Nutrition plays a starring role in treating, and even possibly reversing, non-alcoholic fatty liver disease (NAFLD), a gastrointestinal disease caused by fat build-up in the liver. An effective fatty liver diet menu often consists of minimally processed whole foods, with plenty of fiber and lean protein. Here’s how to weave this diet into your lifestyle, with meal ideas you’ll actually enjoy.
Non-alcoholic fatty liver disease (NAFLD) is a chronic liver condition where fat builds up in the liver of people who drink little or no alcohol. It is usually symptomless, especially in early stages, but if left untreated, it can lead to scarring and inflammation in the liver. Over the last three decades, the prevalence of non-alcoholic fatty liver disease (NAFLD) has risen by over 50% . Today, about 38% of Americans have this condition, which is almost four out of every ten people. Despite how common NAFLD is, many people, including some with this condition, don’t understand how the right fatty liver diet menu can improve symptoms of the disease as well as overall quality of life.
“As a gastroenterologist, I wish more people understood how powerful nutrition and lifestyle is when it comes to fatty liver disease,” says Treta Purohit, MD, a gastroenterologist and hepatologist and Executive Medical Director at Oshi Health, “Fatty liver is far more common than most realize, and in many cases, it can be improved—or even reversed—through dietary and lifestyle changes alone.”
Understanding fatty liver disease and diet’s role
Though not the largest organ in the body (that title goes to the skin), the liver is the largest internal organ and one of the most vital. It helps metabolize food, process nutrients, and remove harmful substances, like alcohol. These aren’t just fun facts (though how the liver works is pretty amazing). They’re important for understanding the role this organ plays in digestion and overall health.
If the liver becomes overwhelmed, especially by diets high in saturated fat and added sugars, it may store excess fat, leading to non-alcoholic fatty liver disease (NAFLD). “NAFLD is a condition where fat builds up in the liver in people who drink little or no alcohol. It ranges from simple fat buildup to liver inflammation and damage, which can lead to cirrhosis or cancer,” says Dr. Purohit, “It’s mostly linked to obesity, type 2 diabetes, and insulin resistance.” Note that both nonalcoholic fatty liver (NAFL, the simple fat buildup Dr. Purohit is referring to) and nonalcoholic steatohepatitis (NASH, the more severe inflammation and damage) are types of nonalcoholic fatty liver disease.
While NAFLD increases the risk for liver inflammation and scarring, as well as complications like cirrhosis or liver cancer, it’s tricky to catch because NAFLD is often symptomless in early stages. If someone does experience symptoms early on, they’re usually upper abdominal pain or fatigue—both relatively minor symptoms that are likely to go unchecked but shouldn’t be dismissed.
Researchers are still looking into what causes NAFLD, but it’s most likely a mix of genetics, the presence of other health conditions, and lifestyle factors, including diet. Specific risk factors for this condition include:
- Being overweight or obese
- High cholesterol
- High levels of triglycerides, a type of fat that comes from butter, oils, and other fats
- Type 2 diabetes and/or insulin resistance
Diet influences all four, which is why being mindful about nutrition choices is essential for long-term liver health. The link between your diet and your liver is also why, if you do end up with NAFLD, your provider will likely recommend positive nutrition changes as part of your treatment.
Core principles of a fatty liver diet
There’s no such thing as one set “fatty liver diet.” But there are a few core principles that you can adjust to your own eating preferences:
- Add in fiber and lean protein: Fiber and lean protein keep us full longer and help with weight management, with fiber also offering added benefits for overall digestion. While these benefits don’t directly impact NAFLD, they do influence someone’s overall weight, and maintaining a healthy weight is important when managing NAFLD.
- Control portions: Excess calories and fat negatively impact liver function, so controlling portions is an effective way to address NAFLD. The ideal portion size depends on many factors ranging from age, gender, activity level, and more.
- Drink coffee: As if you needed another reason to indulge in a morning cup of joe, coffee (when sugar-free) offers antioxidants, which help protect the liver against damage, and helps with the liver’s process for burning fat for energy.
- Focus on whole foods that are minimally processed: “It’s not just about eating less—it’s about eating smarter,” says Dr. Purohit, “Reducing added sugars (especially from sugary drinks and processed foods), cutting back on refined carbs, and focusing on whole, unprocessed foods can make a big difference.”
- Practice time-restricted eating: Time-restricted eating (aka intermittent fasting) may also help protect liver function because it aids in weight management and enhances insulin sensitivity. However, this might not be the best strategy for everyone, including pregnant people and those with type 1 diabetes.
