Irritable bowel syndrome (IBS) can cause uncomfortable gastrointestinal symptoms, like abdominal pain, diarrhea, and constipation. A good IBS treatment plan often includes dietary adjustments as the first line of treatment, and should be customized to your unique IBS triggers and symptoms.
For people with irritable bowel syndrome, the telltale symptoms of a flare—bloating, diarrhea, constipation, cramping, and abdominal pain—are impossible to ignore. A bad day can leave you wondering, “Was it something I ate?” It’s not in your head—an overwhelming majority of people living with IBS have found that different, specific foods make their symptoms worse.
The tricky thing is that there isn’t a one-size-fits all approach to treatment of IBS flare symptoms, including dietary guidance. And navigating the plethora of information on diet and nutrition for IBS can feel extremely frustrating. That said, there are a few dietary approaches you may want to discuss with a gastrointestinal (GI) registered dietitian—and some foods that are usually best to avoid.
Understanding IBS and potential dietary triggers of a flare
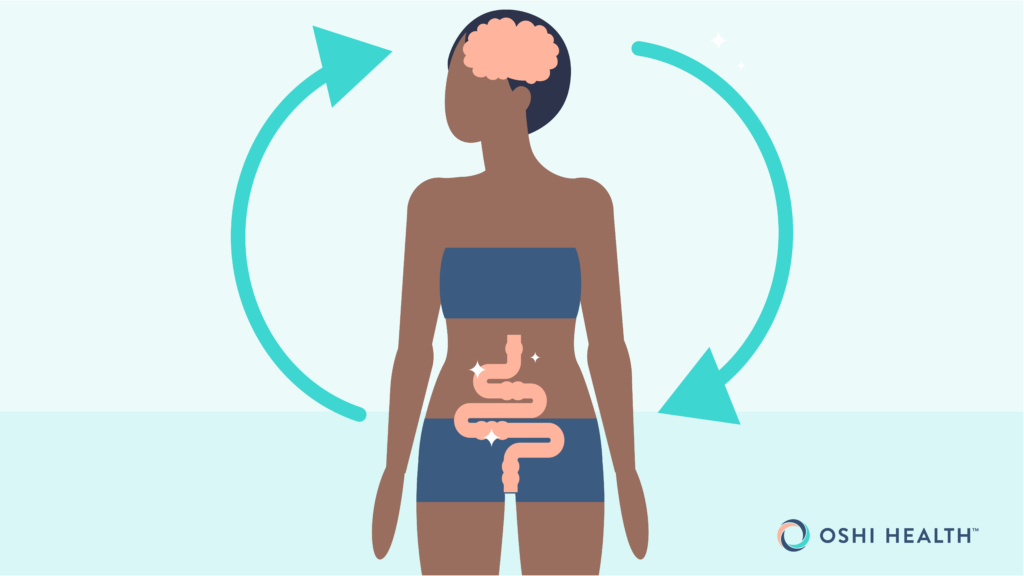
Out of all the gastrointestinal (GI) conditions, IBS is among the most common, affecting about 10-15% of the total population. This chronic condition is a disorder of gut-brain interaction (DGBI) where your GI tract is more sensitive to normal functions like digesting food and having a bowel movement. This sensitivity may lead to a variety of symptoms, such as:
- Abdominal pain
- Abdominal cramping
- Bloating
- Changes in bowel movements
- Excess gas
- Feeling like you haven’t finished a bowel movement
- Mucus in your stool
- Urgent need for a bowel movement (diarrhea)
Symptoms often get worse if you’re going through a stressful event, a bacterial infection (especially within the GI tract), if you have a food intolerance or sensitivity, or even during your period, for menstruating females.
Types of IBS
The above list of symptoms is hefty, but not everyone experiences every IBS symptom. Having said that, abdominal pain and changes in stool are the two defining symptoms for a diagnosis. Typically, doctors also break IBS down into three main types:
- IBS-C (Constipation): Characterized by infrequent, difficult bowel movements, and hard or lumpy stool.
