Anal fissures: a tear or crack in the anal lining
- Fecal incontinence: pooping or leaking in your underwear
- Urinary retention: inability to urinate or urinate fully
- Pelvic floor damage: damage to the muscles of the pelvic region
- Stercoral perforation: rupture of the intestinal wall
- Rectal prolapse: when the lower part of the large intestine protrudes from the anus
- Volvulus: when a section of the intestine kinks or twists
- Fistula-in-ano: an abnormal tunnel-like connection between the anal canal and surrounding skin
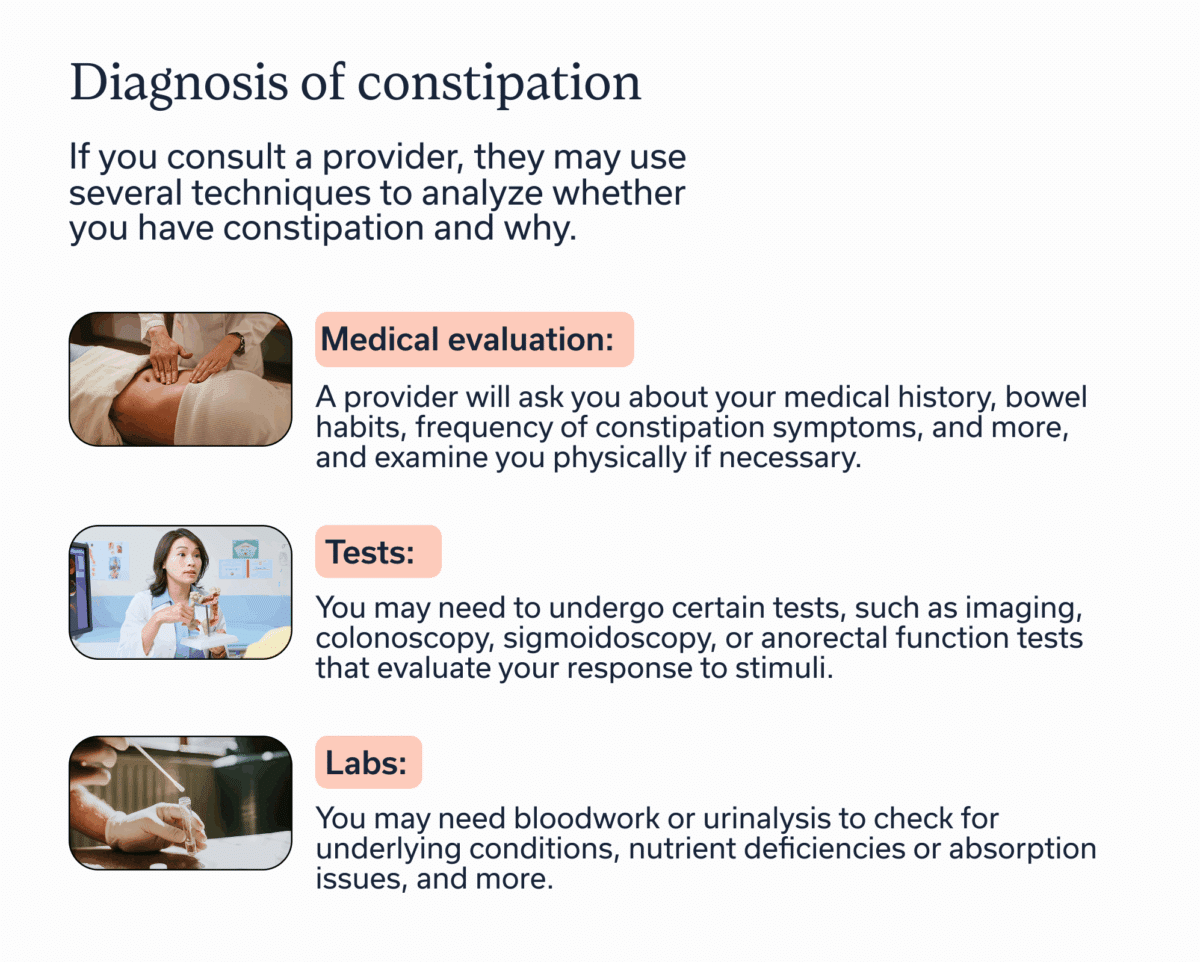
Diagnosis of constipation
If you consult a provider, they may use several techniques to analyze whether you have constipation and why.
- Medical evaluation: A provider will ask you about your medical history, bowel habits, frequency of constipation symptoms, and more, and examine you physically if necessary.
- Tests: You may need to undergo certain tests, such as imaging, colonoscopy, sigmoidoscopy, or anorectal function tests that evaluate your response to stimuli.
- Labs: You may need bloodwork or urinalysis to check for underlying conditions, nutrient deficiencies or absorption issues, and more.
Treatment options for constipation
The treatment options that work best for you will depend on your specific symptoms, the type of constipation you have, any underlying causes, and more. That’s why working with a GI provider who can help you understand your presentation of constipation and how to find relief can be so helpful. These are some general solutions, but an individualized approach is best.
Accessible digestive care
Get proven, whole-person GI care—in-network with many major health plans

Lifestyle, diet, medication and other non-surgical treatment options
- Stay hydrated: Hydration aids with intestinal motility, so drink plenty of fluids throughout the day. Water is the ideal choice, but natural (no sugar added) fruit juice and clear soups also help with hydration. Although you may have heard the “drink 64 ounces of water a day” myth, the actual recommended amount depends on age, sex, breastfeeding status, and activity level.
