Diverticulosis is a condition in which small pouches develop in your intestinal wall. Diverticulitis is when one or more of these pouches becomes inflamed or infected. You can think of diverticulosis as a chronic condition and diverticulitis as more of a flare up. Read on to learn more about the key differences.
The digestive tract starts with your mouth and ends with your anus. It sends water and nutrients and eventually waste on a long and winding path through your body. Unfortunately, sometimes things go wrong with it, leading to uncomfortable symptoms, including abdominal pain.
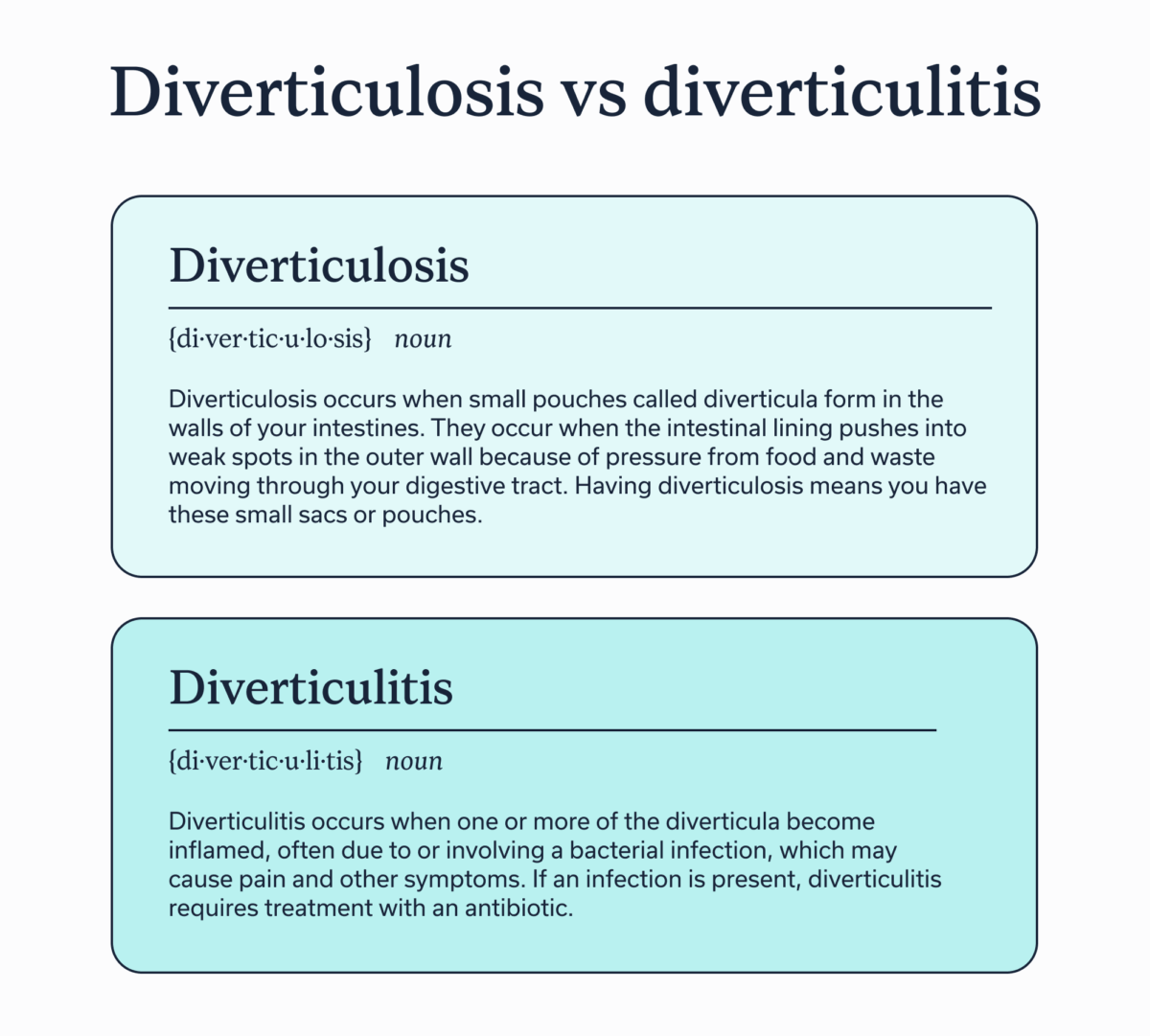
Diverticulosis and diverticulitis are two related conditions that may impact your digestive tract, but their names are sometimes confusing since they sound so similar.
