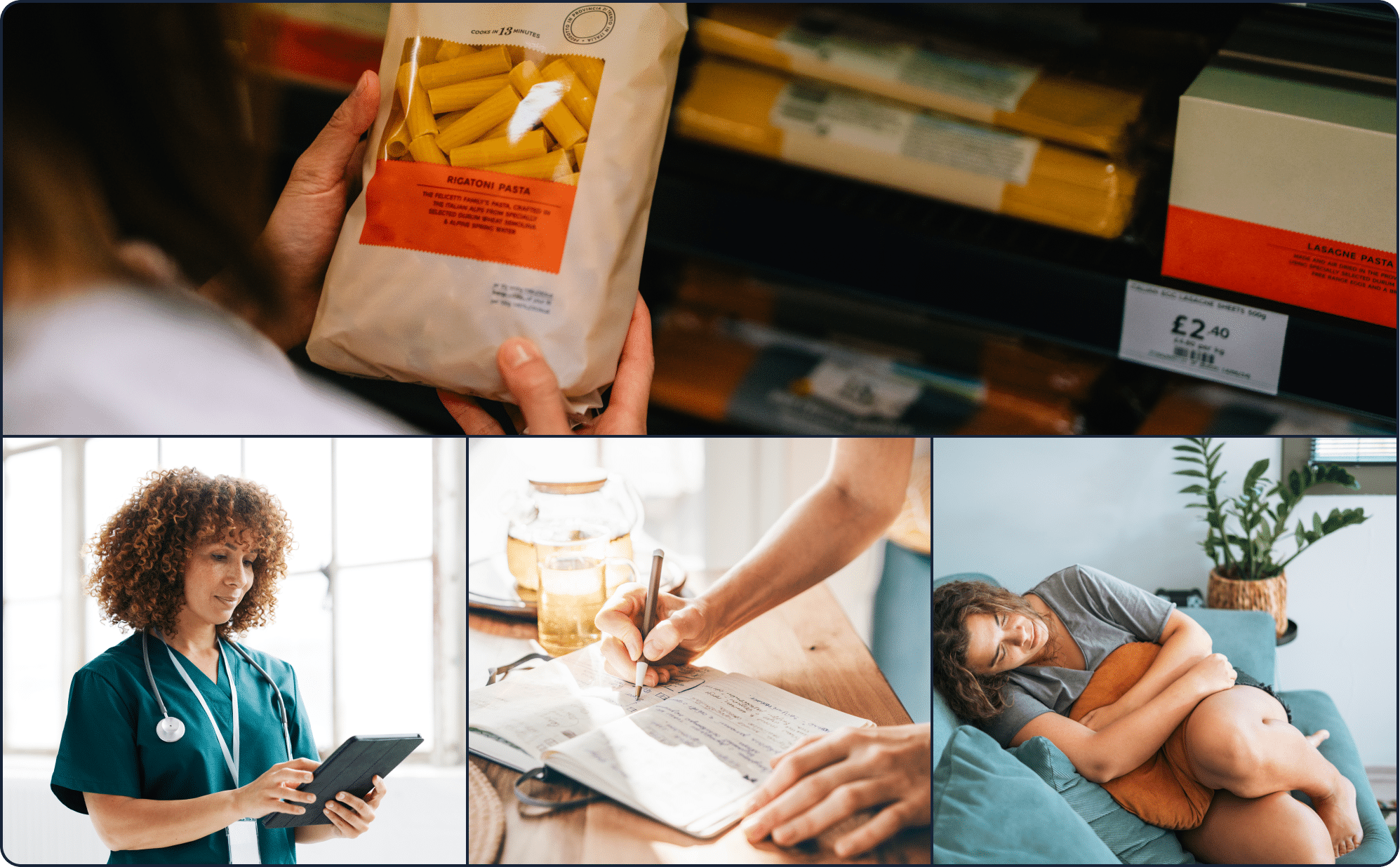
If you often feel gassy or constipated after eating pasta or pastries, gluten might seem like the obvious culprit. But while gluten sensitivity is one possibility, these symptoms also show up with many other gut issues. Here’s how to test for gluten intolerance and its many lookalike conditions.