- Reduce fat and carbs: “Both low-carb and low-fat diets help reduce liver fat, with carb restriction—especially limiting free sugars—offering extra benefits,” explains Dr. Purohit. When possible, keep both carbs and fat healthy, such as opting for whole grains and legumes for carbs and avocados and nuts for fats.
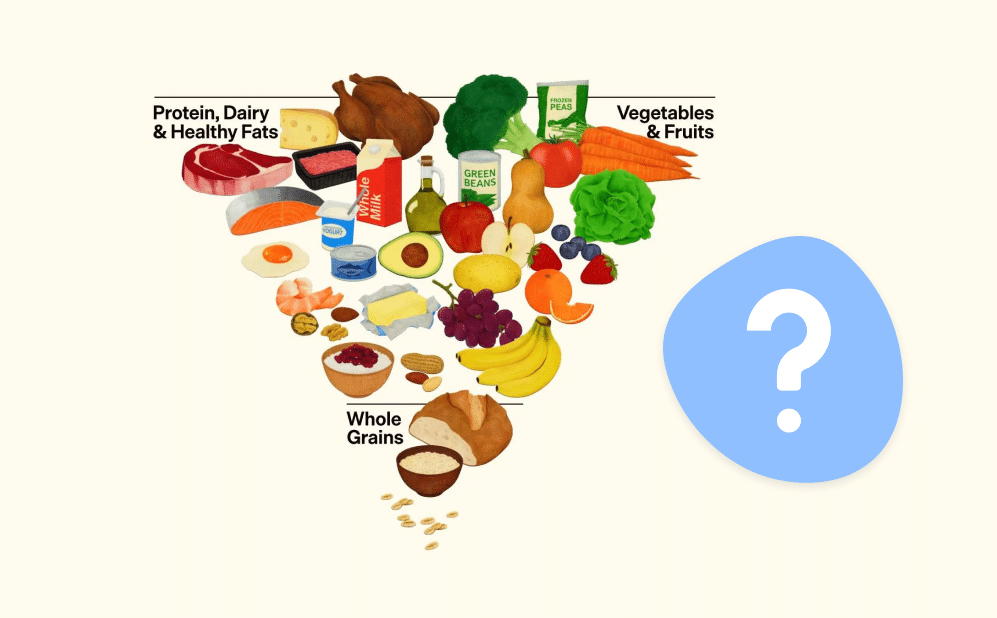
That said, sometimes it is easier to have a set diet to follow, especially if you’re busy. If that’s the case for you, a good fatty liver diet is one that’s delicious and includes a variety of nutritious foods that can reduce fat and help with insulin sensitivity. A great choice is the Mediterranean diet, which focuses on vegetables, fruits, whole grains, legumes, fish, nuts, and olive oil.
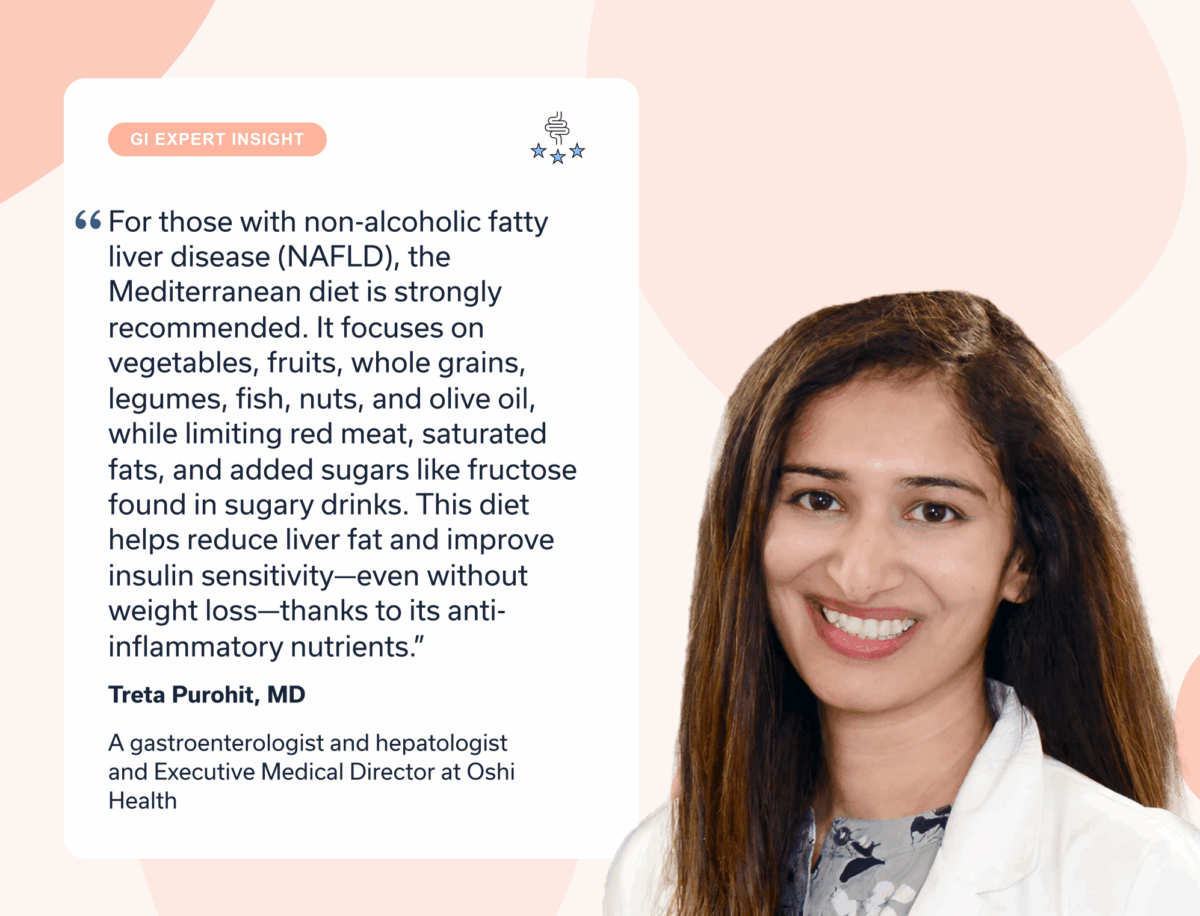
“For those with non-alcoholic fatty liver disease (NAFLD), the Mediterranean diet is strongly recommended,” says Dr. Purohit. In addition to the nutrient-dense foods included, this diet also advises “limiting red meat, saturated fats, and added sugars like fructose found in sugary drinks,” Dr. Purohit continues. “This diet helps reduce liver fat and improve insulin sensitivity—even without weight loss—thanks to its anti-inflammatory nutrients.”