In this article, we explore the difference between diverticulitis and diverticulosis, symptoms to watch for, treatments, and more.
Diverticulosis vs diverticulitis: the core differences
Diverticulosis occurs when small pouches called diverticula form in the walls of your intestines. They occur when the intestinal lining pushes into weak spots in the outer wall because of pressure from food and waste moving through your digestive tract. Having diverticulosis means you have these small sacs or pouches.
Generally, most diverticulosis is asymptomatic, meaning you may not even know you have the condition. (Sometimes a routine colonoscopy can reveal that you have it.)
Diverticulosis is common and generally not cause for concern unless you experience discomfort or other gastrointestinal (GI) symptoms, or you frequently develop diverticulitis.
Diverticulitis occurs when one or more of the diverticula become inflamed, often due to or involving a bacterial infection, which may cause pain and other symptoms. If an infection is present, diverticulitis requires treatment with an antibiotic.
You might come across another related term: diverticular disease, which is the experience of having symptomatic diverticulosis.
Diverticulitis can be uncomplicated or complicated:
-
Uncomplicated: This means the diverticula are inflamed but not causing any of the extra issues listed below, though you may still have pain or discomfort. This is the most common type of diverticulitis, accounting foroccurring in about 80% of cases.
-
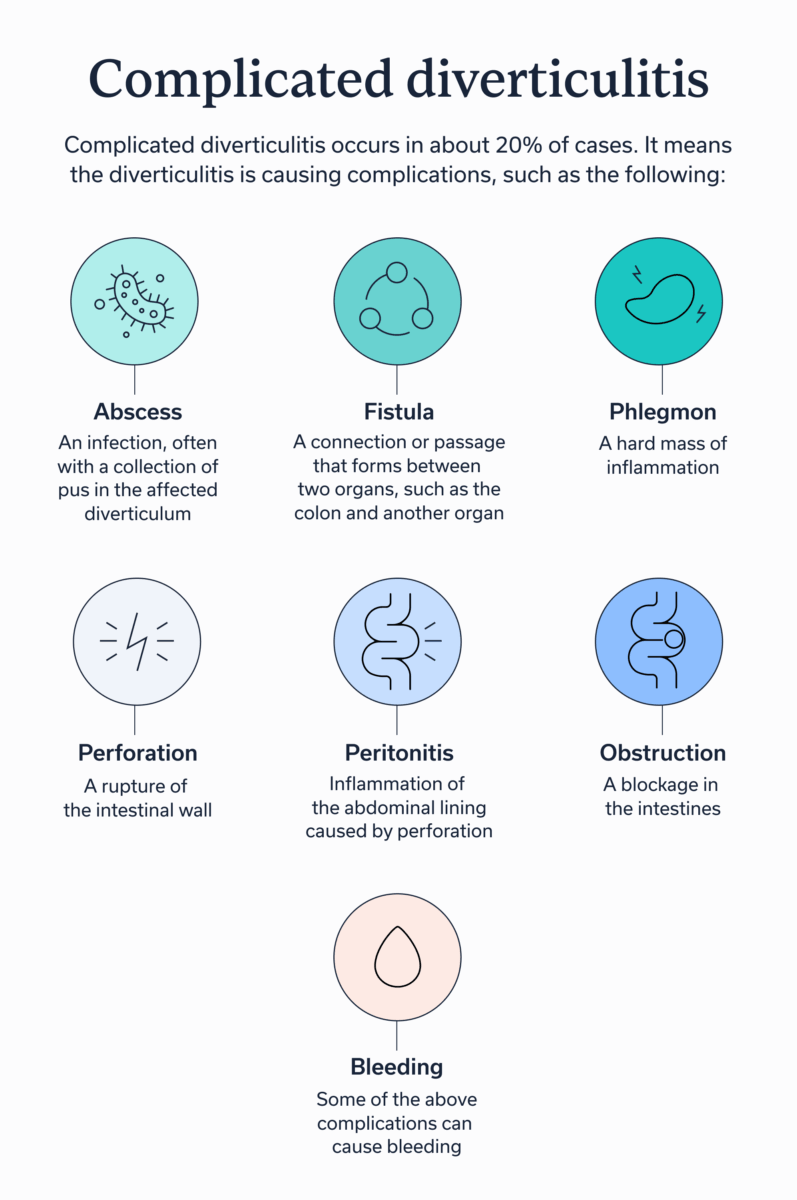
Complicated: Complicated diverticulitis occurs in about 20% of cases. It means the diverticulitis is causing complications, such as the following:
-
Abscess: An infection, often with a collection of pus in the affected diverticulum
-
Fistula: A connection or passage that forms between two organs, such as the colon and another organ
-
Phlegmon: A hard mass of inflammation
-
Perforation: A rupture of the intestinal wall
-
Peritonitis: Inflammation of the abdominal lining caused by perforation
-
Obstruction: A blockage in the intestines
-
Bleeding: Some of the above complications can cause bleeding
-
Colonic diverticulosis without diverticulitis: What it means
To understand this concept, a look at the terminology can help.
-
“Divert” means that the normal path through your intestines has a diversion, such as into a diverticulum., a small sac.
-
“Osis” is a suffix that means a medical condition is present.
-
” Itis ” is a suffix that means inflammation.
Having diverticulosis means you have this medical condition, but it’s not causing major complications.
Having diverticulitis means that you are experiencing a flare up of your condition and that inflammation is present.
So if you have colonic diverticulosis without diverticulitis, you have pouches in your colon, but they are not inflamed or infected.
