“Leaky gut” has become a bit of a buzz-phrase, but it is not a medically diagnosable condition. However, some people do have increased intestinal permeability that may lead to gastrointestinal (GI) issues or other health concerns. Increased intestinal permeability occurs when your gut barrier has become dysfunctional or damaged. Your gut barrier operates like a security feature, letting nutrients and water into the rest of your body and toxins and pathogens out; when damage occurs, this “security guard” doesn’t function as well as it should.
The phrase “leaky gut syndrome” is interesting, since it’s not a true medical term, yet the social media hive mind seems to constantly mention it, creating some confusion. So let’s unpack where the term comes from, why it’s such a buzzy topic, and the truth about leaky gut.
Some people do experience what’s called intestinal barrier impairment, where the crucial lining of the intestines has incurred some damage. This damage can then allow substances into the rest of the body that should be kept out. When they enter, they can cause trouble.
But our intestines aren’t meant to be like a brand-new garden hose, shuttling substances through until they’re, ahem, eliminated at the other end. We need some permeability. That’s why the use of the term “leaky” isn’t technically an accurate one. But it does help describe the idea of problematic substances getting through the barrier.
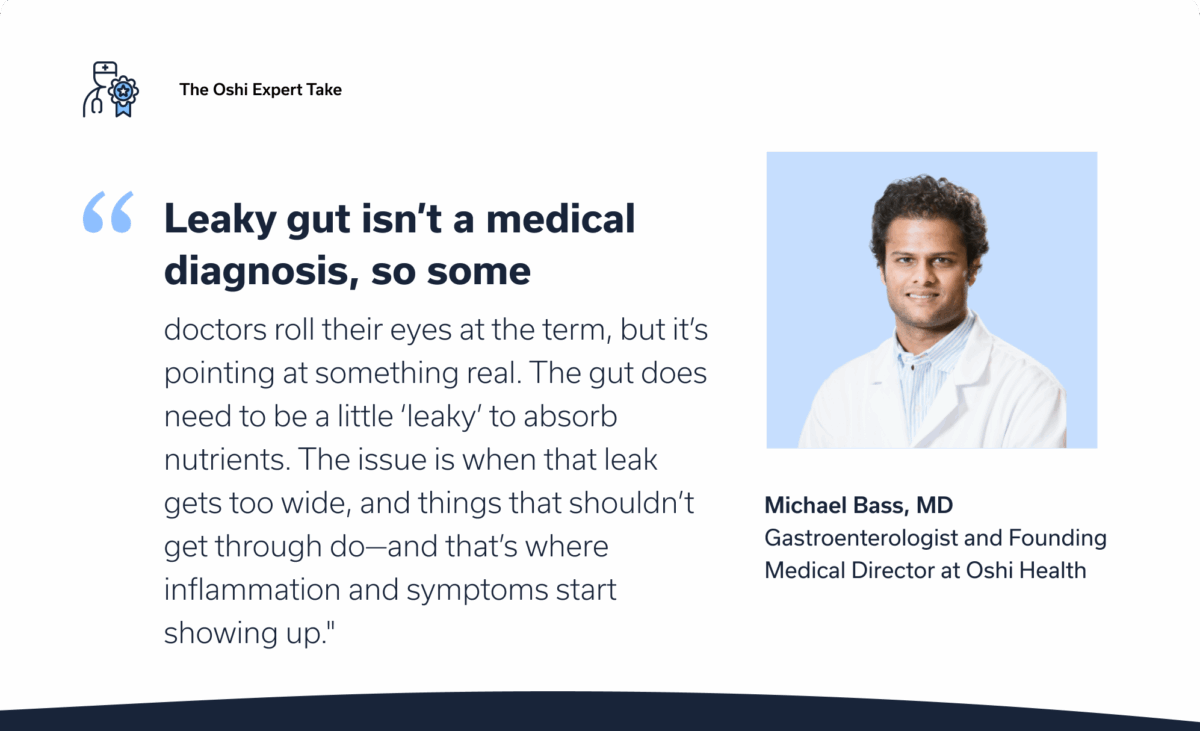
“Leaky gut isn’t a medical diagnosis, so some doctors roll their eyes at the term,” says Michael Bass, MD, medical director at Oshi Health. “But it’s pointing at something real. The gut does need to be a little ‘leaky’ to absorb nutrients. The issue is when that leak gets too wide and things that shouldn’t get through do—and that’s where inflammation and symptoms start showing up.”
