While there isn’t a specific diet for ulcerative colitis (UC), there are general guidelines on what to eat (and avoid) during a flare and when UC is in remission. But those guidelines don’t typically come as full-fledged recipes. Luckily, we’re about to reveal a seven day meal plan for ulcerative colitis with easy-to-follow recipes and swaps for when symptoms are present.
Picture this: you get to the end of a busy workday, stomach grumbling and energy drained. You go to your fridge, praying to find something you can throw together for dinner. Yet your mind blanks on what to cook that’s delicious and won’t trigger an ulcerative colitis flare.
Not knowing what to eat is a pain for anyone, but it’s especially frustrating if you have a condition like ulcerative colitis where certain foods can trigger symptoms or may make a flare worse. While you can go to social media for recipe inspo, it’s hard to know if the top results are actually UC-friendly.
To help, we compiled a seven-day meal plan with recipes designed to make your taste buds and your digestive tract do a happy dance. Plus, we’ll detail what foods to avoid during ulcerative colitis flares.
UC nutrition basics: Foods to eat vs personal triggers
Managing a chronic condition like ulcerative colitis requires not one, but two gameplans. When UC is in remission, you can experiment with your ulcerative colitis diet and try out new recipes. During a flare, symptoms are in full-swing, and you need your tried-and-true recipes that won’t make symptoms worse or last longer.
When UC is in remission
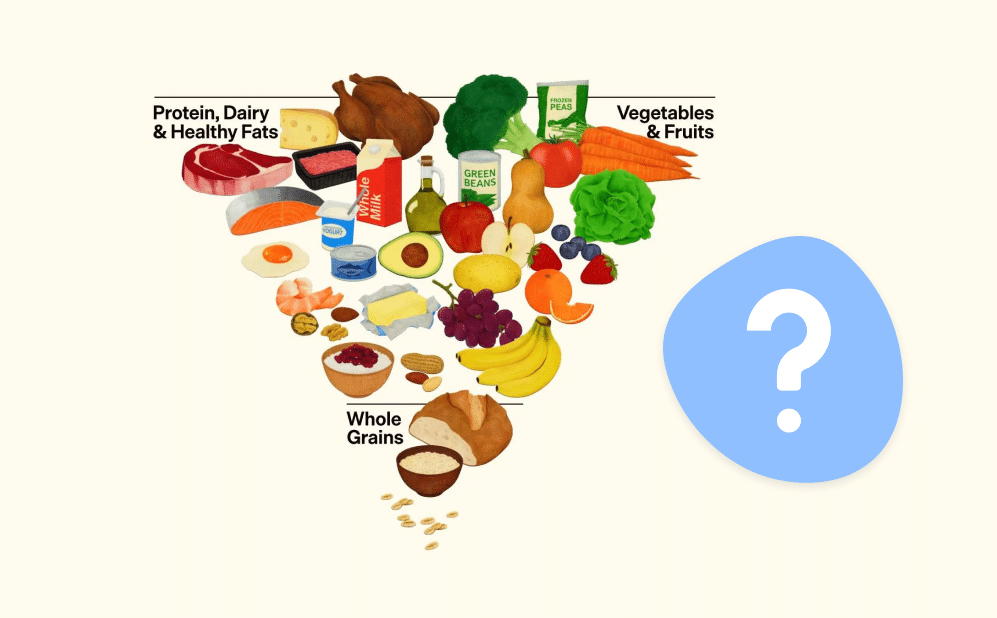
During periods of remission, pack your metaphorical bags and head to the Mediterranean. Unfortunately, the Mediterranean diet doesn’t come with a plane ticket to Italy and all you can eat pasta. That said, it is the one of the most evidence-backed diets for UC and includes many amazing recipes, including some mouth-watering pasta dishes.
