Got sudden or persistent lower abdominal pain? Understandably, you might be searching for what could be causing your discomfort. Is it a digestive, gynecological, urinary, or other issue? Indeed, the topic of lower abdominal or pelvic pain is tricky, especially for females, as several possibilities could be responsible, some that even overlap.
To put it bluntly, us females have a lot of parts in our abdominal and pelvic area. When pain crops up, whether suddenly or regularly, your mind starts with the questions. Is it something you ate? Is it menstrual cramps? Is your appendix going rogue? Is it something more serious? Is it all of the above? Okay, that would be rare, but you get the idea. The possibilities can be hard to pin down without further investigation.
Sometimes lower abdominal pain is just a temporary, minor issue, perhaps a side effect of a recent meal that your system didn’t”agree” with. In these cases, it generally resolves on its own.
Pelvic discomfort that is sudden and intense and doesn’t resolve, or that is ongoing or returns regularly, is not normal, though, and you shouldn’t have to”just live” with the pain. In fact, you could be experiencing a medical emergency, especially in instances where pain is intense and sudden. We don’t say that to scare you, only to raise awareness of the possibilities.
Chronic pelvic pain is common, however, affecting up to about 27 percent of people assigned female at birth. Regardless of the cause, if your pain doesn’t resolve, talking to a clinician as soon as possible—right away in some cases—is always a good idea to get to the root cause.
As noted, possibilities include gastrointestinal (GI), reproductive, or urinary issues, a combination of these, or even a concern with the nerves and muscles of the pelvis. Yes, that’s a thing! Pelvic floor dysfunction (PFD) is a common contributor to pelvic pain, and it often overlaps with underlying GI, urinary, and reproductive conditions.
In this article, we explore female abdominal pain, its potential causes, when to see a doctor—whether soon or immediately—and more.
Understanding lower abdominal pain in females: Why it’s complicated
First, let’s get on the same page about our anatomy and what the abdomen contains. Thinking of it in three sections helps.
-
Upper abdomen: This region contains your liver, gallbladder, pancreas, spleen, stomach, the duodenum (first part of the small intestine), adrenal glands, and the upper portion of the kidneys.
-
Middle abdomen: This area holds your small intestine, transverse colon, the lower portions of the kidneys, and the ureters.
-
Lower abdomen: This section contains the urinary bladder, sigmoid colon, rectum, appendix, uterus, ovaries, fallopian tubes, and upper vaginal area.
Sometimes people think of the abdomen as the stomach region, but we wanted to clarify that if you’re having pain in your lower abdominal region, your stomach isn’t the culprit, since that’s higher up. If you’re wondering, “Why does my stomach hurt?” or you have lower stomach pain or stomach cramps in general, then the concern isn’t lower abdominal or pelvic pain, and this article may not be helpful to you. This piece focuses on pain in your lower abdomen or pelvis. Want info on stomach pain? Check out this piece.
In the lower abdomen, the reproductive organs, urinary organs, and parts of the gastrointestinal (GI) tract hang out together. They have overlapping nerves, major blood vessels, and more. So pinpointing the cause of your lower abdominal pain can be complex, but a knowledgeable clinician can look at your symptoms, the patterns they follow, and more to narrow in on the concern.
Complicating matters is that more than one issue could be going on. For example, irritable bowel syndrome (IBS) is common in people with endometriosis, a systemic inflammatory condition that sometimes presents with severe pelvic pain.