The point here is that your GI symptoms are very real, and they may be a result of intestinal barrier (aka “gut lining”) damage or dysfunction.
If this all a little confusing, gaining an understanding of the intestinal barrier and what it’s supposed to do—and how it can go haywire—can help. So let’s get into it.
Understanding the intestinal barrier
Your body needs nutrients and water to survive. Your GI tract absorbs those things from the food and drinks you consume, and then eliminates what you don’t need. “Think of your gut lining like a security gate,” Dr. Bass says. “It lets the good things in (nutrients and water) and keeps the troublemakers out (toxins and bad bacteria). When that gate breaks down, your whole body can feel it.”
The troublemakers, as Dr. Bass notes, are toxins and bad bacteria or other microbes. They may cause further GI tract inflammation and problems in other parts of the body as well. Why is the security system malfunctioning and letting the bad fellas in?
“We see this in Crohn’s, celiac, irritable bowel syndrome (IBS), even in autoimmune diseases—a stressed-out gut barrier that’s letting in things that trigger the immune system,” Dr. Bass says. “It’s not always the root cause, but it’s often part of the puzzle.”
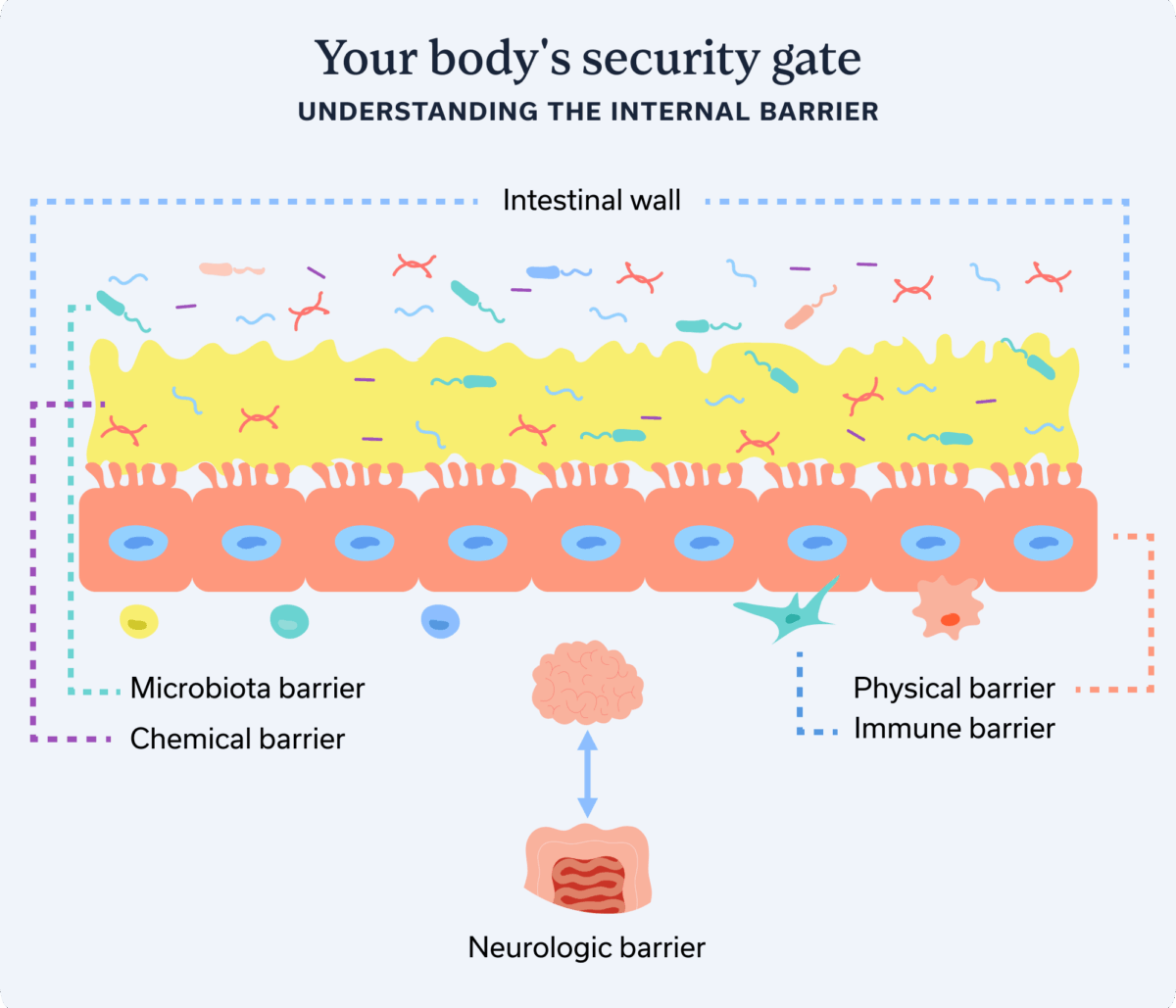
Your intestinal barrier is complex and is made up of several elements, not just one barrier meant to keep the baddies out. Different barrier elements perform different functions, but they all work together as a security system.
Microbiota barrier
Think of this layer as the first security checkpoint in your GI tract. Your intestinal microbiota is a community of microorganisms that live in your gut. This community helps produce protective mucus and immune cells. But it also produces antimicrobial substances to defend against harmful bacteria. And the good bacteria that make up the microbiota use some of the nutrients you eat to produce helpful substances that support the rest of your gut barrier.