Thinking about other medical conditions as an analogy can help you understand what this means. As an example, people with asthma have a chronic condition, but they don’t always experience symptoms or asthma attacks.
Who gets each and why?
Diverticulosis typically develops over time based on several risk factors:
-
Age
-
Genetics
-
High-fat diet
-
Obesity
-
Low-fiber diet
-
Sedentary lifestyle
-
Smoking
-
Taking certain medications, including non-steroidal anti-inflammatory drugs (NSAIDs), opiates, or steroids
In countries that follow a Western diet, including the United States, the prevalence of diverticulosis is less than 20% for people about age 40, but it goes up to 60% for those who are about 60. However, prevalence is on the rise, especially in people between the ages of 18 and 44. In people under age 50, the prevalence is slightly higher in people assigned male at birth, but those assigned female have a higher prevalence over age 50.
Why does aging sometimes lead to diverticulosis?
As you get older, the muscles in the intestinal wall can weaken or lose elasticity, making them more vulnerable to developing diverticula. Additionally, age can lead to slower motility, the movement of food and waste through the digestive tract. Reduced motility can lead to increased pressure that further weakens the intestinal wall. The average age of patients admitted to the hospital for diverticulitis is 63.
However, age is not the only contributor to diverticulosis. Another risk factor is a low-fiber diet, which can lead to constipation and straining that creates additional pressure. A lack of physical activity and having obesity can also contribute.
Diverticulosis is a risk factor for developing diverticulitis, which occurs in about 4% to 15% of people with the condition. The average age of patients admitted to the hospital for diverticulitis is 63.
Symptoms: How they typically present
As mentioned above, diverticulosis is often asymptomatic–but sometimes symptoms can occur. With diverticulitis, on the other hand, you will most likely experience notable symptoms.
Diverticulosis vs diverticulitis symptoms
Diverticulosis symptoms:
-
Blood in the stool, generally without experiencing pain
-
Changes in bowel habits
-
Unexplained abdominal pain or cramping
Diverticulitis symptoms:
-
Bloating and gas
-
Changes in bowel habits
-
Fatigue
-
Fever if an infection is present
-
Loss of appetite
-
Nausea or vomiting
-
Pain, generally in the lower left abdomen
-
Rectal bleeding
Keep in mind that the above symptoms are common in other GI conditions, so if you experience these issues, that does not necessarily mean you have diverticulosis or diverticulitis. However, if you do have unexplained symptoms, talking to a clinician is important so you can figure out what’s going on.
