Some people may have a histamine intolerance that may contribute to GI or other symptoms. A histamine intolerance is not a food allergy. Instead, it means you may be deficient in an enzyme that’s required to break down the histamine content in foods, leading to an overload of histamine in the body that causes symptoms.
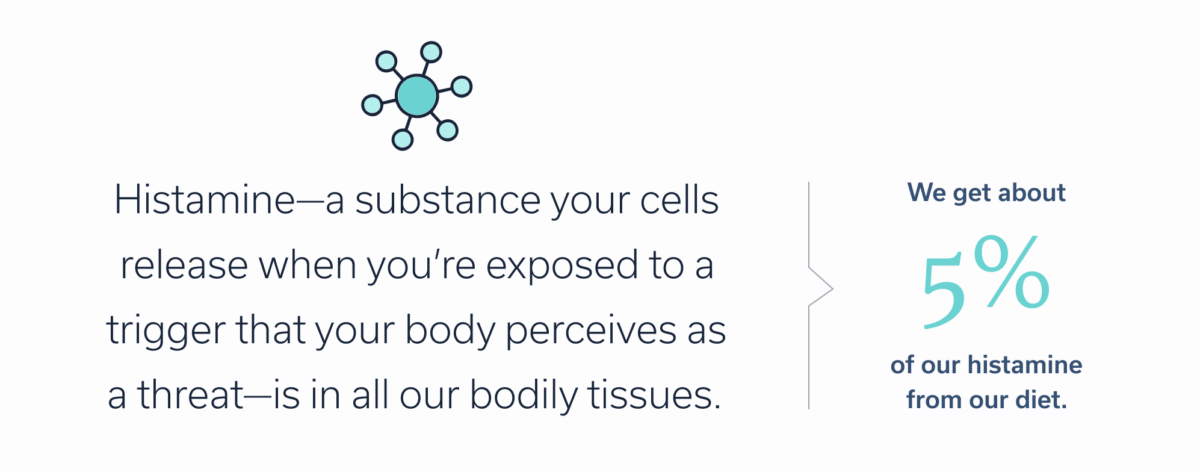
If you’ve ever had a sneezing fit on a fall day (*raises hand), you know all too well what histamine is. It’s a substance your cells release when you’re exposed to a trigger that your body perceives as a threat (Thanks a lot, ragweed!) Some foods that are higher in histamine can exacerbate certain gastrointestinal (GI) symptoms or conditions. If you have a suspected histamine intolerance, your clinician might suggest following a low histamine diet to investigate.
Our bodies produce histamine, but histamine is also in food. Our bodies can break down histamine, but some people have trouble with this, leading to a buildup of histamine. This excess histamine can trigger a host of unfun GI symptoms, including diarrhea, nausea, and more.
You may need to do an elimination diet to determine if histamine triggers your symptoms. However, a low histamine diet requires working with a medical professional, such as a GI registered dietitian, to ensure that you’re getting optimal nutrition despite eliminating certain foods.
Let’s explore what a histamine intolerance is, what a low histamine diet entails, and how to implement such a diet safely and effectively.
Understanding histamine intolerance
To understand what a histamine intolerance is, we first must unpack what histamine is. Histamine is a specialized neurotransmitter. It is in all our bodily tissues, but it’s highly concentrated in cells that are part of our immune system. If your immune system perceives a threat, such as that aforementioned ragweed (the bane of my existence), it mounts an inflammatory response to protect you. Histamine is what causes those classic allergy symptoms, such as sneezing, itching, watery eyes—you know, the ones that make you want to stay in bed and hide from the world.
Histamine is also present in most foods, with higher concentrations in some items, such as tomatoes, and lower in others, such as potatoes. We get about 5 percent of our histamine from diet. Our bodies break down histamine via diamine oxidase (DAO), an enzyme in the GI tract. But research suggests that some people are deficient in DAO.
A histamine intolerance shouldn’t be confused with a food allergy. Instead, think of it as a potential intolerance to certain foods. What’s the difference, you ask? We can compare histamine intolerance to lactose intolerance. People with lactose intolerance aren’t allergic to ice cream or milk. They just have trouble digesting lactose, the sugar found in dairy products. This is because they lack the lactase enzyme that hydrolyzes lactose into glucose.
