Bloating (AKA abdominal distention) is a common inflammatory bowel disease (IBD) symptom. If you live with Crohn’s disease or colitis, that feeling of a tight, swollen belly can be uncomfortable, painful, and even disrupt daily activities.
Working with an integrated gastrointestinal (GI) care team can help find relief from bloating with solutions that fit your life. Oshi’s team-based care approach addresses medical, dietary, and gut-brain factors that affect your digestive health and can lead to bloating.
Let’s break down why bloating happens, how to prevent it, and when to talk to your GI provider.
Why does bloating happen?
Like other GI symptoms, bloating is your body’s way of telling you something is off in your digestive system. There are a few common reasons bloating shows up in people with IBD:
Changes in gut motility
Chronic inflammation from IBD can slow down digestion. When this ‘traffic jam’ happens, food and gas move more slowly, causing that full, stretched feeling.
In people with IBD, the small intestine can also struggle to absorb food. This lets more undigested food enter the colon, where more gas gets produced.
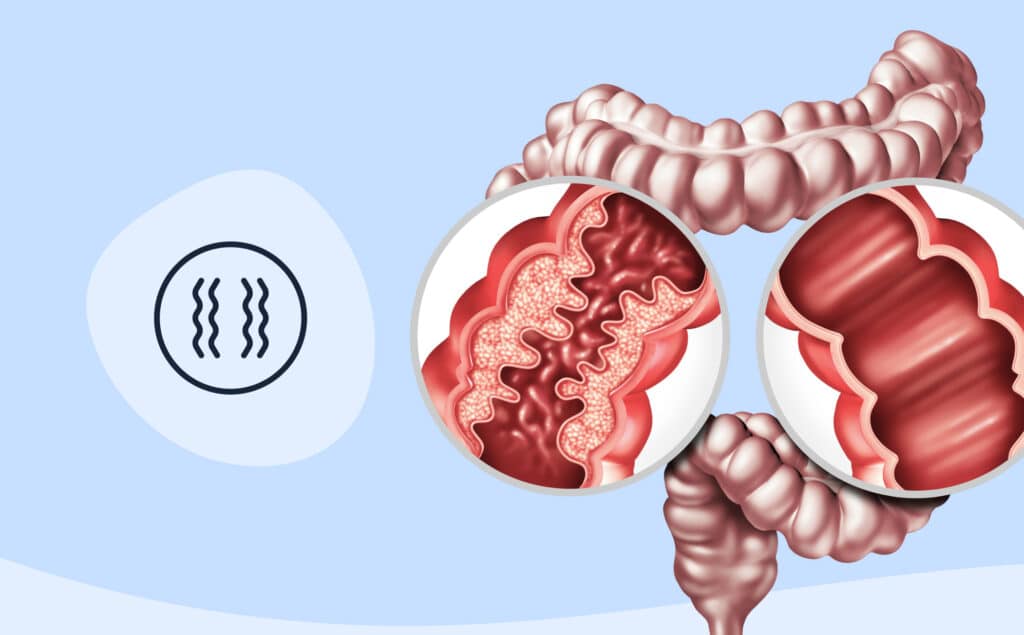
Scarring and narrowing (strictures)
If you have Crohn’s, inflammation can leave behind scar tissue that narrows your intestines. This can make it harder for food to pass through, leading to blockages or gut slowdowns—both of which can lead to bloat.
Scar tissue from past GI surgeries (colectomy or small-bowel resection) can also cause parts of your bowel to stick together (these are called adhesions). This can, in turn, trap gas.
Food intolerances
Living with IBD can make your gut extra sensitive to certain foods—especially those that are harder to digest or naturally create more gas, like dairy or beans.
Swallowing air
Everyday habits like chewing gum, sipping through a straw, or even eating too quickly can cause you to swallow more air, which ends up as extra gas and more bloating.
How to prevent and reduce IBD bloating
There are small, manageable steps you can take to help relieve IBD bloating.
Here are some common strategies:
Make some dietary adjustments
The following changes can help keep extra air and gas out of your system.
Lower your intake of bloat-causing foods, like:
- Legumes (lentils, chickpeas, and other beans)
- Whole grains and certain starches (corn, wheat bran)
- Dairy products with lactose (milk, cheese, ice cream)
- Certain fruits and veggies (apples, cabbage)
Personalized guidance from a GI registered dietitian
Everyone’s food triggers are unique. Your nutrition care plan should be, too.
Other tips to ease bloat:
- Eat smaller meals, and take the time to chew food thoroughly
- Cook food well to help break down fibers (and reduce gas production during digestion)
- Stay hydrated (this helps keep your gut moving)
- Sip drinks instead of gulping (and skip the straw when possible)
- Limit gum and fizzy drinks
Address the stress
It’s not just food that can cause digestive upset and bloating. Feeling overwhelmed and stressed can trigger IBD symptoms, too. Connecting with a gut-brain therapist can add another layer of support.
They can suggest practical tools for bloating relief like:
- Strategies to ease bloating discomfort in the moment, including:
- Belly breathing
- Mindfulness and relaxation techniques
- Stress management tools to prevent bloating in the first place
Let it out
You might feel embarassed about passing gas, but holding in *ahem* farts can trap gas inside your body and make bloating worse.
When to see a doctor about bloating
Bloating is common, but you shouldn’t ignore it—especially if it’s persistent or happens with other new symptoms. Here’s when it’s time to reach out to your GI care team:
- Your bloating lasts longer than 48 hours
- You have new or worsening symptoms with bloating, like vomiting or changes in bowel movements
- Your bloating is interfering with your ability to eat, sleep, or live your life
Your GI provider will work to treat the underlying cause of your bloating (e.g., Crohn’s or colitis). They might also recommend over-the-counter medications to temporarily help relieve bloating discomfort and pain like simethicone pills or peppermint capsules.
You know your body best, so if something feels off, trust your gut.
A high fever along with painful bloating could be a sign of a serious health emergency that requires immediate medical treatment.
Final word
Living with IBD means managing symptoms like bloating on the regular. In addition to the above strategies, compassionate, whole-person care can help you get control of your Crohn’s or colitis symptoms.
Oshi is your partner in IBD management
Feel like your IBD symptoms are running your life? You’re not alone—and we’re here to help you find long-term relief.
Oshi Health GI providers, gut-brain specialists, and registered dietitians work together to address your symptoms and find solutions that actually work for you.
Whether you’re looking to prevent your next flare or in the middle of one right now, your Oshi care team can offer:
✔ A personalized care plan tailored to your needs
✔ Referrals and support for in-person diagnostic testing and screenings
✔ Ongoing, compassionate care to help you achieve and stay in remission
✔ And so much more!
Ready to take get relief from IBD symptoms?