- Eat plenty of fiber: Fiber has many positive effects on the gut, including bulking stool for sending it through the digestive tract. However, increase fiber slowly over time to avoid discomfort. Aim for at least 25 grams if you’re female and 38 if you’re male. Keep in mind that too much fiber, especially in the absence of hydration, can paradoxically contribute to constipation. That’s why talking to a GI registered dietitian may be of benefit; they can help you dial in your fiber needs.
- Engage in physical activity: Movement helps keep things moving. Aim for 150 minutes of moderate-intensity or 75 minutes of vigorous-intensity activity per week.
- Change your toileting routine or posture: Simple changes, such as allowing more time to use the bathroom in the morning or adding a defecation postural modification device that puts in you a squatting position may help.
- Manage mental health: Stress, anxiety, and inadequate sleep can all contribute to constipation. Focusing on these aspects and treating any underlying mental health conditions may get you off the constipation train.
- Improve gut-brain communication: Conditions such as irritable bowel syndrome (IBS) are often rooted in disrupted gut-brain interaction. Working with a gut-brain specialist can help improve this communication.
- Consider supplements: Some supplements, such as magnesium, can help draw water into the bowel for more regularity. A provider can recommend which type and how much to take based on your unique needs.
- Try over-the-counter solutions: Some OTC options may include stool softeners, osmotic laxatives, and more. However, stimulant laxatives should only be used sparingly so as to avoid dependence. Again, consulting a provider on what to use, when, and how often is a great idea.
- Ask your doctor about prescription medications: In some cases, you may need a prescription for neuromodulators or secretagogues, especially if you have IBS.
Surgical treatment options and other medical procedures
Sometimes surgery or other procedures are necessary to resolve severe constipation. In the case of fecal impaction, where hardened stool blocks the colon or rectum, a provider will gently break up impacted stool with a lubricated gloved finger.
In other cases, surgery may be required to dislodge fecal impaction or fix a structural concern. Surgery (colectomy ) is only considered for non-anatomical causes of constipation, when all other conservative options are exhausted and the constipation is severe. Your provider will explore conservative options before recommending a more invasive intervention if necessary.
Key takeaways
- While mild occasional constipation often resolves on its own, frequent, ongoing, or severe constipation warrants an evaluation with a knowledgeable medical professional.
- Constipation danger signs include abdominal pain, blood in your stool, persistent changes in bowel habits, and more, and these symptoms require prompt medical evaluation.
- How to get rid of constipation will depend on the underlying cause and your unique circumstances.
Seek treatment with a GI provider, such as the specialists at Oshi Health, if you are experiencing chronic constipation, with or without additional warning signs.
Meet Oshi Health
An integrated team of GI specialists, working together for you
Our expert gastroenterologists, GI providers, registered dietitians, and gut-brain specialists are leaders in their fields, with advanced education and training in gastroenterology. Our comprehensive team approach is personalized to meet your unique needs and address the root cause of your symptoms.
FAQ
-
You may be dangerously constipated and should talk to a clinician right away if you are experiencing any of the following symptoms:
- Severe abdominal pain
- Blood in your stool
- Constipation lasting weeks
- Unexplained persistent changes in bowel habits
- Inability or difficulty passing gas
- Unexplained weight or appetite loss with constipation
- Vomiting with constipation
- Feeling a mass in your abdomen
- Having to use your fingers to extract feces
- Using an enema or suppository and not being able to evacuate it
-
If you are experiencing extreme constipation, you should talk to a knowledgeable GI provider who can evaluate and treat you and help you find relief as soon as possible. They will also do testing to rule out anatomical causes of constipation, such as obstruction from tumors.
If you have mild to moderate constipation, consider some of the non-surgical treatment options recommended in this article, including boosting hydration, fiber, and physical activity or trying an over-the-counter solution, such as a stool softener, or taking a supplement, such as magnesium.
-
How much water you need to drink to relieve constipation will depend on the underlying cause of your symptoms. However, ensuring you are getting at least nine 8-ounce cups if you’re female and 13 if you’re male is a good rule of thumb for adequate daily hydration. But you may need more water if you’re highly active.
-
As mentioned above, if you are experiencing extreme constipation, you should talk to a knowledgeable GI provider who can evaluate and treat you and help you find relief as soon as possible. If you have mild to moderate constipation, consider some of the non-surgical treatment options recommended in this article, including boosting hydration, fiber, and physical activity or trying an over-the-counter solution, such as a stool softener, or taking a supplement, such as magnesium.
-
If you haven’t pooped in two weeks, you could be experiencing fecal impaction or intestinal blockage and should consult a clinician right away. But don’t wait two weeks. Only you know what’s normal for you in terms of how regularly you go number two. If you notice a change in your bowel habits, you should consult your provider.
Oshi is your partner in digestive health
Feel like your digestive concerns are running your life? You’re not alone—and we’re here to help you find lasting relief.
Oshi Health GI providers, gut-brain specialists, and registered dietitians work together to address your symptoms and find solutions that actually work for you.
Whether you’re dealing with chronic digestive issues or unpredictable symptom flare-ups, our GI specialists deliver:
✔ Personalized care plans tailored to your lifestyle
✔ Science-backed strategies to calm your gut
✔ Compassionate, whole-person care
✔ And so much more!
Ready to take control of your gut health?