Those with a histamine intolerance may lack the DAO enzyme that breaks down histamine. If this is you, your body may have trouble degrading or absorbing the histamine present in foods, such as the Gouda on your fancy mac and cheese. Histamine then builds up, leading to potential symptoms.
The symptoms can affect the integumentary (skin), cardiovascular, respiratory, nervous, and gastrointestinal systems. GI symptoms are particularly common in cases of histamine intolerance, with one study finding that bloating (oh yay) was present in 92 percent of 133 participants.
Symptoms of histamine intolerance
- Abdominal pain
- Acid reflux
- Bloating
- Brain fog
- Chest tightening/trouble breathing
- Constipation
- Diarrhea
- Dizziness
- Elevated heart rate
- Facial swelling
- Gas
- Headache
- Heart palpitations
- Hives/rash
- Menstrual cramps
- Migraine
- Nasal congestion
- Nausea
- Skin flushing
- Throat constricting
- Vomiting
Note: Some symptoms of histamine intolerance are severe and warrant seeking immediate medical attention. These include having trouble breathing, chest tightening, throat constricting, and more.
Many conditions can cause the above symptoms, so just because you have one or more of these symptoms does not mean you have a histamine intolerance. Additionally, sometimes histamine intolerance is associated with certain conditions, such as Crohn’s disease and ulcerative colitis, two types of inflammatory bowel disease (IBD). Celiac disease is also associated with histamine intolerance. A GI Registered Dietitian will look at the overall clinical picture, and might consider recommending a diet other than the low histamine diet to improve your GI symptoms.
Certain medications may also have a link with histamine intolerance, especially if they interfere with DAO activity. You should discuss this with your provider.
Working closely with a knowledgeable GI clinician can help you determine the root cause of your symptoms. Do not stop taking any medications without talking to your doctor.
What is a low histamine diet?
Clinicians do not have a tried-and-true way of diagnosing histamine intolerance, but a few methods can help determine whether the issue affects you. One is an elimination diet. The low histamine diet helps you eliminate high histamine foods to see if your symptoms resolve. Then you slowly reintroduce these foods, one at a time, to see if symptoms return after eating a specific food. If symptoms return, then you’ll know to avoid or reduce intake of that food in the future.
A low histamine diet is highly individual. The same foods that affect one person with a histamine intolerance may not affect the next person. A GI Registered Dietitian may even recommend a reduction in high histamine foods instead of a strict low histamine diet. Additionally, you may react differently to the same food at a different time, depending on various factors.
Our histamine levels rise at night and peak in the early morning, for example. This is because histamine likely plays a role in wakefulness, human and animal studies have shown. If you’ve ever had to take a first-generation antihistamine, such as diphenhydramine (often sold under the brand name Benadryl), which blocks histamine, you may have felt sleepy. So the time of day may play a role in whether you experience symptoms from a certain food.
People with suspected histamine intolerance should only undertake a low histamine diet with careful guidance from a medical professional. It’s also important to remember that elimination diets are not appropriate for everyone. The goal should be to ensure you can eat as wide a variety of foods as possible while keeping symptoms at bay.
Meet Oshi's GI registered dietitians
Find relief—and stay nourished
When you work with an Oshi GI registered dietitians (RD), you’ll get personalized nutrition guidance, including help with finding and avoiding potential food triggers, choosing gut-friendly supplements and recipes, and more.