The Mediterranean diet emphasizes foods with anti-inflammatory properties, such as:
- Plant-based foods, like fruits, legumes, and vegetables
- Lean protein and occasional red meat
- Healthy fat sources such as fish and olive oil
- Minimally-processed whole grains like quinoa and whole grain pasta
- Yogurts
- Cheese, in small amounts
- Limited alcohol
The beauty of this diet is that it’s much easier to follow than more restrictive diets (I’m looking at you, keto diet). It’s flexible, includes a lot of food groups, and has room for a few splurges, whether it’s a glass of wine paired with a cheese plate or a hearty steak on special occasions.
It’s also a fan-favorite with the gut microbiome, a collection of bacteria and other microbes in the intestines that affect digestion, the immune system, energy levels, mental health, and much more. Some research even suggests that the Mediterranean diet’s impact on the microbiome may lead to longer UC remission periods and less severe flares.
During a UC flare
When symptoms flare, turn to the GI gentle diet, which prioritizes soft-textured foods and moderate fiber intake. Its guidelines can help reduce symptoms like cramping, bloating, and abdominal pain:
- Add more liquid foods to your diet (think of a UC flare as soup season).
- A UC flare isn’t the time to splurge on steak. Instead, prioritize lean protein like grilled chicken, grilled turkey, or scrambled eggs.
- Avoid fruits or vegetables with skin, that are stringy, or contain seeds.
- Choose softer breads over ones that are crusty or have seeds.
- Opt for smaller, more frequent meals throughout the day.
- Prioritize cooked vegetables, skinless fruit, and whole grains as fiber sources.
- Reduce the amount of fiber in your diet to your personal tolerance level.
- Swap nuts out for softer sources (i.e. eat peanut butter instead of peanuts).
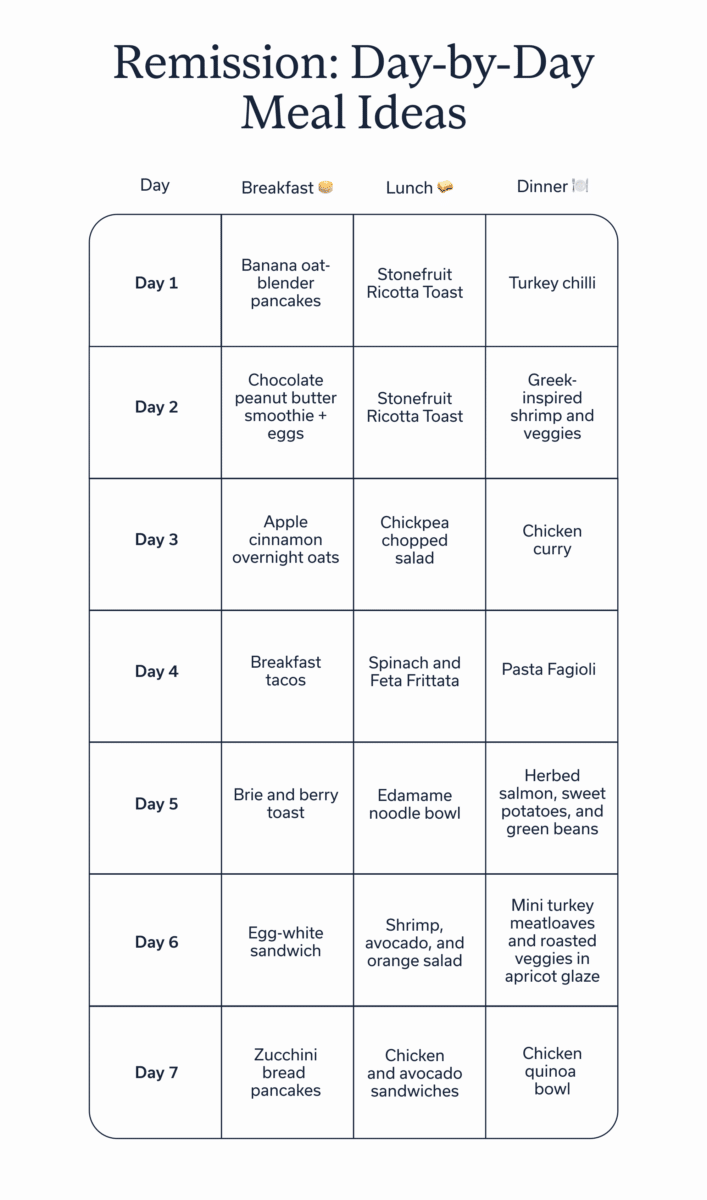
Remission: Day-by-Day Meal Ideas
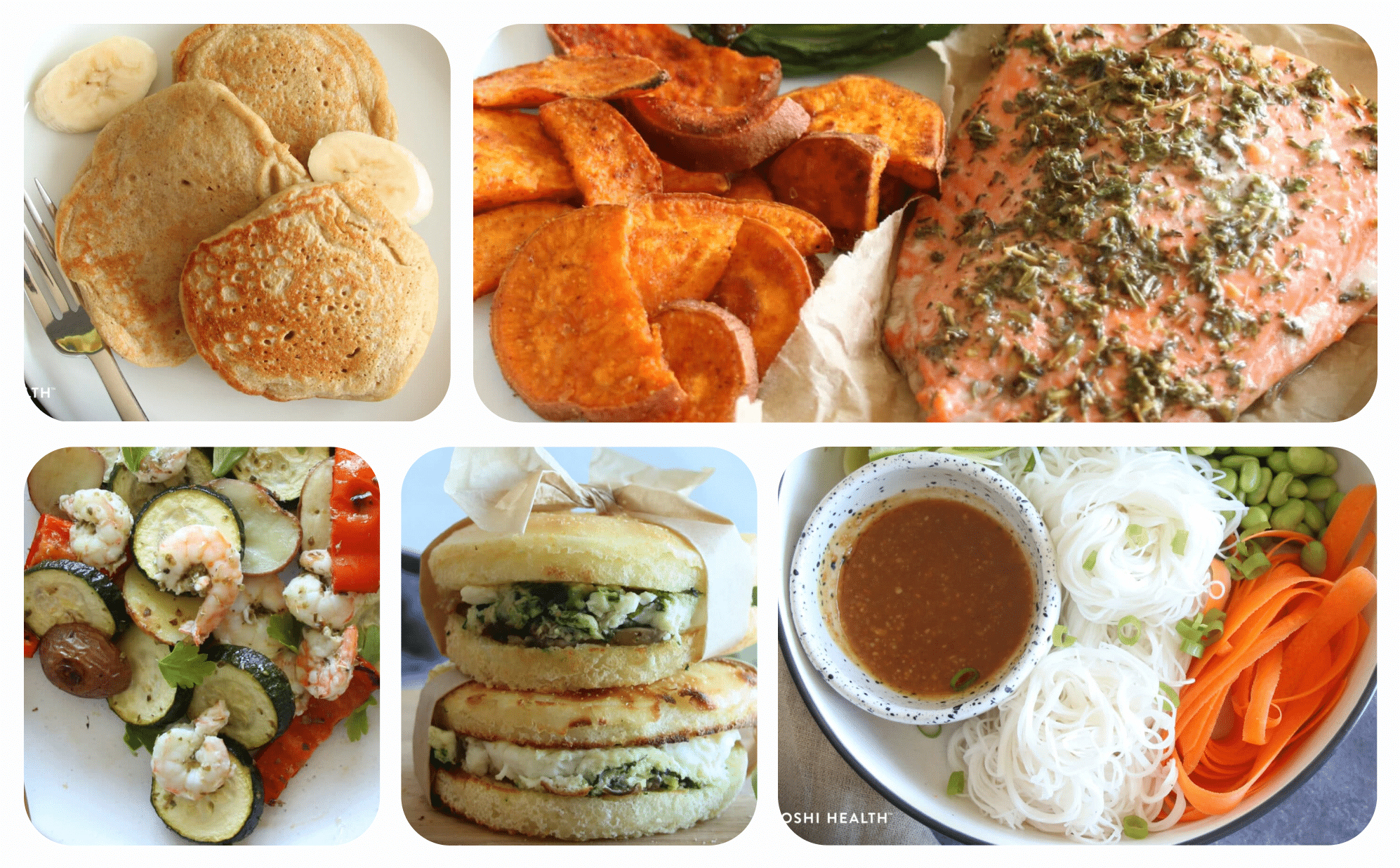
As promised, here are seven days of amazing recipes for when UC is in remission, all of which follow the Mediterranean diet.