- IBS-D (Diarrhea): Marked by overly frequent bowel movements, watery stool, and a persistent need to poop.
- IBS-M (Mixed): A type that oscillates between symptoms associated with IBS-C and IBS-D.
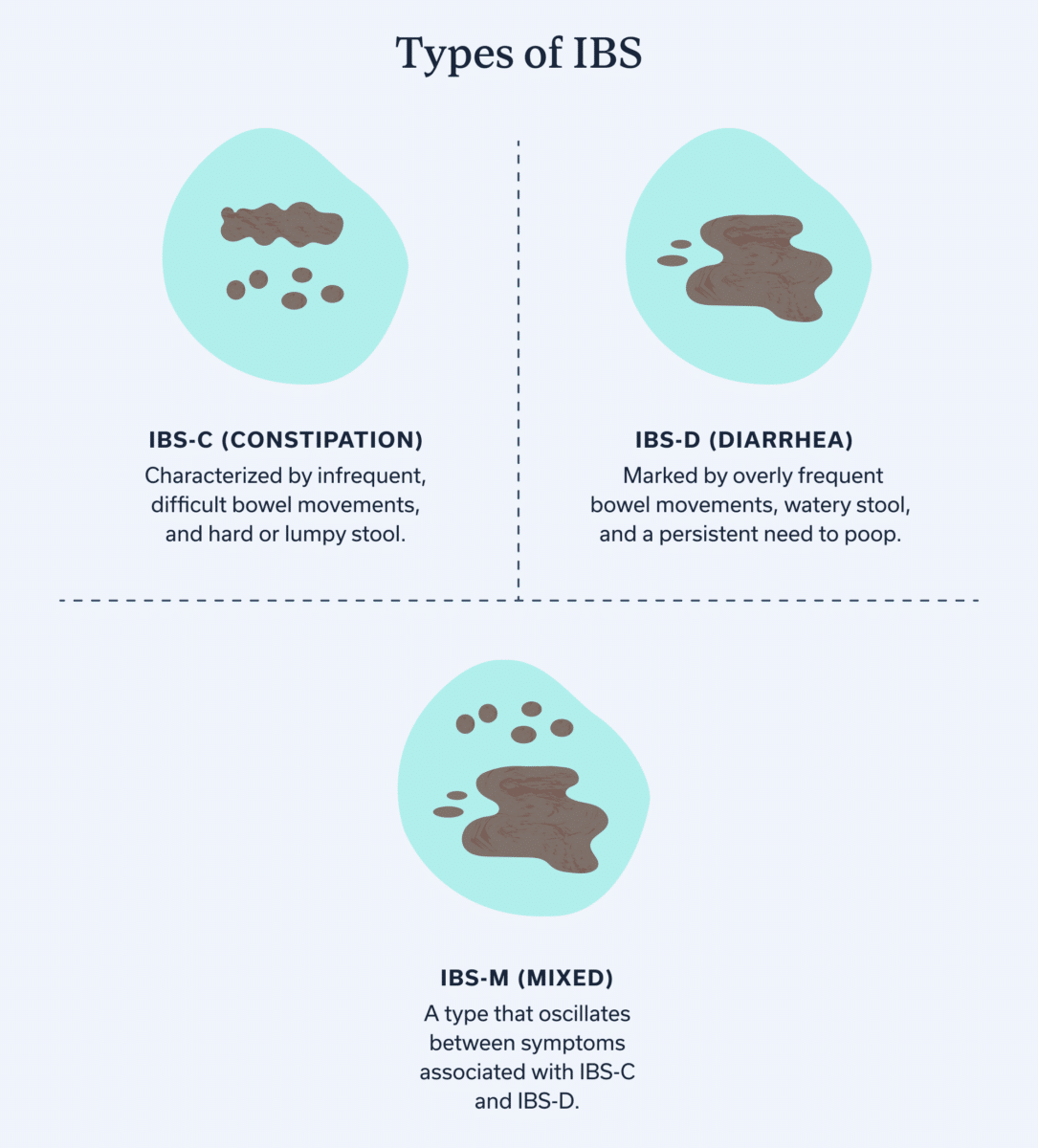
Learning your type can help you identify what makes your IBS tick. Often, those with the same IBS type experience similar symptoms and dietary triggers. When you’re working with a GI provider, knowing the type of IBS you have can help inform your treatment and any lifestyle changes. If you don’t know your type, a GI provider can help you figure that out too!