“Going gluten free” is a buzz phrase these days, so much so that gluten is often mislabeled as an “unhealthy” food—or people automatically assume gastrointestinal (GI) symptoms like abdominal pain or bloating are due to a gluten sensitivity. The truth behind gluten and whether or not you are intolerant is a bit more complicated. Symptoms of gluten intolerance are often the same one would experience with other conditions, including Celiac disease, wheat allergies, and others. This is why understanding how to test for gluten intolerance is often misunderstood too.
Too often, we think we can just go gluten-free without any medical guidance. This approach misses the diagnosis phase and isn’t the most effective way to manage symptoms. Instead, here’s how to accurately find out what’s causing your GI symptoms after eating foods with gluten.
Understanding gluten intolerance and gluten sensitivity
Before we dive into gluten intolerance, let’s take a moment to make sure we have a clear understanding of what gluten is first. The term has become ubiquitous, with one in five Americans thinking that keeping gluten off your plate is a healthy choice.
Gluten is simply a protein found in wheat, rye, and barley—and many foods with gluten contain nutrients that help make up a balanced diet. Some medications and supplements also contain gluten. Despite its reputation, gluten, in and of itself, can be part of a healthy diet for most people.
Part of the reason gluten is mislabeled is because it often gets processed away from its “whole” form. This occurs when gluten is found in ultra-processed foods, like baked goods, candies, hot dogs, and ice cream. But it can also be an ingredient in healthy foods like some soups, whole wheat pasta, and bulgur, making it more of a neutral ingredient.
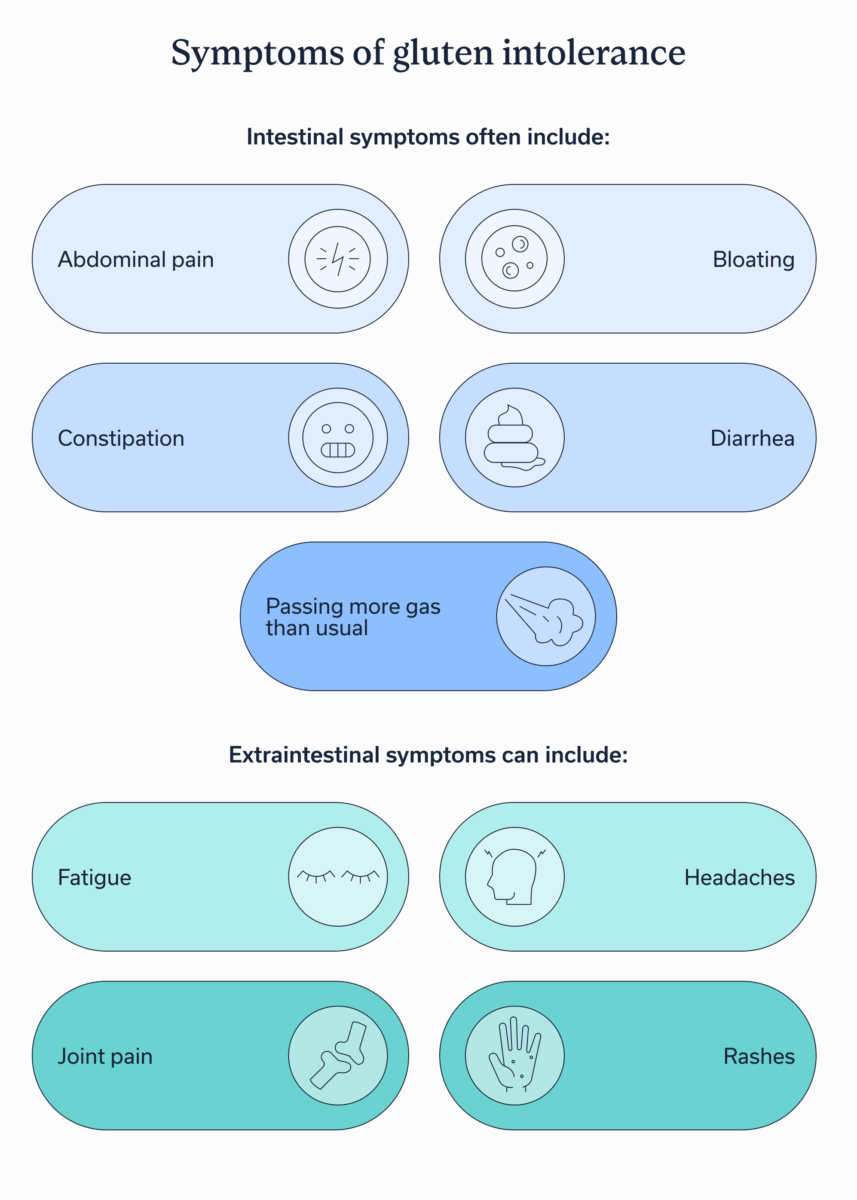
That is, of course, unless you have gluten intolerance or sensitivity (or to use its official medical term, non-celiac gluten sensitivity.) Those with a gluten sensitivity experience intestinal and extraintestinal symptoms when they ingest gluten.