How clinicians diagnose each
Your clinician might use several tools to diagnose you with diverticulosis or diverticulitis.
-
Medical history: They may ask you about your underlying conditions, previous procedures, medications, supplements, lifestyle habits, and more. This helps your clinician understand more about your risk factors for diverticulosis.
-
Family medical history: From research looking twins, scientists have determined that about 50% of individual susceptibility to diverticulosis likely stems from genetic factors. So if someone in your family has diverticulosis, you may also be more at risk for it.
-
Physical exam: A physical exam may include checking your vital signs, feeling your abdomen, listening to bowel sounds with a stethoscope, or doing a rectal exam with a gloved finger.
-
Blood tests: Lab work can be helpful for looking at whether you have markers of inflammation or infection, both of which could indicate diverticulitis.
-
Stool tests: A stool test can help determine if you have rectal bleeding or a GI infection, which could indicate diverticulitis.
-
Imaging tests and procedures: These may include a computed tomography (CT) scan, magnetic resonance imaging (MRI), ultrasound, barium enema, flexible sigmoidoscopy or a colonoscopy to help your clinician determine if you have diverticula, which would indicate you have diverticulosis.
Treatment overview: by condition and severity
If you have diverticulosis without any symptoms, you may not need any specific treatments. However, your provider may recommend lifestyle changes to help reduce your risk of developing diverticulitis. (See the”living with diverticulosis” section.)
If you develop diverticulitis, you will likely need some form of treatment, but the type that is best for you will depend on your specific symptoms, whether you have an infection, how often you’ve had diverticulitis in the past, and more. Your treatment plan will be individualized to you based on these factors.
Non-surgical treatment options
-
Antibiotics: If you have an infection, you may need a course of antibiotics to resolve it. Mild cases of uncomplicated diverticulitis can be managed conservatively with bowel rest and no antibiotics, however. Plus, it’s important to note that not all cases of diverticulitis present with an infection.
-
Pain management: If you are experiencing pain, your clinician may prescribe a medication or recommend an over-the-counter option to help ease your discomfort.
-
Temporary dietary changes: You may need to be on a clear-liquid diet for a short time before slowly returning to eating more solid foods. This can give your intestines a chance to rest and recover from inflammation. In more severe cases, you may need to be on complete bowel rest and take in intravenous (IV) fluids only.
-
Abscess drainage: If you have any large pus-filled diverticula, your clinician may need to drain them via percutaneous drainage . This is a non-surgical treatment, but it is minimally invasive. Your provider will numb the affected area and use imaging tools to then insert a needle or catheter through the skin into the infected diverticula to drain the pus. Sometimes a drain may need to remain in temporarily.
-
Observation and monitoring: You may need to be temporarily hospitalized so that your doctor can monitor how you are doing. In other cases, if your symptoms aren’t severe and you don’t have an infection or you’re being treated with antibiotics, you might be able to remain at home for self-care while keeping in close contact with your doctor to alert them to any changes, such as the improvement or worsening of your symptoms.
Surgical treatment options
Surgical options may be necessary if you’ve had recurrent diverticulitis or experience complications.
-
Primary bowel resection: A bowel resection is the removal of the diseased portion of the intestine. Depending on the circumstances, your surgeon may connect the remaining portions of the bowel to restore normal function, or they may need to perform a colostomy. A colostomy creates an opening called a stoma to divert waste from the colon to outside the body for collection in a pouch that you can empty as needed. A colostomy can be permanent or temporary, with the temporary option often called a Hartmann’s procedure.
-
Laparoscopic lavage: This procedure involves the insertion of a laparoscope (small camera) through an incision in the abdomen. With other incisions, the surgeon inserts small tools to wash the abdominal cavity with saline to flush out any pus or blood. A laparoscopic lavage is only suitable if you’ve had a perforated bowel (rupture) and the perforation is now sealed off, leaving pus but not feces in the abdominal cavity.
-
Fistula repair: A fistula occurs when an abnormal opening forms from one organ to another, such as the colon to the vagina (colo-vaginal fistula) as just one example. If you experience a fistula, a surgeon will repair it.