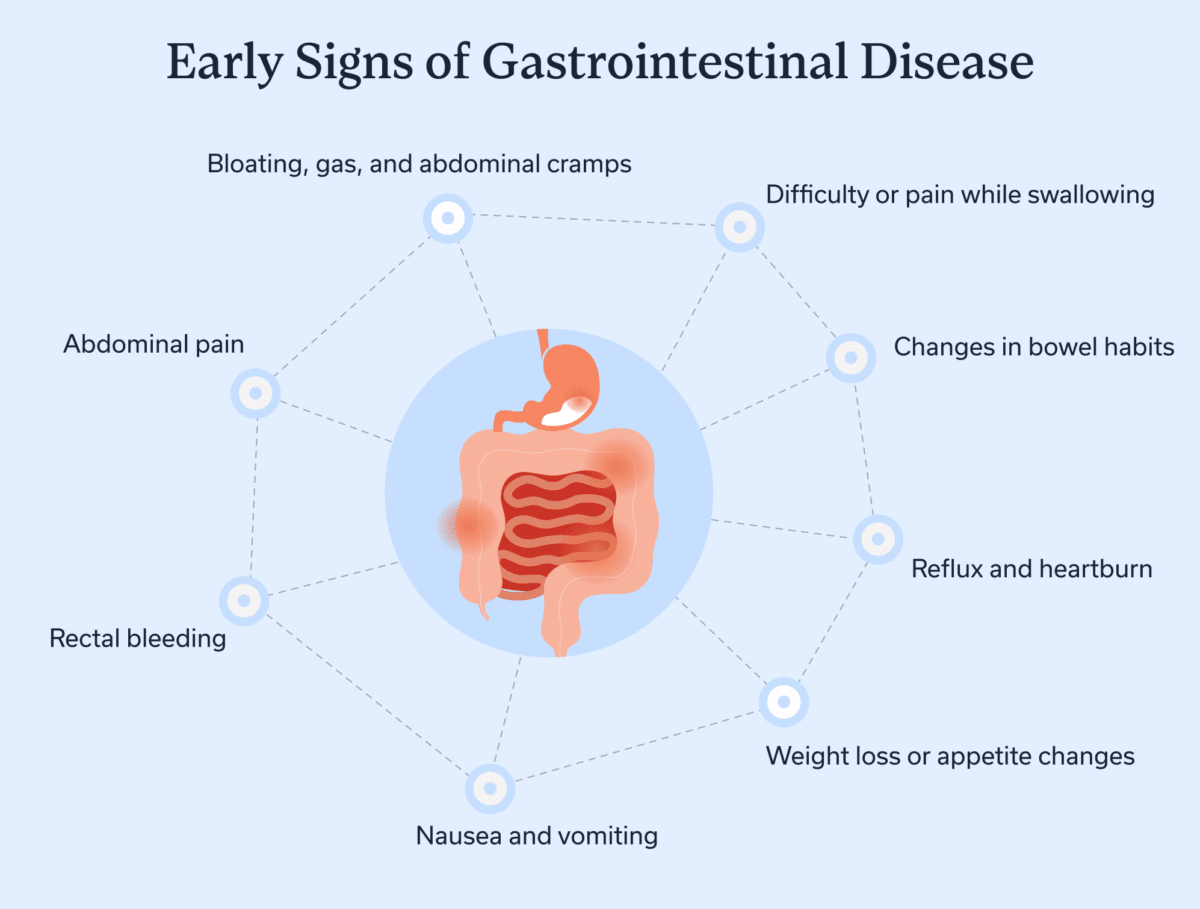
Common GI causes of lower stomach pain
In this section, we will explore issues associated with the GI tract. These might be to blame for your lower abdominal pain. However, just because you have discomfort in this general area doesn’t mean you have one of these conditions.
Constipation or diarrhea
Bowel habits are a bit different for everyone, but if you are having infrequent number two episodes and pain, cramping, or bloating, you might be experiencing constipation. And if you are noticing loose or watery stools, with cramping, you might be experiencing diarrhea. Nearly everyone will experience occasional bouts of either constipation or diarrhea. But if either is ongoing, talking to a provider is a good idea to address underlying causes.
Infection or temporary inflammation
Lower abdominal pain is sometimes a sign of an acute infection, inflammation, or both. For example, gastroenteritis (sometimes referred to as”the stomach flu”) is inflammation of the GI tract. Bacteria, viruses, or parasites can cause this type of trouble.
Food poisoning is a type of gastroenteritis, but not all gastroenteritis is food poisoning. Food poisoning occurs when you eat something contaminated with pathogens.
Gastroenteritis often resolves on its own within a few days with rest, a bland diet, and adequate hydration. If you can’t keep fluids down or are experiencing significant diarrhea or vomiting, blood in your stool or urine, or a high fever, seek medical attention.
Irritable bowel syndrome (IBS)
IBS can cause constipation, diarrhea, or a mix of the two, and abdominal discomfort is a common characteristic. IBS is typically caused by disruptions in communication between the gut and brain. Your gut and brain communicate along what’s called the gut-brain axis. But sometimes this communication doesn’t work so well. Working on the gut-brain connection with the help of a specialist can help.
Diverticulitis or diverticulitis
Diverticulosis and diverticulitis are two related conditions that can affect your digestive tract.
-
Diverticulosis occurs when diverticula (small pouches) form in your intestinal walls. They develop when the intestinal lining pushes into weak spots in the outer wall due to increased pressure. Having diverticulosis means you have these small pouches. But most of the time, diverticulosis doesn’t cause symptoms.
