Undiagnosed Symptoms Overview
Undiagnosed Symptoms Overview
You’re probably here because you’re experiencing gastrointestinal (GI) symptoms and aren’t sure what’s happening with your body or feel your symptoms don’t really fit any common GI conditions.
The truth is that many digestive diseases share common symptoms, and not everyone fits neatly into the diagnostic mold for a specific condition. Your experience with GI discomfort and symptoms might be completely different from someone else’s—even if you share the same diagnosis.
And speaking of diagnosis, you don’t need to have a diagnosed GI condition to benefit from Oshi Health’s virtual, whole-person GI care.
Read on to learn how we can help you get to the bottom of what’s causing your symptoms and on the path to relief.
Unexplained GI symptoms
If something’s out-of-whack with your digestive system, you might be experiencing gastrointestinal symptoms like:
- Bloating
- Excess gas
- Diarrhea
- Constipation
- Abdominal pain
- Heartburn
- Acid reflux
- Difficulty swallowing
- Urgency with bowel movements
- Rectal bleeding or blood in your stool
- Nausea
- Vomiting
- Indigestion
You’re not alone in experiencing occasional or recurring stomach problems! According to a large-scale population-based study, nearly two-thirds of U.S. adults live with GI symptoms—and many of them are just like you, searching for answers.
At Oshi Health, our GI specialists, including GI providers, registered dietitians, and gut-brain specialists, work together to find and address your GI symptoms.
Causes for unexplained GI symptoms
Wondering what could be causing your GI symptoms?
Here are a few possible underlying gastrointestinal diseases that could cause symptoms like bloating, gas, diarrhea, constipation, and abdominal pain:
- Gastroesophageal reflux disease (GERD)
- Crohn’s disease
- Irritable bowel syndrome (IBS)
- Ulcerative colitis
- Small intestinal bacterial overgrowth (SIBO)
Here’s the thing: Digestive symptoms don’t always mean you have an underlying GI disease. Either way, we’re here to help you find relief from digestive distress.
GI condition risk factors
Just because you have a risk factor doesn’t mean you’re destined to develop a GI condition, but it can mean you’re more likely to develop one.
Plus, did you know that many GI conditions share similar risk factors? Here are a few common ones:
- Family history. Genetics plays a strong role in many gut health disorders, so if you have a close family member who lives with GI symptoms or has a diagnosed chronic gut health condition, you’re more likely to develop one yourself.
- Chronic condition. Having a chronic condition—another GI condition included—can up your risk of developing a GI disorder.
- Diet. A low-fiber diet can impact your gut health and lead to GI distress. There’s also a link between certain foods, like processed food, and poor digestive health.
- Lifestyle factors. Smoking, drinking alcohol, and lack of exercise can also increase your risk of developing a GI condition. Alcohol can even damage the lining of your digestive tract. Stress is another common shared risk factor between GI conditions—all thanks to the gut-brain connection.
- Medications. Some medications, like antibiotics, can influence your gut microbiome, making you more vulnerable to GI diseases.
Diagnosis of unexplained GI symptoms
At Oshi Health, our multidisciplinary GI specialists consider the whole you when working together to make a diagnosis, including your medical history, symptoms, and lifestyle.
An integrated team of GI specialists, working together for you
Our expert gastroenterologists, GI providers, registered dietitians, and gut-brain specialists are leaders in their fields, with advanced education and training in gastroenterology. Our comprehensive team approach is personalized to meet your unique needs and address the root cause of your symptoms.
Your provider will ask you questions about your symptoms, like when they typically occur, when they started, and whether certain foods or behaviors tend to make them worse.
They’ll also consider the following:
- Your diet and potential trigger foods
- Lifestyle habits
- Medications or supplements you’re taking or have already tried for your symptoms
- Stress and behavioral health
- Previous surgeries or medical procedures
- Your family history
And while you don’t need to have had previous testing to meet with an Oshi provider and benefit from our integrated GI care, your provider will review any previous testing you’ve gone through, if any.
While testing may be required to get to the bottom of your GI symptoms, we do our best to listen and avoid putting you through unnecessary and repeat testing—diagnosing and addressing symptoms based on our detailed knowledge of the whole you.
In-network with most major health plans
Unlike traditional healthcare providers, we don’t bill on a per visit basis. With insurance coverage, most Oshi Health patients get a year of unlimited care and only pay for four in-network specialist visits. For those four visits, copays and deductibles apply based on your plan benefit details.

Treatment
We take a comprehensive approach to treating GI health concerns, addressing not just your symptoms but also putting you on a path to lasting relief. Here’s an example of what care can look like for someone who came to Oshi with undiagnosed GI symptoms and needed a thoughtful, whole-person approach to treatment.

Here’s what our care entails:
1. Identifying triggers & making dietary and lifestyle adjustments
What does your typical diet look like? Do you have dietary triggers that seem to make your symptoms worse?