The chemical barrier
This barrier is a layer of antimicrobial substances, specifically mucins and peptides, that protect the intestinal lining from troublemaker substances. Mucins form a gel-like structure, while peptides help regulate the gut microbiota, acting like built-in antibiotics to prevent bacterial overgrowth.
Physical barrier
Epithelial cells make up much of this barrier and are connected via specialized junctions. For example, tight junctions “stitch” cells together, creating a strong physical barrier involved in protection, secretion, and absorption. Think of the microbiota and chemical barriers (mentioned above) as if they are a salve protecting this physical barrier, which is meant to prevent troublemakers from going any farther.
Immune barrier
The immune barrier is part of the lamina propria, a thin layer of connective tissue under the physical barrier (epithelium). It’s called the immune barrier because it includes immune cells that help recognize and defend against harmful substances that may have slipped past the physical barrier.
Neurologic barrier
The neurological barrier is part of the whole caboodle. Your enteric nervous system lines your GI tract from your esophagus to your rectum. It facilitates communication along your gut-brain axis, the information superhighway between your GI tract and your brain. It helps control the movement of food and waste through the digestive tract, but it also plays roles in gut-barrier function. It detects bacteria and can even elicit vomiting if something serious has gotten through the security gate.
What causes a “leaky gut” and increases intestinal permeability?
As you can see, your GI tract has several built-in defenses running your personal homeland security. But when a breach in defense occurs with any of these barriers, GI and other symptoms can ensue. A breach increases intestinal permeability, meaning the gut is leakier than it should be. But what causes a breach in the first place? Several factors can play a role.
