A colonoscopy is the gold standard screening for colorectal cancer. It’s recommended for individuals 45-75 years old, usually every ten years. The procedure saves lives by detecting cancer in its early stages, but a colonoscopy is only as effective as its prep. So what should you do if colonoscopy prep is not working after five hours, aka you have not yet had a bowel movement despite taking a prescribed laxative? Here’s what to do–plus a step-by-step guide to good colonoscopy prep.
A colonoscopy is the most effective screening for colon cancer, but like an athlete competing in the Olympics, a colonoscopy is only as good as its “training” (aka the prep you do beforehand). To prepare for a colonoscopy, your GI provider will give you a laxative, typically referred to as colonoscopy prep solution, that you’ll most likely ingest the night before and/or morning of the screening. The laxative should cause (sorry for potential TMI), diarrhea, meaning you’ll probably want to stay close to the bathroom during this time. You’ll also follow a low fiber diet leading up to the screening, a clear liquid diet the day before, and stop eating the night before and morning of the colonoscopy. But what if you take your solution as instructed, and that colonoscopy prep is not working after five hours?
Not seeing any, um, movement by the 5-hour mark can feel nerve-wracking–and can open the door to a lot of questions. (Did I do something wrong? Should I still show up to my screening? And perhaps the most stressful question for many, will I poop during my colonoscopy? ) These questions are all valid, especially since up to a quarter of colonoscopies have bad preparation, and prep directly impacts the screening’s effectiveness. “The hardest part is the prep, but it’s worth it,” explains Michael Bass, MD, a gastroenterologist, hepatologist, and founding medical director of Oshi Health, “because a clean colonoscopy can literally save your life.”
Why is colonoscopy prep so important?
To understand why colonoscopy prep is important, we have to take a scoping look (pun intended) at what a colonoscopy is. During a colonoscopy, a doctor uses a scope, a long thin tube with a light and camera on the end, to look inside the rectum and colon. They’re scanning for abnormal polyps, ulcers, inflamed tissue, and other early signs of colorectal (colon) cancer.
To accurately screen for colorectal cancer, a doctor, typically a gastroenterologist, must have a good visual of the colon, and that’s where colonoscopy prep comes in. “Prep is everything. If the colon isn’t clean, I can’t see polyps or early cancers,” says Dr. Bass, “The test is only as good as the prep.” And cleaning the colon means removing all the stool from your system.
Signs of a good vs. bad colonoscopy prep
In about 10-20% of colonoscopies, the visuals captured by the camera are obstructed, often because of bad bowel prep. But how can you tell if you’ve had good or bad colonoscopy prep? It all comes down to your poop. “A good prep typically means watery, clear, or yellow liquid coming out,” says Dr. Bass, “If it’s still brown or full of solid pieces, the colon isn’t ready.”
What happens if colonoscopy prep doesn’t work?
If colonoscopy prep doesn’t work, your provider may not be able to get an accurate visual of the colon and rectum. The procedure might need to be rescheduled or repeated, as will the colonoscopy prep. When bad colonoscopy prep is the reason the procedure doesn’t work, your gastroenterologist will probably provide alternative prep methods or additional recommendations for the next round.
Colonoscopy prep not working after 5 hours: possible reasons
You’ve taken your colonoscopy prep liquid and followed your gastroenterologist’s recommended diet, but it’s been five hours and the bowel movements haven’t started. Usually, diarrhea begins within minutes to three hours after the prep solution. If it doesn’t, that’s not typical, and it can be stressful, since poor prep may mean having to repeat the whole process and the screening itself.
But now is not the time to panic. Instead, focus on troubleshooting. Possible reasons for bowel prep to work slower than expected include:
- Constipation before taking prep solution: Constipation is when someone experiences difficulty passing bowel movements, and chronic constipation can slow bowel function, impacting when prep solutions work. Certain medications, supplements, habits, and medical conditions may cause constipation.