What to eat and avoid on a fatty liver diet
So what exactly can you eat—and not eat—on a fatty liver diet? Here’s a list of foods to consider during your next grocery shop and ones to shy away from.
Foods good for liver health
- Coffee (without sugar)
- Cruciferous vegetables (broccoli, Brussels sprouts, cauliflower, etc.)
- Fatty fish (i.e. salmon, sardines, trout)
- Fruits (in moderation so as to avoid too much sugar)
- Leafy greens (i.e. spinach, kale, romaine lettuce)
- Lean animal protein such as grilled chicken or turkey
- Legumes (beans, chickpeas, lentils, etc.)
- Nuts (i.e. almonds, peanuts, cashews)
- Olive oil
- Seeds (i.e. sunflower seeds, pumpkin seeds, etc.)
- Whole grains like oats and brown rice

Foods to avoid with fatty liver
- Alcohol
- Fast food
- Fried foods
- High-fat dairy
- Processed meats
- Refined carbs (such as white bread, pastries, and chips)
- Red meat
- Sugary beverages and snacks (especially those with high-fructose corn syrup)
- Any other ultra-processed foods
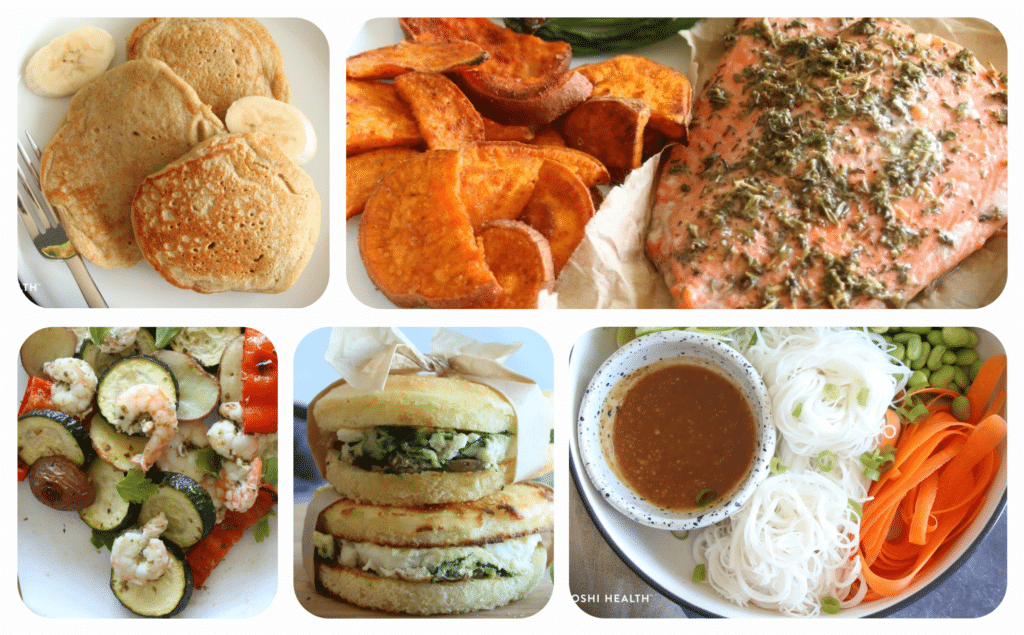
Sample fatty liver meal plan
Following a fatty liver diet is much easier when you have some go-to meals and snacks. To help, here’s a fatty liver diet menu with potential breakfasts, lunches, dinners, and snacks.