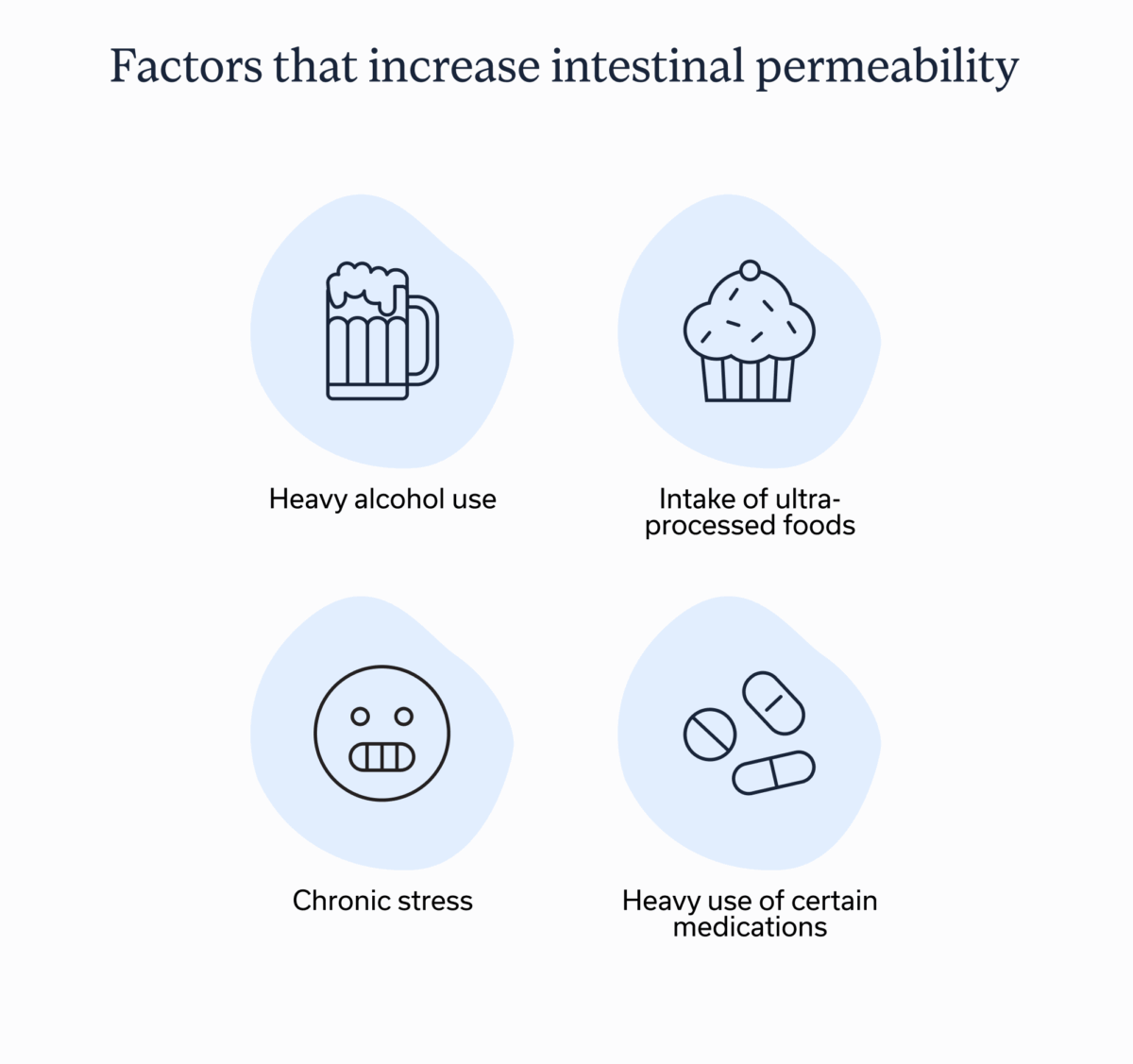
Heavy alcohol use
The occasional drink likely won’t increase your intestinal permeability in the long run, at least not in healthy people. However, regular drinking, especially heavy consumption, poses a threat to GI health and barrier function.