- Incorrect dosage: Perhaps the most common reason, an incorrect dosage can lead to colonoscopy prep not working.
- Inadequate hydration: Ahead of prep, you want to stay hydrated, which can help bowel movements remain regular and protects against dehydration, which can be a complication of colonoscopy prep.
- Not following dietary guidelines beforehand: Your GI provider will provide a colonoscopy prep diet (more on this below) that will ensure there’s no leftover residue in the colon and rectum and that bowel movements are more than regular after taking the bowel prep liquid.
No matter the reason your prep isn’t working, you’re not alone in finding a solution. “If you’ve taken the prep and nothing’s happening after five hours, call your doctor’s office,” advises Dr. Bass, “Sometimes an extra dose or a different laxative is needed.”
Troubleshooting colonoscopy prep issues
If not experiencing bowel movement ahead of a colonoscopy, any of the above issues could be at play. There are a few steps you can take to hopefully get the bowels moving:
- Increase hydration leading up to your colonoscopy, sticking to clear fluids starting 24 hours before your procedure and ceasing consumption by two hours prior.
- Engage in gentle physical activity, like a walk around the living room or stretching
- Reread laxative instructions and any additional guidance provided by your doctor’s office
And yes, we sound like a broken record, but if prep still isn’t working, contact your doctor’s office again. They can provide other options that are customized to your situation.
Optimizing your colonoscopy prep experience
Most of us don’t enjoy colonoscopy prep, which is why you want to optimize the experience now versus repeating it later. And good prep starts once you have a date for the colonoscopy and instructions from your doctor.

Once you have a colonoscopy date
- Read all instructions from your GI provider, typically one week before the colonoscopy, 3 days before, and one day before.
- Plan out some meals with foods that will be easy to digest in the coming days.
- Prepare a comfortable bathroom environment and make any necessary arrangements to be at home the day before and of your colonoscopy.
- Arrange a driver to take you to and from your screening.
Five days before your colonoscopy
- Stop supplements and medication containing aspirin or ibuprofen. Acetaminophen is ok to take.
- Eat easy-to-digest foods, so your colon is as empty as possible ahead of the procedure.
- Avoid fatty or difficult to digest foods.
- Stay hydrated.
| Foods to eat | Foods to avoid |
| White bread | Foods containing nuts and seeds |
| White pasta and noodles | Popcorn |
| White rice | Whole grain bread or pasta |
| Skinless potatoes | Brown or wild rice |
| Plain meat, such as chicken or fish without sauces | Cereals, including granola and oats |
| Fruit without skin | Fruit with skin |
| Cooked veggies without skin | Vegetables with skin |
The day before your colonoscopy
- Take any prescribed medications one hour before starting bowel prep.
- Follow bowel prep instructions from your provider.
- Drink at least 12 glasses of water (8-10 ounces each) the day before.
- Usually you will take half your bowel prep the night before. If your procedure is scheduled for the AM, you’ll take the solution the previous afternoon. If your colonoscopy is scheduled for the afternoon, you’ll take the prep solution the evening prior, around 6pm. The other half of the solution, you’ll take the morning before the procedure. This method is called ” split prep,” and it often leads to a more thorough emptying of the colon, improving visibility during the colonoscopy.
- Consume clear liquids, which make it easier to see the colon. Unclear liquids often distort a gastroenterologist’s view, sometimes looking like blood in a colonoscopy.