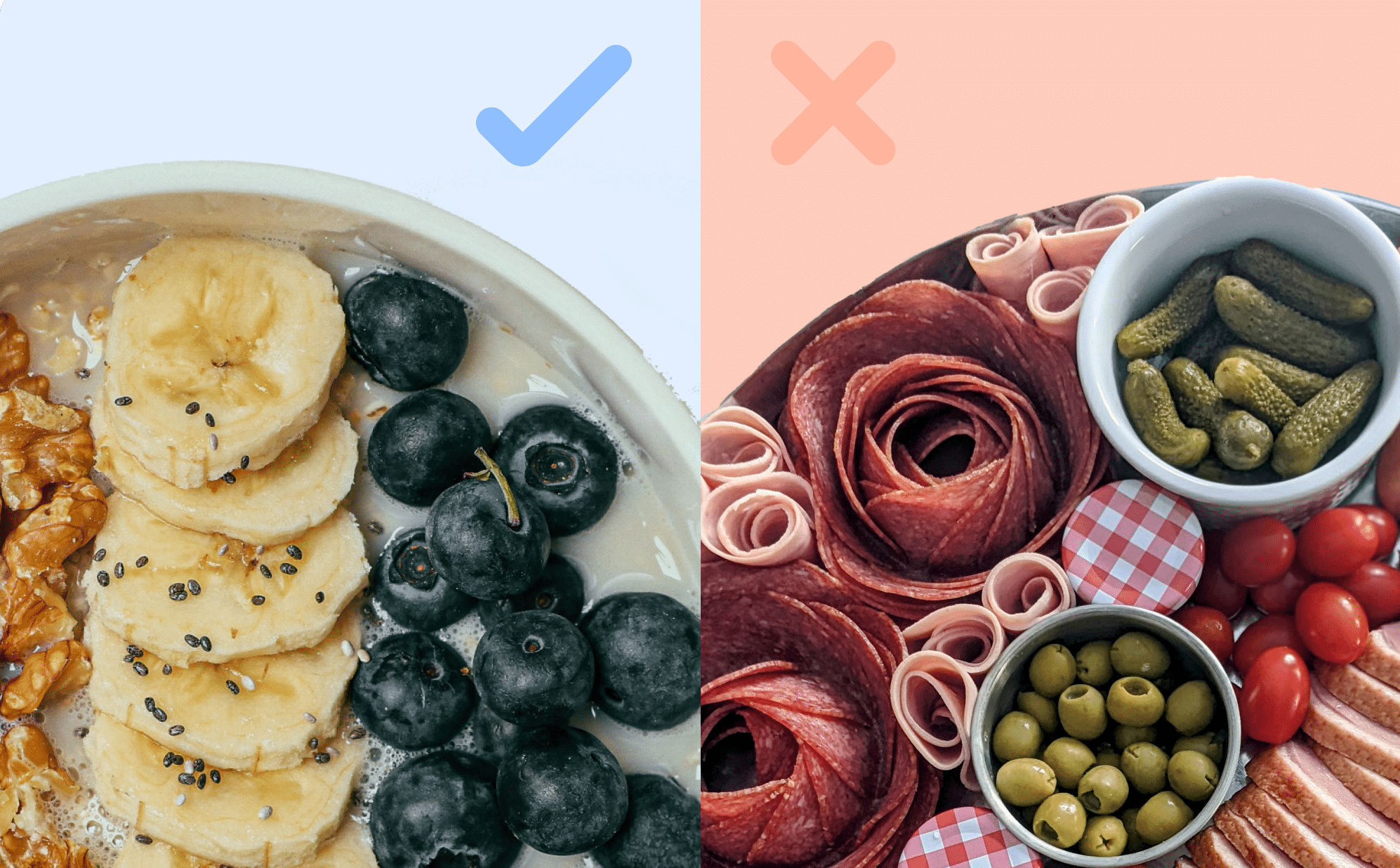
Foods to avoid on a low histamine diet
Researchers have yet to agree upon a unified low histamine diet. However, they seem to agree on a general list of foods to avoid when first beginning a low histamine diet. Oshi Health clinicians have developed a list of foods to steer clear of when first beginning a low histamine diet. But keep in mind that some of these may be added back in later, depending on your unique circumstances. Additionally, your dietitian may recommend a reduction of only a small group of the foods on this list, instead of a complete elimination diet, depending on your typical diet and symptoms.