“Alcohol has been directly linked to apoptosis (cell death) of epithelial cells throughout the gastrointestinal tract,” says Brianna Olivieri, MS, RD, a registered dietitian with Oshi Health. “Furthermore, consumption of alcohol can cause damage to certain proteins that normally help to seal the spaces between cells in the gut lining.”
Intake of ultra-processed foods
“Ultra-processed foods (UPFs) are defined as foods with high energy density, low nutritional quality, and the presence of additives that make them more palatable,” Olivieri says. “This may include commercially available sweets, baked goods, and microwave-ready frozen meals.”
The scientific community is still learning about the effects of UPFs, but some preliminary research specific to gut-barrier function revealed that emulsifiers, commonly added to these foods, increased intestinal permeability and inflammation in mice. And laboratory studies on human epithelial cells revealed that emulsifiers may contribute to increased intestinal permeability. However, direct human studies have been inconclusive.
“That said, it’s important to point out that processed foods can be part of a well-balanced diet, and not all processed foods are harmful,” Olivieri continues. “For example, processed foods such as canned beans, pasta sauces, whole-grain bread, and frozen vegetables can be convenient ways to add fiber, variety, and flavor to a well-balanced diet.”
Chronic stress
Your gut and brain communicate with each other via the gut-brain axis. And your enteric nervous system is part of your gut barrier. Chronic stress may therefore disrupt your gut barrier, with microbiota disruption likely playing a partial role.
Heavy use of certain medications
Sometimes we have to take medications to find relief from ailments or to protect our health. For example, most of us have reached for over-the-counter non-steroidal anti-inflammatory drugs (NSAIDs) like aspirin or ibuprofen when we’ve had a headache or backache. However, NSAIDs appear to induce intestinal permeability by harming the gut’s physical barrier.
Most of us have also required the occasional course of antibiotics to fight a bacterial infection. By their nature, antibiotics battle bad bacteria, but they can also harm the good bacteria present in your gut microbiota. They also damage the tight junctions in your gut’s physical barrier.
Autoimmune disorders
Some autoimmune disorders and leaky gut share connections. Having an autoimmune disorder means your immune system mistakenly attacks your healthy cells and tissues, causing damage.
Conditions (autoimmune and otherwise) associated with altered intestinal permeability
- Celiac disease
- Inflammatory bowel disease (IBD), including Crohn’s disease and ulcerative colitis
- Multiple sclerosis (MS)
- System lupus erythematosus (SLE)
- Type 1 diabetes
- Irritable bowel syndrome (IBS)
- And more
Should you test for leaky gut?
Oshi Health does not recommend testing for intestinal permeability for several reasons. Some studies have explored tests, but they aren’t well validated yet and have different metrics. For example, some measure excretions in urine, while others test stool. Plus, these tests aren’t widely available. “There’s no gold-standard test right now,” Dr. Bass says.
Your provider might request baseline testing for other factors that may be causing your GI symptoms. For example, do you have a structural issue? They may test you for GI inflammation or bleeding, bacterial infection, and/or whether you have nutrient absorption issues. These tests may help inform your provider whether you’re potentially experiencing a compromised gut barrier and why.
With or without testing, the best bet is to emphasize symptom resolution. “I focus on the person,” Dr. Bass says. “What are your symptoms telling us? I always go to first principles and evaluate stress, sleep, diet, and exercise.” These tactics help reduce the need for unnecessary invasive tests and take the process one step at a time to help you find relief.
Treating altered intestinal permeability involves treating the root cause
If your care team suspects that you’re experiencing intestinal barrier dysfunction, they will work with you to determine why and then treat the root cause. Treatment should take a multidisciplinary approach to address various factors related to your unique situation. Here are a few examples.
Manage underlying conditions
Appropriately managing any underlying conditions can help. For example, if you have IBD or another autoimmune disorder, you may need an enhanced treatment protocol to improve your condition management, especially if you’re experiencing a flare.