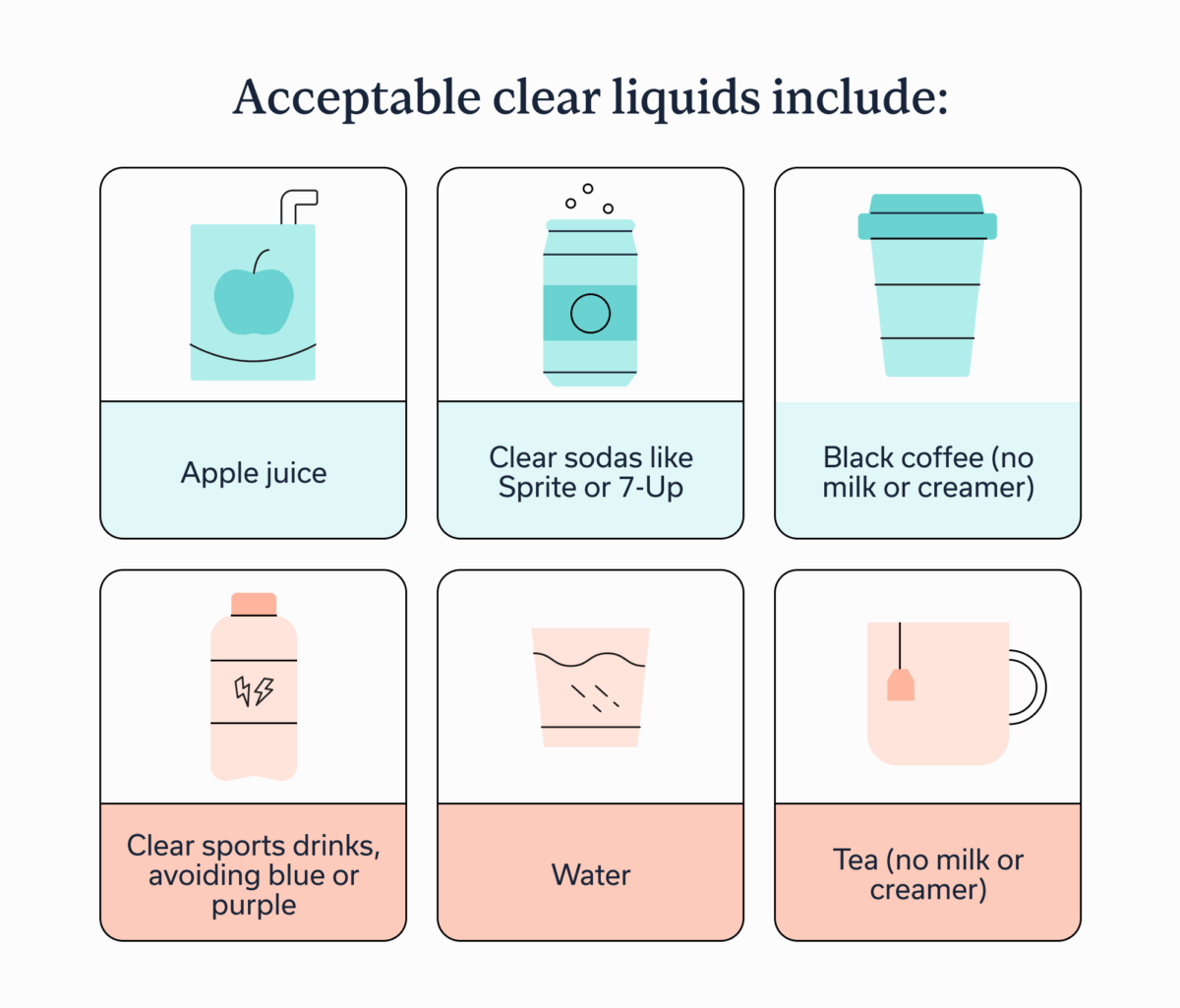
If you’re confused about what clear liquids are, you’re not alone. A good test for if a certain drink makes the cut is to place a glass of the liquid on top of a page with words. If you can read the words through the glass, it’s clear. The one exception to that rule is coffee, which can be drunk black with no milk or creamer.
Acceptable clear liquids include:
- Apple juice
- Clear sodas like sprite or 7-up
- Black coffee (no milk or creamer)
- Clear sports drinks, avoiding blue or purple
- Water
- Tea (no milk or creamer)
The day of your colonoscopy
- Only drink bowel prep, stopping even that four hours before surgery.