Foods to avoid on a low histamine diet
Avoid foods naturally high in histamine
- Avocado
- Cherries
- Eggplant
- Spinach
- Soybeans and soy products
- Tomatoes that are red and ripe (green tomatoes are OK)
- Yeast extract (yeast itself as an ingredient is OK)
Avoid fermented and pickled foods, and foods that spoil quickly
- Aged cheeses (Gouda, cheddar, Camembert, Roquefort, bleu cheese, Emmentaler, Swiss, Parmesan)
- Canned, smoked, or salted fish (mackerel, herring, sardines, canned tuna, lox, smoked whitefish)
- Cold cuts, charcuterie and cured/processed meats (prosciutto, salami, nitrite-preserved bacon/ham/hot dogs, aged sausages)
- Cultured dairy foods (yogurt, kefir, buttermilk, cultured cottage cheese/cream cheeses)
- Dry aged meats/steaks
- Fermented condiments (soy sauce, teriyaki sauce, fish sauce, liquid aminos, coconut aminos, miso, black bean paste)
- “Fresh” (thawed) fish sold at a supermarket (individually quick-frozen filets are usually fine)
- Kombucha
- Leftover meats or spoiled foods
- Olives, sauerkraut, pickles, relish
- Shellfish (unless cooked from live)
- Vinegar-containing condiments: commercial salad dressings, ketchup, mustard, mayonnaise, hot sauce, barbecue sauce
Limit or avoid foods with histamine-releasing capabilities
- Baked goods that contain bleached flour (commercial breads and pastries)
- Berries (strawberries, raspberries, cranberries)
- Certain spices (cinnamon, cloves, anise, nutmeg, curry powder, chili powder)
- Citrus fruit (lemon, lime, orange, grapefruit)
- Cola
- Foods preserved with sulfites (dried fruit, frozen potatoes, red wine)
- Foods preserved with BHA or BHT (some breakfast cereals)
- Foods that contain artificial food coloring, especially tartrazine (FD&C Yellow #5)
- Grapes
- Licorice
- Papaya
- Pineapple
- Pumpkin seeds
- Stone fruits (apricots, plums, nectarines)
- Tea
Limit or avoid alcohol (which blocks DAO)
- Beer
- Red wine
- White wine
Implementing a low histamine diet
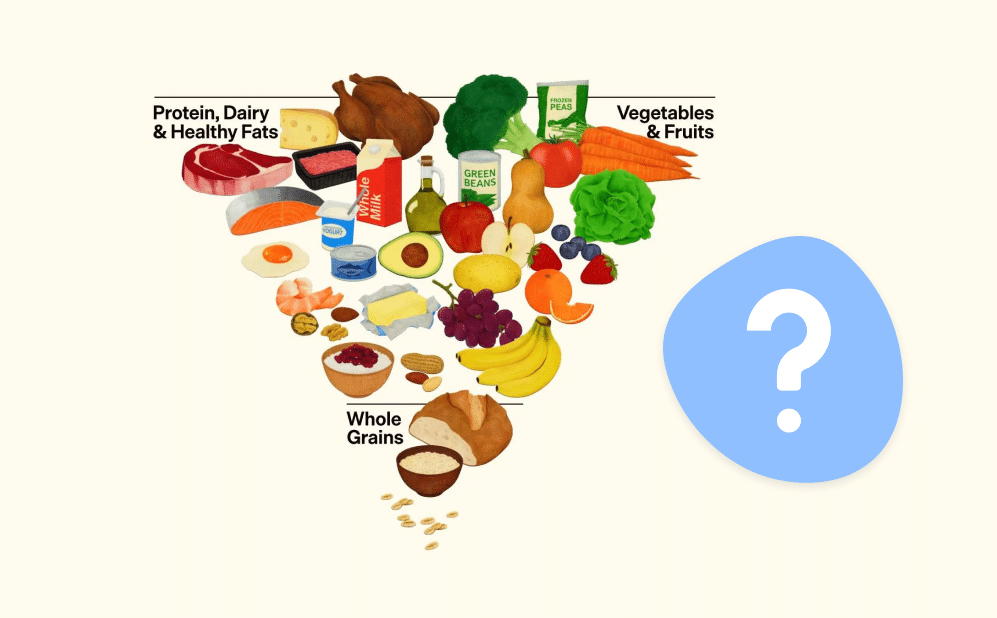
Elimination diets tend to focus on what to avoid, but when embarking on a low histamine diet, knowing what you can eat is also helpful. There are certain foods that are generally considered to be low in histamine, but again, any diet is highly individual. The following are Oshi Health-recommended foods for people on low histamine diets.