The role of diet in IBS symptoms
When I leave the house, there are two types of trips I tend to take. One type is when I pinpoint an exact location and head there and back. The other is when I slowly wander through multiple stores, perhaps stop for a coffee, and then meander my way through errands, maybe backtracking a little before I reach my final destination. IBS treatment is more like the second trip: There isn’t one direct route there and back when it comes to tackling this GI condition.
One of the most popular routes on the metaphorical IBS road trip? Changing your diet. 84% of those with IBS report that food triggers their symptoms, meaning diet improvements can have a big payout for many with IBS. But there’s one big caveat—those dietary changes will differ from person to person, depending on your unique food triggers.
When you find the right diet to placate your IBS symptoms, it can feel like striking gold. A 2021 meta-analysis acknowledges there’s no set IBS diet, but states that in most studies, people with IBS experienced symptom relief after they adjusted their diet based on evidence-based recommendations.
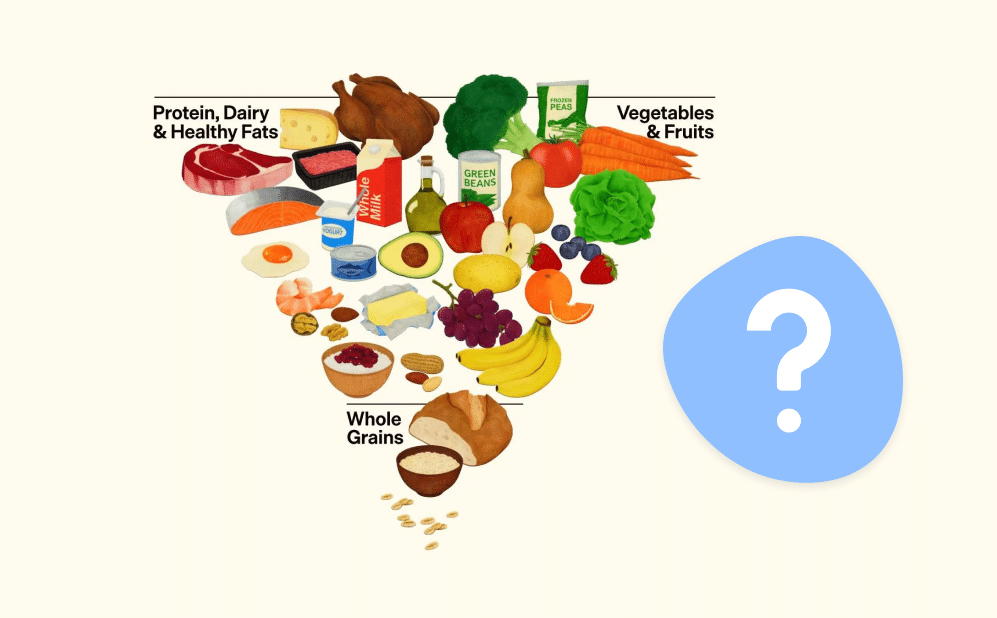
Dietary approaches for IBS management
As mentioned, the exact diet you follow should be personalized to tackle your symptoms—and a customized IBS treatment plan is built in tandem with a registered dietitian and other GI specialists.
The dietary approaches below can give you a rough idea of potential diets for IBS. Feel free to bookmark this page for later and bring up any of the diets below with your GI provider, who will partner with you to decide which dietary approach is right for you. They can also help you navigate the diet as well so you stay well nourished and don’t overly restrict yourself.
Low FODMAP diet
One of the most popular and clinically validated diets for IBS is the low FODMAP diet. In one 2022 study, this diet reduced IBS symptoms, including abdominal pain, bloating, and irregular bowel movements, for the majority of participants.