-
Diverticulitis occurs when one or more diverticula become inflamed, often due to a bacterial infection, which may cause pain and other symptoms. If an infection is present, diverticulitis requires antibiotic treatment; antibiotics are typically reserved for complicated diverticulitis.
Inflammatory bowel disease (IBD)
IBD is an umbrella term for diseases including Crohn’s disease and ulcerative colitis, both chronic inflammatory conditions that can cause damage to the GI tract. Flares often involve abdominal pain and a host of GI symptoms.
Appendicitis
Appendicitis means inflammation of the appendix. This can cause lower abdominal pain ,typically in the right side, sometimes along with other GI symptoms and a fever. If you suspect appendicitis, seek immediate medical attention. The organ can rupture and cause peritonitis, severe inflammation of the abdominal lining.
Colorectal cancer
Although generally less common than the other conditions mentioned in this section, colorectal cancer deserves a mention. It is the third most diagnosed cancer in the United States. The early stages of colorectal cancer may not present any symptoms, but abdominal pain can be a warning sign. So if your pain continues, be sure to get checked out.
Pelvic floor dysfunction(PFD): An overlooked cause of lower abdominal and pelvic pain
PFD is a significant contributor to pelvic pain and back pain, especially in people assigned female at birth. It occurs when you can’t fully relax, tense, or otherwise coordinate the muscles in your pelvis. The pelvis is shaped like a bowl, and the pelvic floor muscles make up the bowl’s base.
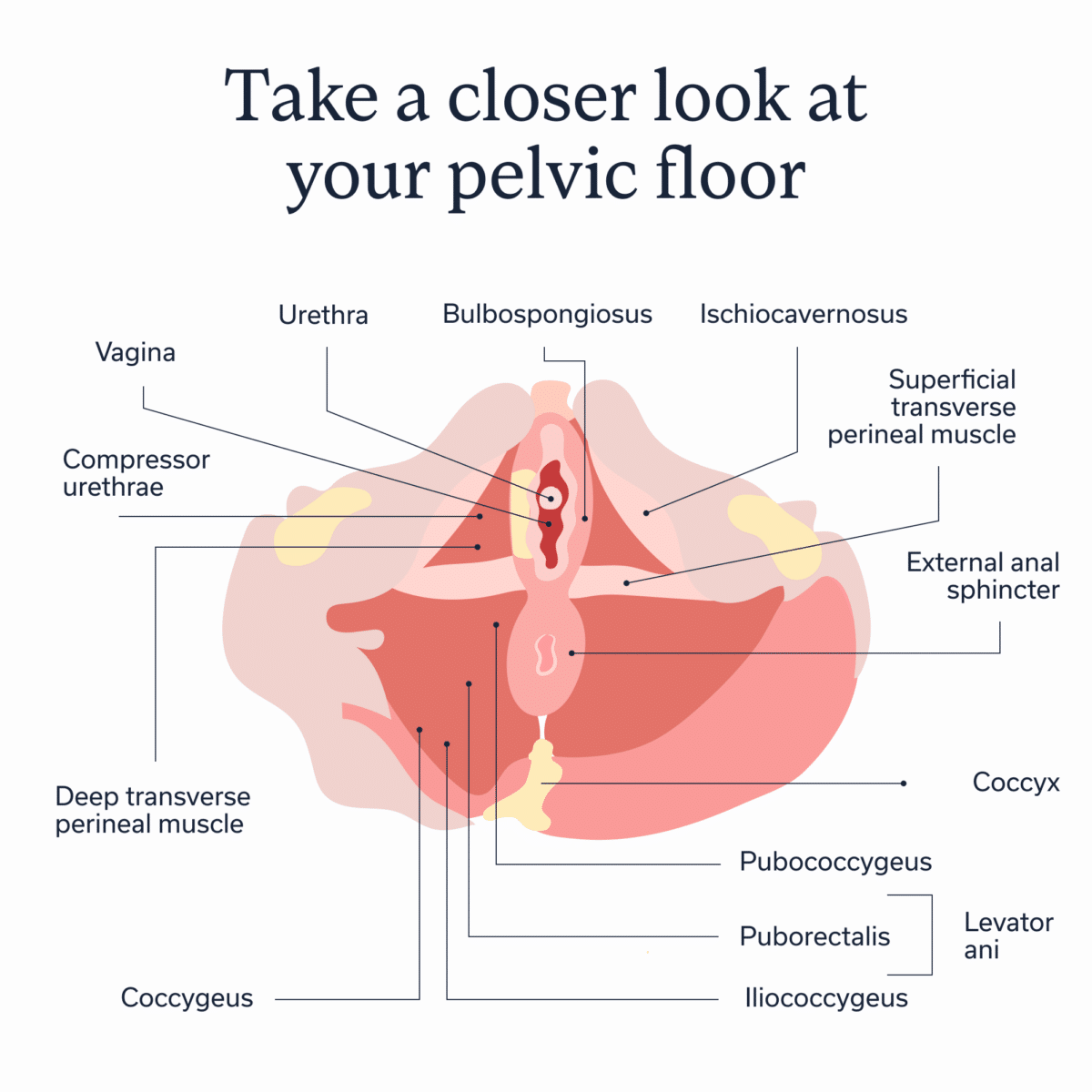
This group of muscles and other connective tissue support your pelvic organs, including your bladder, bowel, and uterus. These muscles perform several functions, including helping you to poop and pee. They also contribute to your sexual function and help maintain continence so you don’t have bladder or bowel leaks. Risk factors for PFD include childbirth, chronic constipation, pelvic surgery, obesity, and more.