Intestinal symptoms often include:
- Abdominal pain
- Bloating
- Constipation
- Diarrhea
- Passing more gas than usual
Extraintestinal symptoms are less common than GI symptoms and can vary widely—from headaches to fatigue to brain fog.
Gluten intolerance vs. celiac disease: key differences
Gluten intolerance and celiac disease are two conditions that are often mixed up, and without proper testing, it can be hard to tell which is causing symptoms.
“Celiac disease is an autoimmune disorder where the immune system attacks the lining of the small intestine when gluten is consumed,” explains Megan Koistinen, MS, RD, LDN, lead registered dietitian at Oshi Health. Celiac disease is diagnosed with a lab test whereas gluten sensitivity and gluten intolerance are typically more general terms and are used interchangeably to describe food intolerances. Both an “intolerance” or “sensitivity” can cause temporary digestive issues like bloating, fatigue, or abdominal discomfort but do not cause any damage to the digestive tract.”
While the two share many symptoms, a differential diagnosis is required. Left undiagnosed and untreated, celiac disease leads to more serious symptoms, such as bone loss, malnutrition, and neuropathy or problems with the nervous system. It also increases the risk of developing intestinal cancer, cancers in the lymphatic system, and oropharyngeal cancers, which develop the middle section of the throat.
Step-by-step guide: How to test for gluten intolerance properly
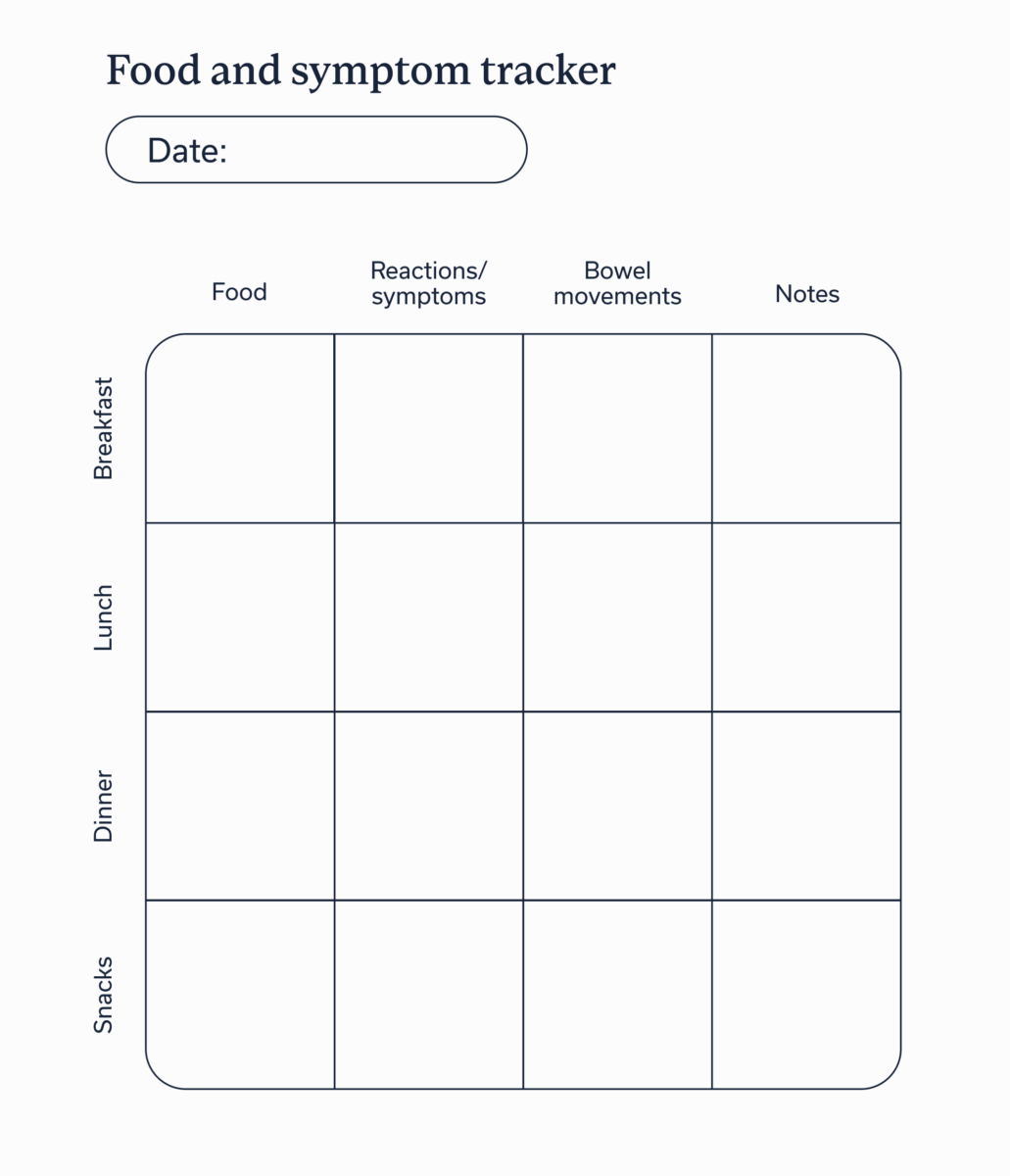
If you suspect you may be sensitive to gluten, start tracking your symptoms (we recommend using a paper journal or the notes app on your phone). When you log symptoms, write down what you’re feeling, any notes on severity, what foods you consumed and how much, as well as the time of day when symptoms occurred. If you felt bloating and abdominal pain after eating a bagel on Saturday morning at 8am, for example, you’d log that in your gluten sensitivity tracker.