Living with diverticulosis: prevention and reduction
Although lifestyle changes aren’t a cure for diverticulosis, they may help manage your condition and reduce your risk for developing diverticulitis.
-
Consume adequate fiber: A low-fiber diet is a risk factor for diverticulosis and diverticulitis. Fiber helps move food and waste through your digestive tract, which helps relieve intestinal pressure, and supports overall GI health. The recommended dietary allowance for fiber is 25 grams for females and 38 grams for males per day. You can get fiber from eating fruits and vegetables. However, if you have trouble getting enough fiber in your diet, you may need a fiber supplement, such as psyllium husk.
-
Maintain good hydration: Good hydration is crucial for overall health, and it’s especially important for GI health. When you up your fiber intake, be sure to drink adequate water. Nine cups daily for women and 13 cups for men is recommended, but fluid needs will vary from person to person.
-
Engage in regular physical activity: Exercise benefits your whole body, but movement can be especially important for supporting your GI tract . Living a sedentary lifestyle is a risk factor for diverticulosis. Adults need at least 150 minutes of moderate-intensity or 75 minutes of vigorous intensity exercise, along with at least two days of strength-training, per week.
-
Reduce your risk factors: Additional controllable risk factors for developing diverticulosis and diverticulitis include smoking and eating high-fat diet. If you smoke, talk to your provider about a cessation method that’s right for you. If you eat a high-fat diet, focus on consuming healthy fats, such as omega-3 fatty acids, found in fish, nuts, and seeds. Diet is highly individual, and you may benefit from working with a GI registered dietitian, such as those at Oshi Health, who can help you customize a diet to your unique nutritional needs and preferences.
When to seek care
You should talk to a clinician as soon as possible if you suspect you have diverticulosis or diverticulitis. The knowledgeable clinicians and care team at Oshi Health can help, and you can start the process from your own home. Book a virtual visit today.
That said, seek immediate medical attention if you notice the following”red flag” symptoms:
-
Abdominal or back pain that is sudden and severe
-
Blood in your stool
-
Difficulty or inability to pass gas or stools, which may indicate a bowel obstruction
-
Fecal matter expelled from the vagina, which may indicate a fistula
-
High fever (over 100.4 degrees Fahrenheit) or related chills
-
Perforation, which may present as a sudden sharp pain with abdominal distention and difficulty breathing
-
Unexplained nausea and vomiting
Key Takeaways
- Diverticulosis is a condition in which small pouches develop in your intestines.
- Diverticulitis is when one or more of the pouches become inflamed or infected.
- Diverticulosis may not cause any symptoms, but diverticulitis generally causes some GI issues.
- In some cases, diverticulitis can cause complications that are a medical emergency.
- The team at Oshi Health can help you manage diverticulosis and take steps to reduce your risk for diverticulitis.
FAQ
-
Diverticulosis is a condition in which small pouches develop in your intestines. Diverticulitis is when one or more of the pouches become inflamed or infected. Diverticulosis on its own is generally not cause for concern. However, diverticulitis can be serious and sometimes even a medical emergency.
-
Researchers don’t know the exact causes of diverticulitis, but pressure in the digestive tract seems to contribute to the development of small pouches in the intestinal wall. Risk factors include aging, a genetic predisposition, obesity, a low-fiber diet, a sedentary lifestyle, smoking, and taking certain medications.
-
Diverticulosis, which is when small pouches form in the intestinal wall, does not have a definitive cure. However, you can manage the condition with lifestyle changes that may help prevent the development of diverticulitis, which is when one of the small pouches becomes inflamed or infected.
Oshi is your partner in digestive health
Feel like your digestive concerns are running your life? You’re not alone—and we’re here to help you find lasting relief.
Oshi Health GI providers, gut-brain specialists, and registered dietitians work together to address your symptoms and find solutions that actually work for you.
Whether you’re dealing with chronic digestive issues or unpredictable symptom flare-ups, our GI specialists deliver:
✔ Personalized care plans tailored to your lifestyle
✔ Science-backed strategies to calm your gut
✔ Compassionate, whole-person care
✔ And so much more!
Ready to take control of your gut health?