And if you’re like me and love a good snack, here’s some recipes your gut and taste buds will love:
Flare-friendly modifications
Even though the recipes above are some of the best on the internet (not that we’re biased), some need to be modified during a colitis flare-up. For the brie and berry toast, for example, it may be best to swap the berries for a cooked berry compote and skip the brie during a flare.
More general modifications for UC flares include:
- Avoid raw produce
- Eat smaller, more frequent meals
- Eat less fat (even healthy fats, like avocado–though it still best to prioritize beneficial sources of fat when you do indulge)
- Swap out foods high in insoluble fiber, such as legumes, whole grains, nuts, and seeds
- For carbs, choose white rice, sourdough, and mashed potatoes over whole grains like brown rice or whole grain bread
- Swap some meals for smoothies, soups, or other liquid meals
- Temporary reduce lactose, such as yogurts or cheese
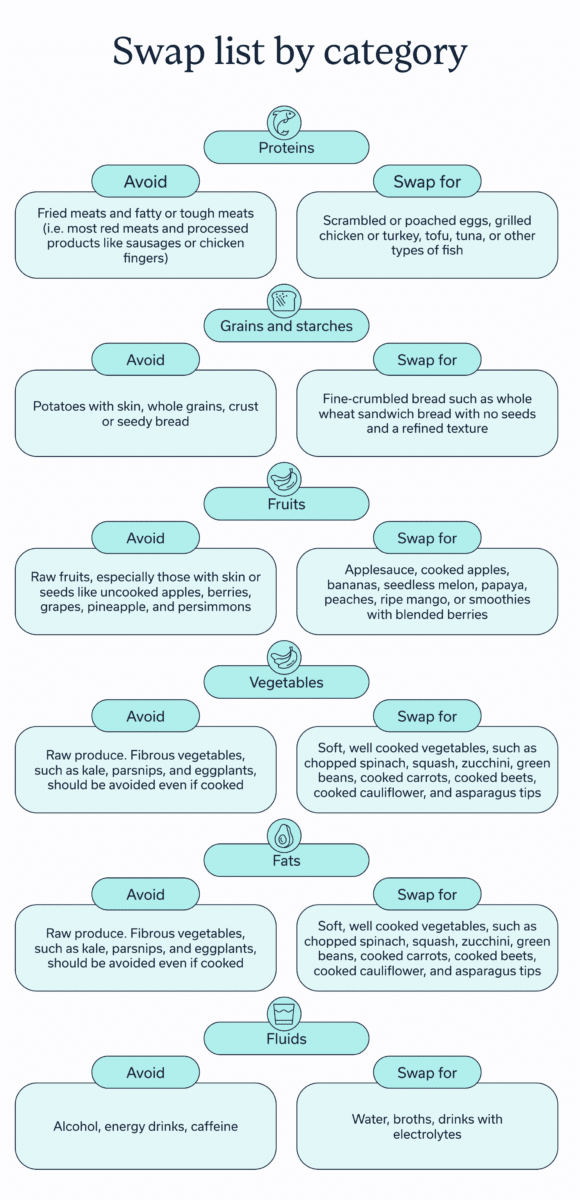
Swap list by category
| Category | Avoid | Swap for |
| Proteins | Fried meats and fatty or tough meats (i.e. most red meats and processed products like sausages or chicken fingers) | Scrambled or poached eggs, grilled chicken or turkey, tofu, tuna, or other types of fish |
| Grains and starches | Potatoes with skin, whole grains, crust or seedy bread | Fine-crumbled bread such as whole wheat sandwich bread with no seeds and a refined texture |
| Fruits | Raw fruits, especially those with skin or seeds like uncooked apples, berries, grapes, pineapple, and persimmons | Applesauce, cooked apples, bananas, seedless melon, papaya, peaches, ripe mango, or smoothies with blended berries |
| Vegetables | Raw produce. Fibrous vegetables, such as kale, parsnips, and eggplants, should be avoided even if cooked | Soft, well cooked vegetables, such as chopped spinach, squash, zucchini, green beans, cooked carrots, cooked beets, cooked cauliflower, and asparagus tips |
| Fats | Reduce fat consumption overall, especially from deep-fried foods | Healthy fats, like avocado and olive, in moderation |
| Fluids | Alcohol, energy drinks, caffeine | Water, broths, drinks with electrolytes |
Grocery & weekend prep
If you want to take your planning to the next level (and make your life 10x easier), consider ways you can prep your food over the weekend or on days of the week that are less busy. This might look like:
- Having set days when you shop for groceries so you have a stocked fridge more often than not
- Buying nonperishable staples in bulk, such as chickpeas and quinoa for remission periods or frozen bananas (for smoothies) and broth for UC flares
- Batch-cooking meals or parts of meals