FODMAP stands for “fermentable oligosaccharides, disaccharides, monosaccharides and polyols.” This is a group of carbohydrates that provide food for bacteria in the gut, but can trigger IBS symptoms for certain individuals. Common foods that are high in FODMAPs include apples, beans, cashews, cow milk, and watermelon. With a low FODMAP diet, you temporarily eliminate all FODMAPs and then slowly reintroduce each group (starting with, say, disaccharides and then moving to add polyols, etc.) so you can figure out which specific foods trigger your symptoms.
If that summary sounds complicated, it’s because this diet is tricky. A low FODMAP diet should only be carried out under the supervision of a GI-specialized registered dietitian. And, despite its common usage, one third of individuals with IBS don’t benefit from a low FODMAP diet—yet another reason to consult a RD before making dietary changes.
NICE IBS guidelines
Coming from across the pond, the NICE guidelines were developed in the UK to help diagnose and treat IBS. These recommendations include dietary and lifestyle changes that may help manage IBS:
- Avoid fizzy drinks and alcohol when possible
- Avoid long gaps between meals or skipping meals
- Drink 8 cups or more of fluids a day, prioritizing water
- Eat fewer than three portions of fresh fruit a day
- Limit consumption of high-fiber foods and resistant starch (found in processed or re-cooked foods)
- Only have three cups of coffee or tea a day (maximum)
- Schedule regular meals
Additionally, the NICE IBS guidelines have suggestions for specific types of IBS. If you have IBS-D, the guidelines recommend avoiding sorbitol, a type of sweetener. Those who experience bloating may find it useful to incorporate oats and linseeds into their daily diet.
High soluble fiber diet
Following a low FODMAP can be difficult. A more accessible alternative is a high soluble fiber diet. Unlike low FODMAP, this diet doesn’t have hard and fast rules; instead, it simply means those with IBS may benefit from prioritizing soluble fiber in their diets. Soluble fiber turns into a gel-like substance once you eat it, which helps with gut motility and cultivates a healthy gut microbiome. It’s also slower to digest than insoluble fiber.
The 2021 American College of Gastroenterology Guidelines recommend soluble fiber for the management of IBS symptoms. While it may help with general IBS symptoms, it’s especially beneficial for those with IBS-C.
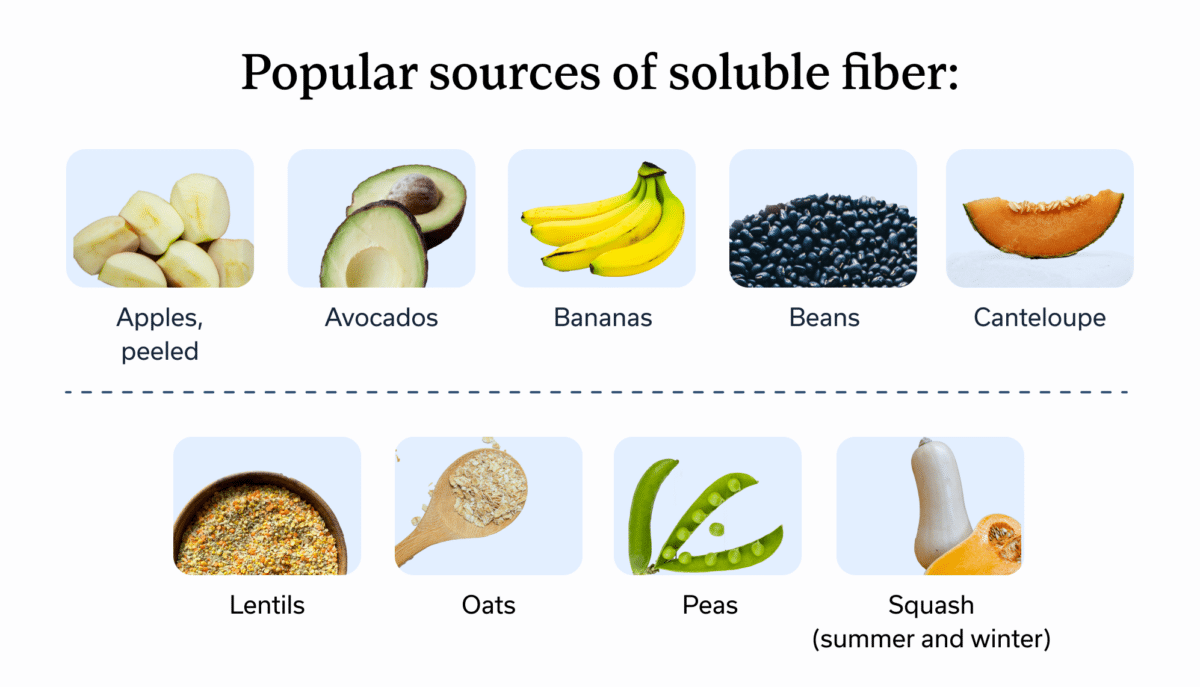
Some popular sources of soluble fiber include:
- Apple, peeled
- Avocados
- Bananas
- Barley
- Beans
- Cantaloupe
- Lentils
- Oats
- Peas
- Squash (summer and winter)
Gluten-free diet
Another common diet for IBS is going gluten-free. Admittedly, there’s less evidence to support this diet for IBS than the others listed—and certainly not everyone with IBS needs to ditch gluten. To date, removing gluten has not been proven to relieve IBS symptoms for those without an existing gluten intolerance or sensitivity.