Improve the gut-brain connection
Remember: Your gut and brain talk to each other. So when one isn’t doing well, it affects the other. Managing stress, anxiety, depression, and other mental health concerns may help improve your GI barrier health. Working with a GI psychologist can help you create strategies that bolster your gut-brain communication.
Support your gut barrier with nutrition and sometimes supplements
A GI registered dietitian can be key in helping you address which foods and supplements will help enhance your gut microbiota and overall barrier health. Here are a few considerations.
Eat a mostly whole-food diet
“When your diet consists of a wide variety of fruits, veggies, grains, healthy fats, and lean protein sources, there will be less ‘gaps’ to fill with UPFs,” Olivieri says. Many plant-based whole foods are also packed with fiber and polyphenols that help support gut barrier function. See more on each below.
Consume more fiber
Fiber helps feed the good bacteria in your gut, which can strengthen your gut barrier. When the bacteria in your gut ferment fiber, they produce short-chain fatty acids (SCFAs). “SCFAs serve as an energy source for epithelial cells, promoting mucus production and secretion,” Olivieri says. “A healthy mucus layer can act as a protective barrier within the GI tract.”
Amp up your polyphenol intake
Polyphenols are beneficial plant-based compounds with anti-inflammatory effects. You can get them from fruits, veggies, nuts, seeds, legumes, whole grains, some spices, dark chocolate, and coffee and certain teas, specifically black, green, and white.
“Polyphenols can help to keep the gut lining healthy and functioning properly in several ways,” Olivieri says. “They can help to strengthen the connections between cells, promote beneficial bacteria in the gut, and lower inflammation by reducing harmful molecules.”
Eat a variety of protein sources
Glutamine is a nonessential amino acid, meaning your body produces it by breaking down protein. Eating a balanced diet of protein sources can enhance glutamine production, which may be beneficial for reducing inflammation and strengthening tight junctions in your gut’s physical barrier.
Consider supplements when deficient
If you are deficient in beneficial gut bacteria or certain nutrients, your care team may recommend probiotics or other supplements to help populate the gut. Again, a GI registered dietitian can be super helpful here, so that you aren’t spending your hard-earned money on too many supplements, some of which may not work or may not be necessary. Plus, over-supplementation is a thing—and it can lead to toxic levels of some vitamins and nutrients.
Two supplements may be particularly helpful for strengthening your gut barrier, if you’re deficient in them:
- Vitamin D. This vitamin appears to help strengthen the physical barrier by enhancing tight-junction proteins. It may also help upregulate antimicrobial peptides to prevent harmful bacteria from taking over.
- Zinc. If you’re deficient in zinc, you may have a less diverse community of bacteria in your gut, which could contribute to increased permeability. However, the right dosage is crucial, since overconsumption of zinc may also lead to issues with your microbiome.
Key takeaways
- “Leaky gut ” is not a medically diagnosable condition; however, some people have increased intestinal permeability that may allow harmful substances to pass through to the rest of the body, causing uncomfortable GI symptoms.
- Increased intestinal permeability occurs because the gut barrier, which has many elements to it, has somehow been compromised.
- The gut barrier functions like a security gate, letting the good fellas in (nutrients and water) and keeping the bad ones out (toxins and pathogens).
If you’re wondering if your symptoms are related to increased intestinal permeability, the comprehensive team at Oshi Health can help.
Personalized answers for your gut health
Does it feel like your digestive symptoms have taken over your daily routine? You’re not alone—and we’re here to guide you toward real, lasting solutions.
Oshi Health takes an evidence-based, concierge approach to diagnostic testing and screening. We work with you to understand your unique symptoms and decide if tests are needed. Our goal is to recommend only what makes sense for your specific situation. You can expect:
✔ Clinically-backed testing recommendations tailored to you
✔ Scheduling support from our care coordinators
✔ Clear explanations of what your results mean
✔ And so much more!
Ready to find lasting symptom relief?