It may also help to have a running grocery list on your phone. You can add staples when you run out of them and ingredients for new recipes. This way, you’ll avoid the frustration of walking into a grocery store and not knowing what you need and the internal groan of forgetting to pick up eggs.
Supplements & add-ons
The Mediterranean diet is hands-down the most effective way to get the nutrients our guts love. For those who struggle to follow this diet, supplements may help.
The best* supplements for UC are:
- Probiotics: A probiotic supplement contains bacteria strains that can strengthen the gut microbiome and may help improve the quality of life for individuals with UC. There is a specific probiotic supplement (VSL #3) that is backed by evidence in UC, but most probiotic supplements available on the market are not.
- Omega 3: An omega 3 supplement may offer similar gut health benefits as fish oil, though research is mixed on if it directly impacts UC.
- Vitamin D: This vitamin may help reduce inflammation related to UC, though most studies use animal test subjects, meaning the reported results may not be entirely applicable to us.
- Curcumin: In some studies, this spice helped reduce UC symptoms. It’s possible to use it as a spice when cooking, though some supplements also contain curcumin.
* Note: I use the word”best” hesitantly. The jury is still out on if supplements are beneficial for everyone with UC, meaning it’s best to discuss any of the above with a healthcare provider (ideally a GI specialist).
Other UC treatment options
Think about all the ways UC impacts your life or a loved one’s life. This chronic condition may cause unwanted GI symptoms, make meals less enjoyable, result in unease at work or in social situations, and so much more. The recipes above are a great tool, but managing irritable bowel syndrome (IBS) (or any condition that impacts all areas of your life) requires an entire toolkit.
Oshi’s Health treatment approach reflects that. Our team of GI specialists work together to make a diagnosis and create a comprehensive management plan. Alongside a UC diet, other treatment options include:
- Exercise: Moving your body may reduce UC inflammation, improve overall quality of life, and provide an energy boost for individuals with UC. Before you sign up for an extreme CrossFit class, rest assured that light to moderate exercise works too. In fact, during UC flares, it’s better to stay on the light side.
- Medications: UC medications relieve symptoms during a UC flare, prevent future flares, or help with both. A wide variety of UC medications, with different therapeutic targets, can be extremely effective in UC remission and preventing surgery or other complications.