Our registered dietitians will help you identify your potential trigger foods and find ways to modify your diet without necessarily giving up the foods you love.
Depending on what triggers symptoms for you, management might also involve lifestyle changes, including:
- Adjusting meal timing or portion sizes
- Hydrating properly
- Improving sleep hygiene
- Regular physical activity
- Stress reduction (more on that below!)
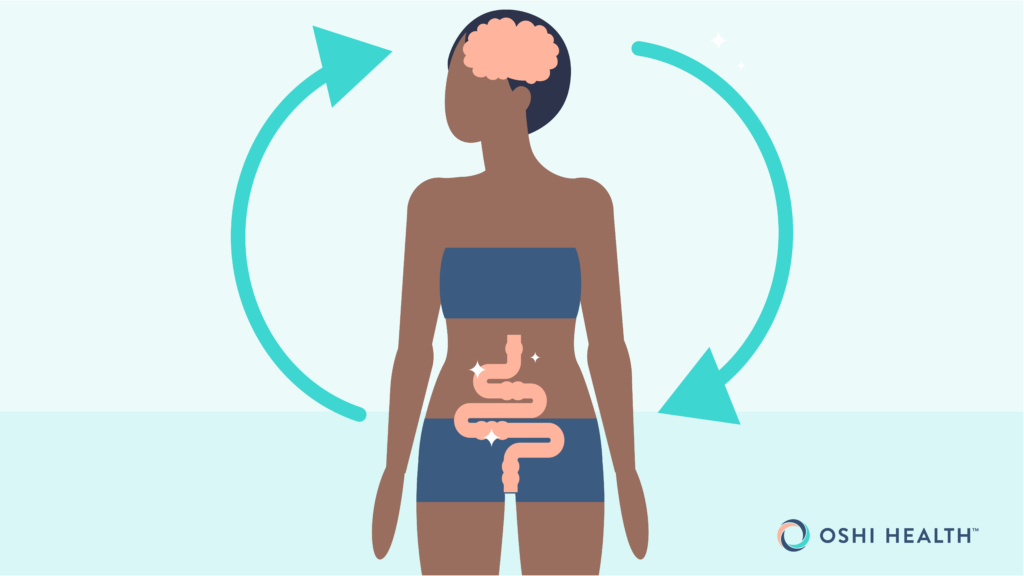
2. Working on the gut-brain connection
Did you know your brain and digestive system are in constant communication? It’s why you might feel nauseous when you experience heightened emotions like stress or excitement.
The close link between your GI system and mind can also play a role in GI conditions.
Our gut-brain specialists can help you identify potential stress-related triggers causing GI symptoms.
Gut-brain specialists are trained and licensed behavioral health professionals with specific experience treating GI concerns. Working alongside GI providers and registered dietitians, they can help you take control of your symptoms by providing you with the skills and tools to cope with distressing thoughts, feelings, and physical reactions that may be contributing to GI distress.
Some examples of common therapeutic gut-brain approaches include:
- Diaphragmatic breathing exercises
- Guided imagery and visualization
- Mindfulness-based therapies
- Cognitive behavioral therapy (CBT) for GI symptoms
- Gut-directed hypnotherapy (GDH)
Oshi Health gut-brain specialists are here to help you cope with digestive symptoms and validate your GI-related concerns—so you never feel alone in your journey to symptom relief.
3. Prescribing or recommending medications
Depending on your unique needs, medications may be a part of your personalized treatment plan.
However, medications are just one piece of the journey to symptom relief. Our whole-person approach to GI care looks at lifestyle factors such as diet and stress that may be contributing to symptom flares.
4. Whole person GI care
At Oshi Health, no two treatment plans are the same.
Our GI specialists work together to create a personalized treatment plan to address your GI discomfort. We consider the whole you—not just your symptoms. That means taking into account diet, lifestyle, and the gut-brain connection, ensuring you get the individualized care you need.
Already seeing a GI provider? We can provide support between visits and work with your existing gastroenterologist as an extension of your care.
- decrease in unnecessary (and expensive) procedures and tests
- of undiagnosed patients get a clear diagnosis within 3 months
- of patients report better quality of life, with less stress and anxiety, within 3 months
Source: Results of a clinical trial conducted in partnership with a national health plan
Oshi is your partner in digestive health
Feel like your digestive concerns are running your life? You’re not alone—and we’re here to help you find lasting relief.
Oshi Health GI providers, gut-brain specialists, and registered dietitians work together to address the root cause of your symptoms and find solutions that actually work for you.
Whether you’re dealing with chronic digestive issues or unpredictable symptom flare-ups, our GI specialists deliver:
✔ Personalized care plans tailored to your lifestyle
✔ Science-backed strategies to calm your gut
✔ Compassionate, whole-person care
✔ And so much more!
Ready to take control of your gut health?
Last medically reviewed July 2024