Breakfast options
- Egg white omelet with low-fat cheese and sauteed veggies
- Greek yogurt with minimally-processed cereal, chia seeds, and berries
- Low-fat cottage cheese with fruit and nuts or seeds
- Apple-cinnamon overnight oats
- Whole-grain toast with eggs
- Whole-grain bagel with hummus, tahini, or nut butter
- Zucchini bread pancakes
Lunch options
- Grilled chicken with whole-grain rice, roasted carrots, and cooked spinach
- Herbed salad with sweet potatoes and green beans
- Lentil soup (homemade or minimally-processed) with whole-grain crackers
- Tacos with tomatoes, beans, lettuce, guacamole or salsa, and a lean protein
- Tossed salad with chicken or chickpeas, assorted veggies, nuts or seeds, and a vinegar or vinaigrette dressing
- Chickpea chopped salad
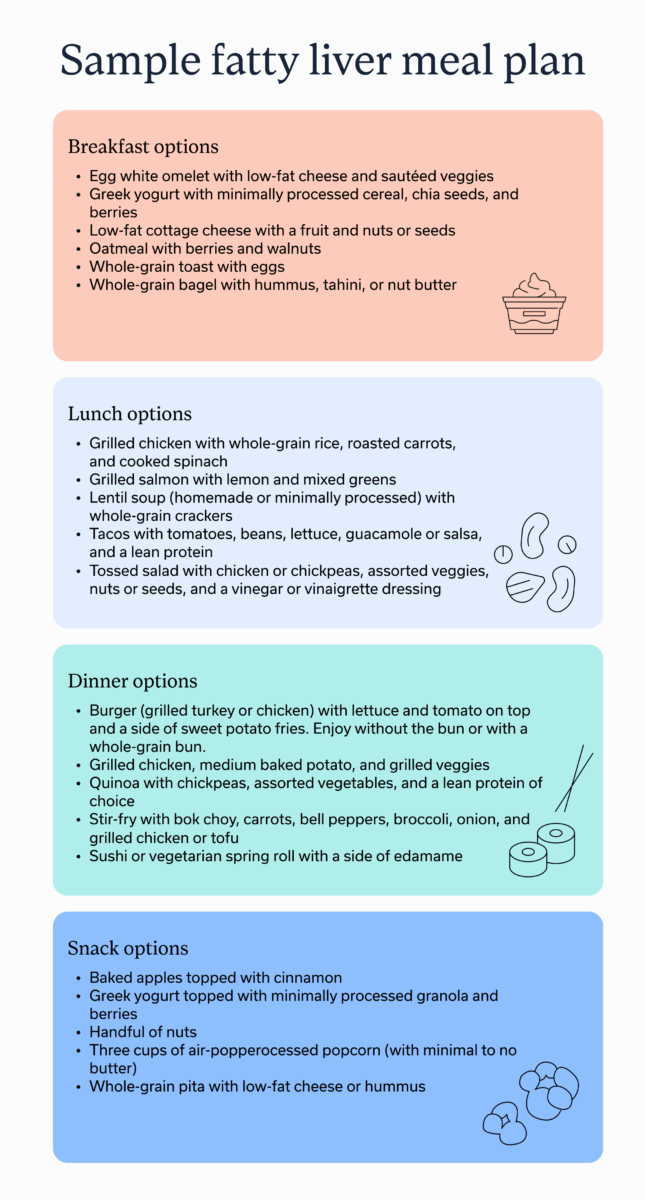
Dinner options
- Burger (grilled turkey or chicken) with lettuce and tomato on top and a side of sweet potato fries. Enjoy without the bun or with a whole-grain bun.