But for those who have both a gluten sensitivity and IBS, a common overlap, the gluten-free diet may help relieve IBS symptoms. One study found those who had IBS plus a gluten sensitivity or intolerance had fewer IBS symptoms once they went gluten-free.
Gluten is a protein found in wheat and some other plants. It’s a common ingredient in many breads, pastas, pastries, cereals, and more. If an RD does recommend that you eliminate gluten from your diet, don’t fret: There are many gluten-free alternatives available, and they’re often just as delicious.
Other diet adjustments to consider
While an IBS diet isn’t one-size-fits-all, there are a few other adjustments that relieve symptoms for most folks. The first is staying hydrated. Hydration is important for us all, but those with IBS-D may be at higher risk since diarrhea can cause someone to lose too many fluids. Daily recommended water varies depending on the type of IBS and other factors, like the temperature outside and someone’s activity level.
Many people also find it helpful to eat smaller meals throughout the day in order to stabilize their digestion. The good news is: Smaller meals also equals more meals, and who doesn’t appreciate a bit more time to eat?
Foods to avoid for IBS relief
Determining what foods you should avoid is tricky—and 100% personal. That said, there are some foods that tend to trigger symptoms for many people with IBS. These include:
- Alcohol in large quantities. For reference, the maximum recommended daily intake is one drink or less for women, two for men.
- Artificial sweeteners. Many processed beverages contain artificial sweeteners, though they’re found in some foods as well.
- Caffeine. Don’t worry—you may still be able to have your morning coffee or tea. The key here is to enjoy caffeine in moderation.
- Fried or fatty foods. Those fries are best enjoyed occasionally, as fried or ultra-processed foods aren’t a staple in most recommended diets, whether or not you have IBS.
IBS meal planning tips
The only reason I don’t eat out three times a day is my meal planner. Knowing exactly what I’m going to make is a blessing at the end of a long work day—and makes cooking easier than ordering takeout. If you’re like me and want to have quick recipes on hand, we’ve got you covered.
Here’s what a day of eating with IBS-friendly meals could look like:
| Breakfast | Banana protein muffins |
| Lunch | Dough drop soup |
| Snack | Pumpkin paletas (popsicles) |
| Dinner | Lemon & dill boiled salmon with cooked veg of choice |
Before you dive into these recipes, consult an RD to make sure they work for you. Plus, an RD may be able to provide even more meal inspo that’s tailored to your specific triggers and symptoms.