PFD overlaps with several of the conditions mentioned throughout this article, especially constipation, diarrhea, and IBS. Additionally, PFD shares associations with several non-GI causes of abdominal pain.
Non-GI causes of female abdominal pain to keep in mind
With your reproductive organs also in your pelvis, lower abdominal pain isn’t necessarily a GI issue. Here are some common conditions affecting reproductive and urinary health. Keep in mind that these conditions can overlap with both acute and chronic GI symptoms.
Menstrual cycle pain
You’ve probably heard of premenstrual syndrome (PMS), which involves symptoms related to your menstrual cycle that typically show up in the week leading up to and even during your period. Some minor menstrual cramping and discomfort or feeling a bit under the weather during this time is normal, but intense pain or cramping is not. Never hesitate to talk to a clinician about your symptoms, as you could have one of the conditions mentioned below.
By the way, you might also experience minor cramping or twinges of discomfort around the time of ovulation, a sensation called mittelschmerz. The pain can be minor or somewhat intense, but it should be temporary. You might wish to track cramping or other symptoms throughout the month to see if you notice a pattern.
Premenstrual dysphoric disorder (PMDD)
PMDD is a severe form of PMS, and it’s classified as a mental health condition because of intense mood changes that can occur, typically in the second half of the menstrual cycle, known as the luteal phase. PMS symptoms, such as cramping and bloating, can also be more intense.
Urinary tract infection (UTI) or bladder infection
A UTI or bladder infection can cause pelvic pressure, pain, or discomfort. These infections require treatment, typically with an antibiotic.
Endometriosis
Endometriosis is a systemic inflammatory condition in which tissue that mimics the endometrium (the uterine lining) grows outside of the uterus on other organs and tissues. Although endometriosis lesions have been found in nearly every organ system—including the heart, lungs, and brain—it’s most commonly found in the pelvis. Severe pelvic pain is a common symptom.
Polycystic ovary syndrome (PCOS)
PCOS is an endocrine and reproductive health condition affecting the ovaries. Hormonal disruptions and imbalances can lead to the development of several immature follicles, which may appear as cysts on imaging tests. One or both ovaries may also become enlarged. PCOS often affects fertility. And it can cause lower abdominal pain, bloating, and other symptoms.
Ovarian cyst rupture
Sometimes an ovarian cyst (a fluid-filled sac) can rupture, causing lower abdominal pain. Some ovarian cysts are normal and called functional cysts, while others are abnormal. All can potentially rupture and cause intense discomfort. If you experience sharp abdominal pain or pain with ongoing dizziness, weakness, or nausea, seek medical attention. An ovarian cyst can cause torsion (forcing the ovary to twist), potentially cutting off the blood supply to the tissue. Ovarian torsion is a medical emergency.
Uterine fibroids
Uterine fibroids are benign (noncancerous) growths that appear in and around the uterus. They can lead to pressure, pain, bloating, and more. They can also cause heavy or lengthy periods and irregular bleeding.
Ectopic pregnancy
An ectopic pregnancy occurs when a fertilized egg implants outside of the uterus. Most often, this occurs in the fallopian tubes. Symptoms include sharp or intense one-sided pelvic pain or cramping, and sometimes vaginal bleeding or spotting. An ectopic pregnancy is a life-threatening medical emergency.