Foods that are low histamine
Low histamine fruits
- Apple
- Banana
- Blueberries
- Coconut
- Dragon fruit
- Figs
- Guava
- Jams (made from fruits on this list that don’t contain sulfites)
- Kiwi
- Lychees
- Mango
- Melons
- Pear
- Peaches
- Rhubarb
- Starfruit
Low histamine vegetables
- Asparagus
- Beets
- Broccoli
- Brussels sprouts
- Cabbage
- Carrots
- Cauliflower
- Cucumber
- Corn
- Garlic
- Green beans
- Kale
- Lettuce
- Onion
- Peppers
- Zucchini
Low histamine proteins
- Eggs, fully cooked (especially yolks)
- Fresh meat, chicken, turkey (avoid leftovers)
- Individually quick-frozen fish filets
- Legumes (except chickpeas, lentils, red beans and soybeans/tofu)
- Milk and fresh cream (plain)
- Nuts and seeds (except pumpkin seeds)
- Nut butters (natural, no preservatives)
- Protein powders, plain or vanilla (with no added colors, sweeteners, or preservatives)
- Sunbutter
- Uncultured cheeses (cottage cheese, cream cheese, ricotta, mascarpone, paneer, fresh mozzarella)
Low histamine grains and starches
- Biscuits or scones that use baking soda/powder and unbleached flour
- Breads, crackers, and baked goods made with unbleached white flour or whole wheat flour
- Buckwheat
- Cereals that are plain (corn flakes, shredded wheat, rice cereal, oats/oatmeal, cream of wheat and cream of rice)
- Corn
- Couscous
- Millet
- Pasta (plain)
- Popcorn
- Potato and sweet potato (not frozen potato products)
- Quinoa
- Rice (all varieties), rice cakes, rice crackers
Low histamine seasonings
- Butter
- Garlic
- Herbs and spices (except those listed in the foods to avoid)
- Honey
- Maple syrup
- Oil
- Pepper
- Salt
- Sugar
Low histamine beverages
- Coffee
- Juices (made from the low histamine fruits list)
- Milk
- Tea (herbal, but no zingers or zests)
- Sparkling water (unflavored)
Low histamine desserts
- Ice creams (vanilla) with short ingredient lists
- Cookies and cakes made with unbleached flour, real butter, sugar, eggs etc.
Tips for success on a low histamine diet
After a period of avoiding certain foods on a low histamine diet, you’ll carefully add foods in, one at a time, with the guidance of your clinician. A few tips can help.
Keep a food and symptom diary
Start keeping a food and symptom diary when you start your low histamine diet and as you slowly add foods back in. Write down the date, time, and contents of each meal, snack, and beverage (aside from water) and note if the meal produces any symptoms. Include the type of symptom, its severity, and the time. The information you include in your food diary can help your clinician further tailor a diet that’s right for you.
Avoid frying or grilling
Some cooking methods may increase the histamine content of foods, while others might reduce it. One study investigated the changes in histamine levels of foods based on different cooking methods: frying, grilling, boiling, or fermenting. The researchers found that frying and grilling tended to increase histamine content, whereas boiling either didn’t change histamine content or reduced it.
Takeaway
- Some people may have a histamine intolerance that may contribute to GI or other symptoms.
- If your clinician suspects you have a histamine intolerance, they may recommend a low or reduced histamine diet.
- A low histamine diet is an elimination diet that temporarily eliminates foods that are high in histamine before reintroducing them, one by one, to see if they contribute to symptoms.
- You should only undertake a low histamine diet under the guidance of a clinician.
- Oshi Health has GI registered dietitians with extensive knowledge about low histamine diet protocols. Schedule your first appointment to address your digestive health concerns.
FAQ
-
If you suspect you have high histamine levels and a histamine intolerance, be sure to consult a knowledgeable clinician, such as the GI experts at Oshi Health. They can determine if a low histamine diet is right for you, and if so, tailor it to your unique needs, ensure you’re getting adequate nutrition, and help you carefully reintroduce foods after a period of elimination.
-
You cannot flush histamine out of your body, because it is a chemical present all over in specialized cells. If you need to reduce histamine levels because of a condition or histamine intolerance, work with a knowledgeable clinician who can help you lessen consumption of foods that affect histamine levels.
-
A low histamine diet is an elimination diet to help you determine if any foods are the culprit of your symptoms. You should only undertake a low histamine diet under the guidance of a knowledgeable clinician. They can help you eliminate suspected foods and then carefully reintroduce them, as appropriate, while monitoring for symptoms.
-
A low or reduced histamine diet may be appropriate for certain individuals who are suspected of having histamine intolerance, are on certain medications that disrupt histamine breakdown, or who have certain conditions. You should only follow a low histamine diet under the guidance of a clinician, such as a registered GI dietitian.