Lifestyle tips to complement an IBS diet
Diet isn’t the only stop on the IBS journey. Other lifestyle changes can help manage symptoms and make your day-to-day less gut-wrenching (pun intended). One of the most common alongside diet and staying hydrated? Exercise. It’s time to lace up those sneakers; low to moderate intensity aerobic exercise (think: walking, jogging, biking) has been linked to improved psychological wellbeing and reduced IBS symptoms.
While diet, exercise, and hydration, could potentially be DIY-ed, it’s best to call in a professional. A team of GI providers can help analyze IBS symptoms and create a customized treatment plan that provides whole-person care.
An integrated team of GI specialists, working together for you
Our expert gastroenterologists, GI providers, registered dietitians, and gut-brain specialists are leaders in their fields, with advanced education and training in conditions like irritable bowel syndrome (IBS). Our comprehensive team approach is personalized to meet your unique needs and address the root cause of your symptoms.
Cognitive behavioral therapy (CBT) and stress management
Remember when we discussed that IBS has roots in the gut-brain connection? It turns out that addressing the brain side of that connection helps too. For many, cognitive behavioral therapy (CBT) helps address the negative emotions that may trigger or exacerbate IBS symptoms. Bonus points if you do CBT with a gut-brain specialist who can use this approach to address your gut health specifically.
Stress management techniques may help as well. Whether it’s yoga, meditation, or some other way you love to de-stress, time for stress management can help manage IBS flares.
Frequently asked questions (FAQs)
-
There isn’t one best diet for IBS. This GI condition causes different symptoms for different folks, meaning your diet should be customized to you. Common diets might include the low FODMAP diet, following the NICE IBS guidelines, a high soluble fiber diet, and a gluten-free diet, but a RD with experience treating IBS can help you determine the best dietary approach for your symptoms.
-
Generally, you’ll want to avoid high quantities of alcohol or caffeine, artificial sweeteners, and ultra-processed or fried foods. Other food triggers are more personal, which is why it’s important to work with an RD to determine yours.
-
The best way to treat an IBS flare-up depends on your symptoms and lifestyle factors. Working with a qualified GI provider can help you determine the best way to address symptom flares.
-
While there is a correlation between depression and IBS symptoms, depression most likely won’t cause IBS. In fact, there’s no exact known cause for IBS, though several factors are most likely at play, including a disruption in the gut-brain axis
Key takeaways
Just as no two snowflakes are alike, not two cases of IBS are the same. That means your IBS treatment plan, including your diet, should be customized to your symptoms and triggers. A GI provider and/or GI registered dietitian will help you customize the best IBS dietary practices for you. Those practices may include:
- Implementing a new dietary approach: There are many diets that can help with IBS flares. The ones that have been found beneficial in various clinical studies include a low FODMAP diet, a high-fiber diet, the NICE IBS diet, and a gluten-free diet.
- Prioritizing certain foods: Some tried-and-true faves among people with IBS include soluble fiber and hydrating foods.
- Avoiding certain foods: While specific food triggers vary, some common ones are large quantities of alcohol, caffeine, artificial sweeteners, ultra-processed foods, and fried foods.
If you’re looking for a GI provider or GI dietitian to help you develop your own IBS diet, check out Oshi Health. Our providers take a whole-person approach to IBS, meaning any treatment plan addresses all aspects of gut health, not just your symptoms.
Find lasting relief from IBS symptoms
Feel like irritable bowel syndrome (IBS) is getting in the way of enjoying your life? You’re not alone—and we’re here to help.
Oshi Health GI providers, gut-brain specialists, and registered dietitians work together to address symptoms like indigestion, bloating, and stomach pain, and find solutions that actually work for you.
Our GI specialists will work with you to reduce symptom flare-ups through:
✔ Personalized care plans tailored to your lifestyle
✔ Evidence-based IBS nutrition guidance
✔ Science-backed strategies to calm your gut
✔ Compassionate, whole-person care
✔ And so much more!
Ready to take control of your IBS symptoms?