- Stress management: Most of us have probably experienced knots in our stomach at one time or another. This sensation is a reminder of the gut-brain connection, which is why UC symptoms may be worse when you’re stressed or anxious. Two of the best stress management techniques for UC include meditation and breathwork. Bonus points if you work with a gut-brain specialist to customize either to gut health.
- Sleep: Getting seven to nine hours of quality sleep is always a good idea, and it even has UC-specific benefits. One study found poor sleep is associated with more UC flares while getting enough quality sleep (aka not tossing and turning all night) is correlated with fewer flares.
- Surgery: In severe cases, surgery may be required.
When to seek care
If experiencing any symptoms related to ulcerative colitis (i.e. diarrhea, blood in stool, abdominal pain, a constant need to poop, even when your bowels are empty), make an appointment with a GI provider who can assess symptoms and provide an accurate diagnosis.
Once diagnosed, you may want to work with a team of GI specialists (usually a GI provider, GI registered dietitian, and gut-brain specialist) so that treatment approaches your gut health from every angle.
Whether you have a UC diagnosis or not, seek immediate medical care if experiencing:
- A high fever
- Inability to keep fluids down
- Persistent vomiting
- Significant blood in stool
- Severe abdominal pain
- Unexplained rapid weight loss
Final thoughts
- Following a gut-healthy diet, like the Mediterranean diet, when UC is in remission and a GI-gentle diet when symptoms flare may help manage ulcerative colitis.
- This seven-day meal plan for ulcerative colitis is a flexible starting point that can be adjusted according to your preferences, symptoms, and personal UC triggers.
- These recipes and nutrition guidelines work best when incorporated into a larger treatment plan. Work with GI specialists, such as the team at Oshi Health, to create a tailored, comprehensive treatment approach.
Frequently asked questions (FAQs)
-
A good dinner for someone with ulcerative colitis is a meal that adheres to the Mediterranean diet, a popular nutritional plan that prioritizes anti-inflammatory foods. Salmon with roasted veggies, a chicken quinoa bowl, and a chickpea chopped salad all follow this diet.
-
Foods to avoid with ulcerative colitis, especially during flares, include high-fat foods, deep fried foods, and ultra-processed foods, such as potato chips or cake. During a flare, it’s also best to avoid raw produce, cooked or raw high-fiber veggies like kale or eggplant, and fruit or veggies with skin or lots of seeds.
-
Oatmeal is a great breakfast for someone with ulcerative colitis because it contains soluble fiber, which aids in digestion and supports a healthy gut microbiome. During a flare, be mindful of what you top oatmeal with, since ingredients like chia seeds, nuts, and uncooked fruit may make symptoms worse.
-
Many people with ulcerative colitis can eat pizza, so long as the toppings are also gut-friendly. If someone with UC is lactose-intolerant or gluten makes symptoms worse, consider lactose-free cheese or gluten-free dough.
-
Papaya is a low-fiber and easy-to-digest fruit. It’s especially beneficial during a flare, a time when it’s more difficult to eat other fruits, especially ones with a rough skin or many seeds.
-
There isn’t a cure for ulcerative colitis, meaning no one has ever recovered from it, but it is possible in most cases, with good clinical care to achieve disease control-remission. That said, many people develop successful treatment approaches that reduce the frequency and severity of UC flares. An effective UC management plan often includes medications, stress management techniques, dietary adjustments, exercise, medications, and a multidisciplinary approach.
Oshi is your partner in digestive health
Feel like your digestive concerns are running your life? You’re not alone—and we’re here to help you find lasting relief.
Oshi Health GI providers, gut-brain specialists, and registered dietitians work together to address your symptoms and find solutions that actually work for you.
Whether you’re dealing with chronic digestive issues or unpredictable symptom flare-ups, our GI specialists deliver:
✔ Personalized care plans tailored to your lifestyle
✔ Science-backed strategies to calm your gut
✔ Compassionate, whole-person care
✔ And so much more!
Ready to take control of your gut health?