“From there, consult with a healthcare provider who can help determine if celiac testing is most appropriate. This is typically used to rule out celiac disease,” says Koistinen, “If the tests are negative, it is generally recommended to work with a registered dietitian who can help guide you through a gluten elimination for about four to six weeks then work toward a gluten reintroduction or ‘challenge’ if appropriate.”
For easy reference, the exact steps for determining if you have a gluten sensitivity often look like:
- Track symptoms and what foods seem to have caused them.
- Consult a healthcare provider, ideally a gastroenterologist or GI provider, showing them your symptoms.
- The healthcare provider will order celiac testing, if appropriate. Continue eating gluten up until the test for accurate results.
- If tests are negative, begin a gluten elimination diet with a GI registered dietitian.
- Reintroduce gluten to confirm results if necessary.
Testing for celiac disease, gluten intolerance, or gluten sensitivity
When we talk about testing for celiac disease, we don’t mean a test with multiple choice questions or essays, though there may be some needles. The first line test is generally a lab test followed by a biopsy of the small bowel for confirmation.
When someone has celiac disease, they have higher levels of certain antibodies, which are protective proteins the immune system produces. The immune system creates these antibodies because it views gluten as a threat, similar to how it would produce antibodies to fight the flu. A blood test can detect and measure these antibodies, which will give your healthcare provider the information they need to either provide a clear diagnosis or rule out celiac disease.
There are four commonly used antibody blood tests for celiac disease:
- Tissue transglutaminase antibody (tTG), IgA test: The most common of the four, this test measures the tTG subset of total IgAl
- Immunoglobulin A (IgA) test: This test looks for total immunoglobulin A.
- TTG IgGt test: Immunoglobulin G is another antibody associated with celiac disease, and it’s detected by this test.
- Deamidated gliadin peptide (DGP) antibodies test: If someone has lower immunoglobulin A levels but a provider suspects celiac disease, they may order this test. It’s also the preferred option for patients under two years old.