When to seek care
Seek care right away if intense lower abdominal pain comes on suddenly and does not resolve. Also seek care for chronic pelvic pain, whether it comes and goes or sticks around continuously.
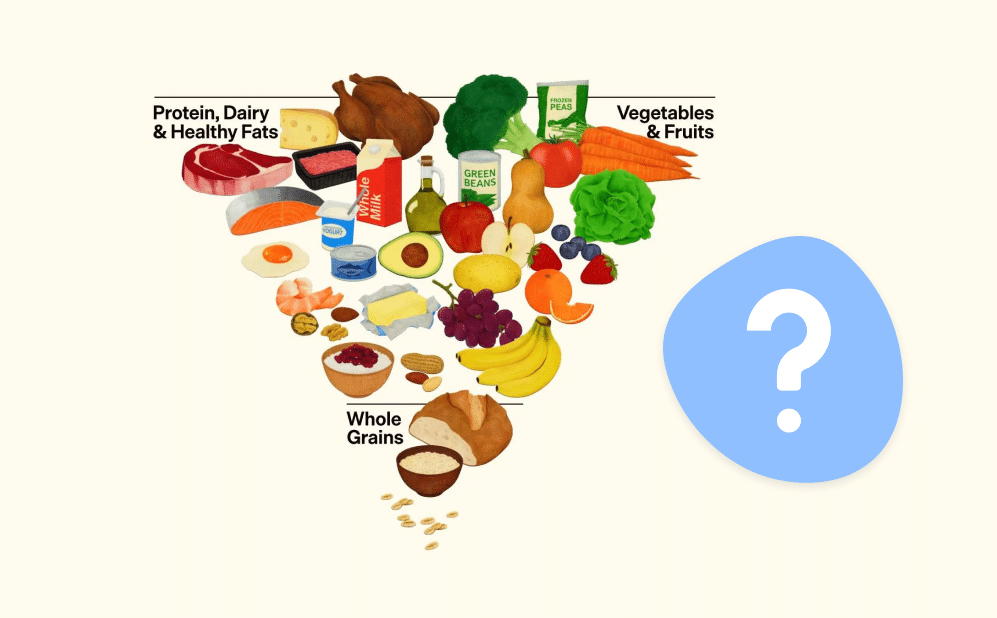
If your condition is GI-related or overlaps with the GI system, Oshi Health can help. They can also help you determine if you need to see another type of clinician.
Oshi Health provides multidisciplinary care for whole-person comprehensive GI health. Your care team might include a GI provider (a nurse practitioner or physician associate), a GI registered dietitian, and/or a gut-brain specialist, all overseen by board-certified gastroenterologists . They collaborate to help you improve your gut health and manage chronic conditions. You’ll have access to unlimited virtual visits with your care team, with appointments available within days.
Key takeaways
-
Lower abdominal pain in females could be GI, urinary, reproductive, or nerve and muscle-related, or it could be a combination of concerns.
-
But lower abdominal pain that is severe or ongoing isn’t normal, and in some cases, you might need immediate medical attention.
-
For ongoing issues, Oshi Health can help, especially for GI-related issues or those that may overlap with other pelvic health conditions.
FAQ
-
If you are assigned female at birth and experiencing lower abdominal pain that is sudden, intense, and doesn’t resolve within a short time, seek immediate medical attention. If you are experiencing chronic pelvic pain, talk to a knowledgeable clinician to get to the root cause.
-
Five causes of abdominal pain in females include GI conditions or symptoms, reproductive health concerns, issues with urinary organs, pelvic floor dysfunction, and a combination of these concerns.
-
If you are female and have lower abdominal pain, the relief methods you need will depend on the underlying cause of the pain. If your pain is intense, sudden, and doesn’t resolve quickly, seek medical attention right away. In other cases, talk to a knowledgeable clinician as soon as possible about your symptoms so you can get to the root cause and feel better.
Oshi is your partner in digestive health
Feel like your digestive concerns are running your life? You’re not alone—and we’re here to help you find lasting relief.
Oshi Health GI providers, gut-brain specialists, and registered dietitians work together to address the root cause of your symptoms and find solutions that actually work for you.
Whether you’re dealing with chronic digestive issues or unpredictable symptom flare-ups, our GI specialists deliver:
✔ Personalized care plans tailored to your lifestyle
✔ Science-backed strategies to calm your gut
✔ Compassionate, whole-person care
✔ And so much more!
Ready to take control of your gut health?