- Also around the four-hour mark, avoid putting any substances into your mouth, including food, drinks, cigarettes, chewing tobacco, and chewing gum. This ensures your stomach is completely empty and your doctor can get an accurate view.
- You should be able to return to a normal diet the evening of your procedure, but a doctor will provide any specific dietary guidance for after, along with tips to help with recovery.
- Avoid alcohol, signing legal documents, and driving until the day after the procedure because of the sedatives used during a colonoscopy.
Easiest colonoscopy prep to tolerate
Colonoscopy prep liquids can be difficult to tolerate, with some people reporting side effects like nausea, vomiting, and abdominal pain. Fortunately, there are some steps to make colonoscopy prep more comfortable.
The first is to practice split-dose prep, which is when you take half the prep the afternoon or evening before and the other half the morning of. Not only can this reduce side effects, it’s also associated with better cleansing and a clearer visual during the colonoscopy.
Prep is also easier to tolerate when the prep liquid is a low-volume solution. These solutions cause fewer GI side effects, often taste better than high-volume solutions, and come in a liquid or pill form. MoviPrep, Suprep, Clenpiq, and SUBTAB are popular options that fall into this camp. That said, your doctor should recommend which option is best based on your health needs, whether it’s one of the three we mentioned or something else.
Key takeaways
- A colonoscopy is the gold standard for detecting colorectal cancer, but it’s only as good as its preparation.
- For good colonoscopy prep, follow all instructions from a provider, stick to an easy-to-digest diet a few days before and a clear liquid diet the day before and day off.
- If you’ve taken colonoscopy prep liquid and aren’t having bowel movements, call your doctor’s office. They can adjust the dosage as necessary and provide any ways to troubleshoot that are specific to your situation.
Frequently asked questions (FAQs)
-
If colonoscopy prep isn’t kicking in, it could just be that you need more time. Prep solutions don’t work instantly; they often take a few hours to kick in. During that time, stay hydrated with clear liquids and move around the house, which could look like walking or following along with a gentle yoga video. If five hours passes without results, call your doctor’s office.
-
If you’re not pooping during colonoscopy prep, the first thing to do is stay calm. Prep can take up to three hours to work, and it often works better alongside adequate hydration and some light movement. If five hours have passed and you still haven’t had a bowel movement, call your doctor’s office for additional guidance.
-
Signs of good or bad colonoscopy prep are found in your stool. If stool is a brown liquid or has solid chunks in it upon completing the colonoscopy prep, colonoscopy prep probably failed. A good colonoscopy prep looks like stool that is clear or yellow and fully liquid. Other signs of a failed colonoscopy prep is if you haven’t had diarrhea-like bowel movements or you’re experiencing severe GI symptoms, such as debilitating abdominal pain or ongoing vomiting.
-
Drinking extra water can help with colonoscopy prep. A good guideline is to drink 12 8-10 ounce glasses in the hours leading up to your colonoscopy. The extra water ensures you won’t become dehydrated during the prep and helps make the colon more visible during the screening.
-
If the prep fluid is not working, contact your doctor’s office. They can help identify and fix the specific issue, which may mean having another dose of the prep liquid or pill, increasing your intake of clear liquids, or moving around the house and stretching in order to get things moving.
Oshi is your partner in digestive health
Feel like your digestive concerns are running your life? You’re not alone—and we’re here to help you find lasting relief.
Oshi Health GI providers, gut-brain specialists, and registered dietitians work together to address your symptoms and find solutions that actually work for you.
Whether you’re dealing with chronic digestive issues or unpredictable symptom flare-ups, our GI specialists deliver:
✔ Personalized care plans tailored to your lifestyle
✔ Science-backed strategies to calm your gut
✔ Compassionate, whole-person care
✔ And so much more!
Ready to take control of your gut health?