To confirm blood test results, a provider may order a biopsy. A biopsy is a procedure to remove tissues from a specific part of the body—in the case of celiac disease, the small intestine—the first and second portion of the duodenum. That sample is then examined under a microscope for any damage in the small intestine caused by celiac disease- classic histologic changes of celiac enteropathy
No matter which test you take, continue eating gluten up until the test. If you try to cut it out on your own, a test for celiac disease may not provide accurate results.
Once a provider has ruled out celiac disease (and possibly a few other conditions), there are no needles or biopsies moving forward. In fact, there are no accurate tests to confirm gluten sensitivity.
If you do have celiac disease, gluten intolerance or gluten sensitivity
If your provider determines you do have celiac disease, you should see a gastroenterologist as well as a registered dietitian (RD). They’ll work with you to come up with a diet plan that will avoid gluten while keeping you well nourished. You may also want to meet with a GI psychiatrist to incorporate gut-brain therapies and address the mental aspects of the fact that your celiac diagnosis will require some lifelong changes.
It’s important to note that the only treatment for celiac disease is a strict gluten-free diet. If you are negative for celiac, however, but believe you are sensitive to gluten, there are a few different approaches you might take.
“As with all intolerances, the most accurate way to determine how a food might be affecting you is through strategic diet modifications and monitoring symptoms with a registered dietitian,” says Koistinen.
That often starts with a gluten elimination diet, which is where someone removes all sources of gluten from their plate for four to six weeks. During that time they track symptoms, noting if they improve or stay the same.
If you’re feeling overwhelmed at the prospect of identifying which foods, medicines, and supplements do and don’t contain gluten, you can rest easy knowing that an elimination diet is conducted under the guidance and supervision of an expert, typically a GI registered dietitian (RD). The provider can detail what the elimination diet looks like, answer any questions you have, and help you interpret any changes in symptoms.

Around the six week mark, the RD may introduce a “gluten challenge” which is a strategic reintroduction of foods that contain gluten to see if symptoms reappear. While the reintroduction phase is more common in other elimination diets, such as the FODMAP diet, it may be useful in confirming a gluten sensitivity. Like with the elimination phase, you only want to conduct a gluten challenge in partnership with a RD and will want to log symptoms and what you eat during this phase.
Other factors that may cause similar symptoms
Part of the reason a gluten sensitivity is so difficult to nail down is because its symptoms are shared among a few different conditions. We’ve already discussed celiac disease, but it’s not the only look-alike condition:
| What it is | Common symptoms | How it’s diagnosed | |
| Gluten intolerance | A food sensitivity where someone experiences temporary digestive symptoms after eating gluten | Bloating, gas, diarrhea, constipation, fatigue, headaches | Ruling out any other conditions followed by a gluten elimination diet |
| Celiac disease | An autoimmune disease where someone’s body cannot process gluten. | Bloating, gas, diarrhea, constipation, damage to the small intestine | Blood testing and/or a biopsy of the small intestine |
| Irritable bowel syndrome (IBS) | A chronic condition where the colon or small intestine is sensitive to normal GI functions | Abdominal pain, bloating, gas, diarrhea, constipation | Thorough review of medical history and symptoms, sometimes supported by additional testing |
| Lactose intolerance | Difficulty processing lactose, a sugar found in dairy products | Bloating, gas, diarrhea, nausea, vomiting | Review of medical history and symptoms in tandem with a lactose elimination diet |
| FODMAP sensitivities | Sensitivity to FODMAPs, a group of carbohydrates that digest slowly in the small intestine | Abdominal discomfort, bloating, constipation, diarrhea, pelvic pain | Ruling out other conditions, followed by the FODMAP diet |
After celiac disease, a wheat allergy is the condition whose symptoms most closely mimic gluten intolerance. A wheat allergy is when someone is allergic to wheat in general, not just gluten (which is a protein found in wheat). It can cause similar GI symptoms and, like gluten sensitivity, it doesn’t harm the small intestine.