- Grilled chicken, medium baked potato, and grilled veggies
- Edamame noodle bowl
- Stir-fry with bok choy, carrots, bell peppers, broccoli, onion, and grilled chicken or tofu
- Sushi or vegetarian spring roll with a side of edamame
- Greek-inspired pan sheet shrimp and veggies
Snack options
- Baked apples topped with cinnamon
- Greek yogurt topped with minimally-processed granola and berries
- Crispy curried chickpeas
- Three cups of air-popped popcorn (with minimal to no butter)
- Whole-grain pita with low-fat cheese or hummus
- Seedy pizza crackers
Tips for long-term success on a fatty liver diet
Like any nutrition plan, a fatty liver diet is much easier to follow for a few days than month after month, even though it works better if incorporated for the long-haul. Fortunately, there are a few strategies to make a fatty liver diet a sustainable lifestyle change, rather than a temporary diet that stops as soon as life gets busy.
Focus on sustainability and gradual changes
We’ve probably all decided to go all-in on a restrictive diet at one point or another, only to fall off the bandwagon a few weeks (or days) later. That’s because grand, sweeping changes are harder to maintain than small, gradual ones—and this applies to a fatty liver diet too.
Slowly switching to this diet might mean adding in a few meals each week that follow the Mediterranean diet or cutting out one sugary snack at a time. “Even modest sugar reduction and time-restricted eating (like an 8–12 hour window) can help,” advises Dr. Purohit, “The key is finding what works for your lifestyle, and a nutritionist can help personalize it for lasting results.”
Batch-cook or meal prep to reduce barriers during the week
When life gets busy, healthy eating is the first thing to go in my household. To avoid this, my partner and I create a meal plan each Friday and batch-cook on Sundays, Tuesdays, and Thursdays, making extra of each meal so that other days, we can just zap healthy meals in the microwave.
I’m not saying you have to follow this exact process, though I can say that it works for us, but planning meals in advance and finding time to batch-cook makes it easier to eat healthy.
Track how different foods make you feel
When incorporating any change, reflection is part of the process. An easy way to reflect on nutritional changes is to keep a food log where you track what you eat, how you felt after (mentally and physically), and how much you enjoyed the meal. If there are certain meals you particularly enjoy, keep them in a virtual or physical recipe bank with the ingredients written out so they’re easy to return to.
Combine with physical activity
Regular physical activity is just as important as your nutrition, adds Dr. Purohit. That’s because “it helps burn visceral fat, improve insulin sensitivity, and supports overall metabolic health, even if weight loss is modest.”
This doesn’t mean you have to join an intense CrossFit class or register for a 100 mile cycling race. 150 minutes of moderate exercise a week, such as walking, yoga, or swimming, is the minimum recommended amount. That’s less than 30 minutes of exercise if you workout seven days a week, and exactly half an hour if you want to take two rest days.
Consider working with a registered dietitian or GI provider for support
While clinical research establishes that the above foods, meals, and strategies help with a NAFLD, that doesn’t necessarily mean they fit into everyone’s lifestyle and dietary preferences. For a more tailored approach, consider working with a GI registered dietitian or GI provider, such as the ones at Oshi Health.
“Regardless of body weight, all NAFLD patients should get guidance on diet, regular exercise, and avoiding alcohol,” says Dr. Purohit, “Working with a dietitian can help personalize these changes for better long-term success.”
Key takeaways
- What you eat and how much you eat both impact liver health. Research suggests those with NAFLD should follow a diet that prioritizes whole foods, fiber, and lean protein, such as the Mediterranean diet.
- Eating smaller portions, practicing intermittent fasting, and drinking coffee may also help with NAFLD.
- While standard dietary guidelines do exist for NAFLD, a fatty liver diet often works best when customized to your needs and taste. Oshi Health’s team of registered dietitians and gastrointestinal (GI) providers regularly help patients land on a tailored nutrition plan unique to them.
Frequently asked questions (FAQs)
-
A good menu for a fatty liver includes plenty of whole foods, lean protein, fiber, and minimal carbs and fats. When possible, opt for healthy carbs and fats.
-
Leafy greens, legumes, and lean protein are good foods for a fatty liver. If looking for a set diet to follow, the Mediterranean diet has the most evidence to suggest its benefits for treating a non-alcoholic fatty liver.
-
Drinks that are low in sugar and non-alcoholic are the best options for a fatty liver. Coffee in particular may help support liver health and water can help someone stay hydrated, which is beneficial for the digestive system overall.
-
In moderation, rice is a good addition to a fatty liver diet. When possible opt for a whole-grain option like brown rice instead of white rice, which is more processed. Quinoa and barley are two other substitutes for white rice.