It does, however, come with different extraintestinal symptoms, including itchy eyes or difficulty breathing. Symptoms usually occur one to three hours after being exposed to wheat. This allergy is confirmed via an allergy skin prick test, during which a doctor pricks the skin with possible allergens—in this case wheat—and monitors how the patient reacts.
Another condition that may present with similar symptoms is irritable bowel syndrome (IBS). IBS is when the colon or small intestine are highly sensitive to gut functions, such as contractions or passing gas. IBS causes similar symptoms to a gluten intolerance, like bloating and abdominal pain.
To make matters more confusing, many with IBS develop food sensitivities, which can include gluten. A GI provider must diagnose IBS, usually after reviewing your medical history and current symptoms, which is sometimes combined with additional testing.
A gluten intolerance also shares symptoms with other food sensitivities, chief among them intolerance of lactose and/or FODMAPs.
Lactose intolerance is when someone has difficulty processing lactose, a sugar found in milk and other dairy products. Common symptoms include bloating, gas, and diarrhea, which are also commonly experienced with a gluten intolerance. It is typically diagnosed after a provider examines your medical history and current symptoms and oversees a lactose elimination diet.
FODMAP is actually an acronym for four carbohydrate subgroups: fermentable oligosaccharides, disaccharides, monosaccharides, and polyols. All of these digest slowly in the small intestine. For some individuals, one or more of these groups can cause GI symptoms that are similar to a gluten sensitivity. To figure out if, and which, FODMAPs are causing GI symptoms, someone will usually complete the low FODMAP diet under the supervision of a GI provider or GI registered dietitian.
When to seek medical advice
It’s probably pretty clear by now that the symptoms you suspect are caused by gluten sensitivity might stem from many other conditions. Getting to the bottom of which are behind your symptoms will be a lot easier with the support of an experienced GI provider.
“When and if you experience ongoing GI issues (bloating, diarrhea, constipation, etc.), unexplained weight loss, brain fog or fatigue, nutrient deficiencies, a family history of celiac disease or an autoimmune disorders, you should consider seeking medical help,” advises Koistinen.
Key takeaways
- A gluten intolerance or sensitivity is when someone experiences uncomfortable digestive symptoms whenever they eat gluten, a protein found in wheat, barely, and rye.
- Common symptoms include abdominal pain, bloating, passing more gas than usual, constipation, diarrhea, fatigue, headaches, and joint pain. These symptoms occur with many other conditions, including celiac disease, IBS, and other food sensitivities, including FODMAP and lactose intolerance, which is why proper testing is recommended before beginning a gluten-free diet
- If you suspect a gluten intolerance, consult a GI provider, such as the team at Oshi Health, who can test for celiac disease and oversee a gluten elimination diet in order to determine what’s causing your symptoms.
Frequently asked questions (FAQs)
-
There is no official test for gluten intolerance. If you suspect a gluten intolerance, consult a GI provider who can assess symptoms. Usually, they’ll order bloodwork and possibly a biopsy of the small intestine to rule out celiac disease before overseeing a gluten elimination diet.
-
To check if you’re sensitive to gluten, visit a GI provider who can assess symptoms and determine the right course of action. Typically, diagnosis involves ordering bloodwork and possibly a biopsy of the small intestine to rule out celiac disease before starting a gluten elimination diet. By eliminating gluten, you and your provider can determine if that is what’s causing symptoms.
-
Gluten is a protein found in wheat, barely, and rye, so you’ll want to avoid foods with these ingredients. Foods to avoid include baked goods, pasta, breads, cereal, and beer, unless any of the aforementioned clearly state they are gluten-free.
-
A gluten intolerance does not go away and requires a lifelong commitment to a gluten-free diet. Once someone with a gluten sensitivity eliminates gluten from the diet, symptoms usually go away.
Oshi is your partner in digestive health
Feel like your digestive concerns are running your life? You’re not alone—and we’re here to help you find lasting relief.
Oshi Health GI providers, gut-brain specialists, and registered dietitians work together to address your symptoms and find solutions that actually work for you.
Whether you’re dealing with chronic digestive issues or unpredictable symptom flare-ups, our GI specialists deliver:
✔ Personalized care plans tailored to your lifestyle
✔ Science-backed strategies to calm your gut
✔ Compassionate, whole-person care
✔ And so much more!
Ready to take control of your gut health?