Ever find yourself asking, “why does my poop burn like acid?” Turns out, there are a lot of potential causes, ranging from eating spicy foods to gastrointestinal conditions like IBS and IBD. Here’s how to figure out what’s causing your burning bowel movements—and how to stop them.
Bowel movements are usually something we don’t think about too much—unless there’s something wrong. And if you sit down to go number two only to experience a burning or acidic sensation, it probably falls into the “something’s not quite right” category.
Burning bowel movements don’t have one easy-to-identify cause that applies to all situations. When it’s a one-hit-wonder, things like an extra spicy meal or using scented toilet paper may be to blame. If recurring, acidic poop may be related to a gastrointestinal disease, a medication, or another medical condition. Ahead, we’ll help you decipher what’s causing that burning sensation and offer ways to relieve it.
Fast answers: Top reasons it burns
Answering the question “Why does my butt burn when I poop?” sometimes feels like a whodunit novel. There’s a wide cast of suspects (aka possible causes), and without a diagnosis from a gastrointestinal (GI) provider, it can be impossible to get to the bottom of the mystery.
If burning when pooping is a passing sensation, meaning it doesn’t happen for weeks on end, it may be due to something you ate or drank. Spicy foods, alcohol, caffeine, and some sugary beverages may cause this sensation. An external irritant, like a scented soap or dyed toilet paper, may cause a burning or acidic sensation as well.
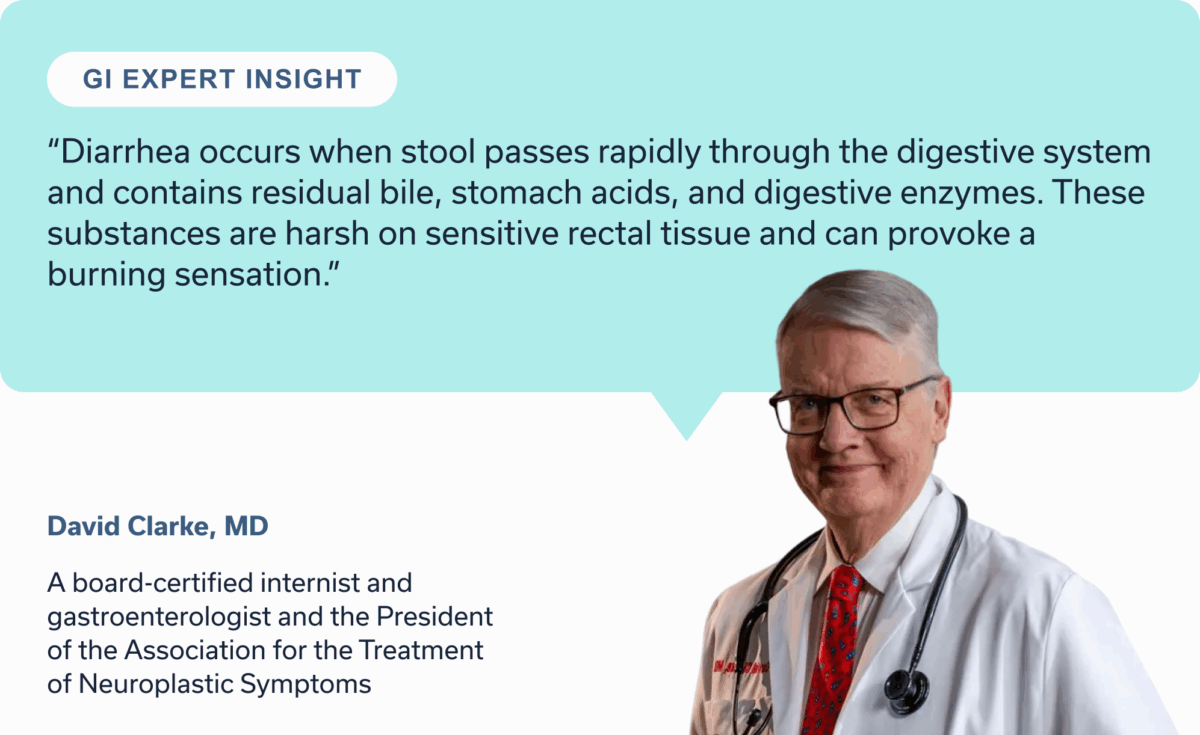
Two other common culprits are diarrhea and constipation, either of which can be temporary or long lasting. “One of the most frequent reasons is diarrhea, which occurs when stool passes rapidly through the digestive system and contains residual bile, stomach acids, and digestive enzymes,” says David Clarke, MD, a board-certified internist and gastroenterologist and the President of the Association for the Treatment of Neuroplastic Symptoms, “These substances are harsh on sensitive rectal tissue and can provoke a burning sensation when expelled.”
Constipation, defined as fewer than three bowel movements a week, can also result in burning bowel movements. Alongside making it harder to pass stool, constipation leads to hard and dry stool, which can be accompanied by a painful, sometimes burning sensation when it finally leaves the body, especially when associated with a fissure.
Common causes
If burning poop is a constant week after week, there’s probably an underlying medical cause. Sometimes that is diarrhea or constipation, though these can also be symptoms of another underlying condition.
Anal fissures
Small tears in the lining of the anus, referred to as anal fissures, can develop from various causes, including but not limited to: constipation, STIs, inflammatory bowel disease, and anal intercourse. These fissures cause painful bowel movements since the stool irritates the fissure.
Hemorrhoids
Hemorrhoids occur when the veins in the anus and lower rectum become swollen. These can cause anal itching or pain, especially when sitting or when pooping. Strained or painful bowel movements also increase the risk of hemorrhoids, meaning burning poop or hemorrhoids are a chicken and egg situation—it’s difficult to determine which causes which.
Irritable bowel syndrome (IBS)
Burning or painful poop can be a sign of many GI diseases, including IBS. This chronic condition leads to uncomfortable abdominal symptoms, which may include constipation or diarrhea, both of which may lead to burning bowel movements.
Inflammatory bowel disease (IBD) and proctitis
IBD is an umbrella term for Crohn’s disease and ulcerative colitis, two conditions that cause inflammation in the intestines. One of IBD’s symptoms is proctitis, inflammation in the lining of the rectum, which may contribute to pain when pooping.
While IBD-related proctitis is the most common type, it isn’t the only kind. Proctitis may also be caused by some bowel surgeries, certain infections, food poisoning, and radiation therapy in the pelvic region or lower abdomen.
Other medical conditions
“Less commonly, the sensation may stem from infections, sexually transmitted diseases, or even precancerous or cancerous growths in the digestive tract,” says Dr. Clarke.
Another potential cause is perianal eczema, which is when the skin near the anus is irritated, red, or swollen. Perianal eczema stems from a mix of genetic and environmental factors.
A burning sensation may also be from contact dermatitis, a type of eczema caused by an interaction with an irritating chemical or other substance. In the case of the anus, this could be an irritating soap or scented toilet paper, for example.
Food, medications, and supplements
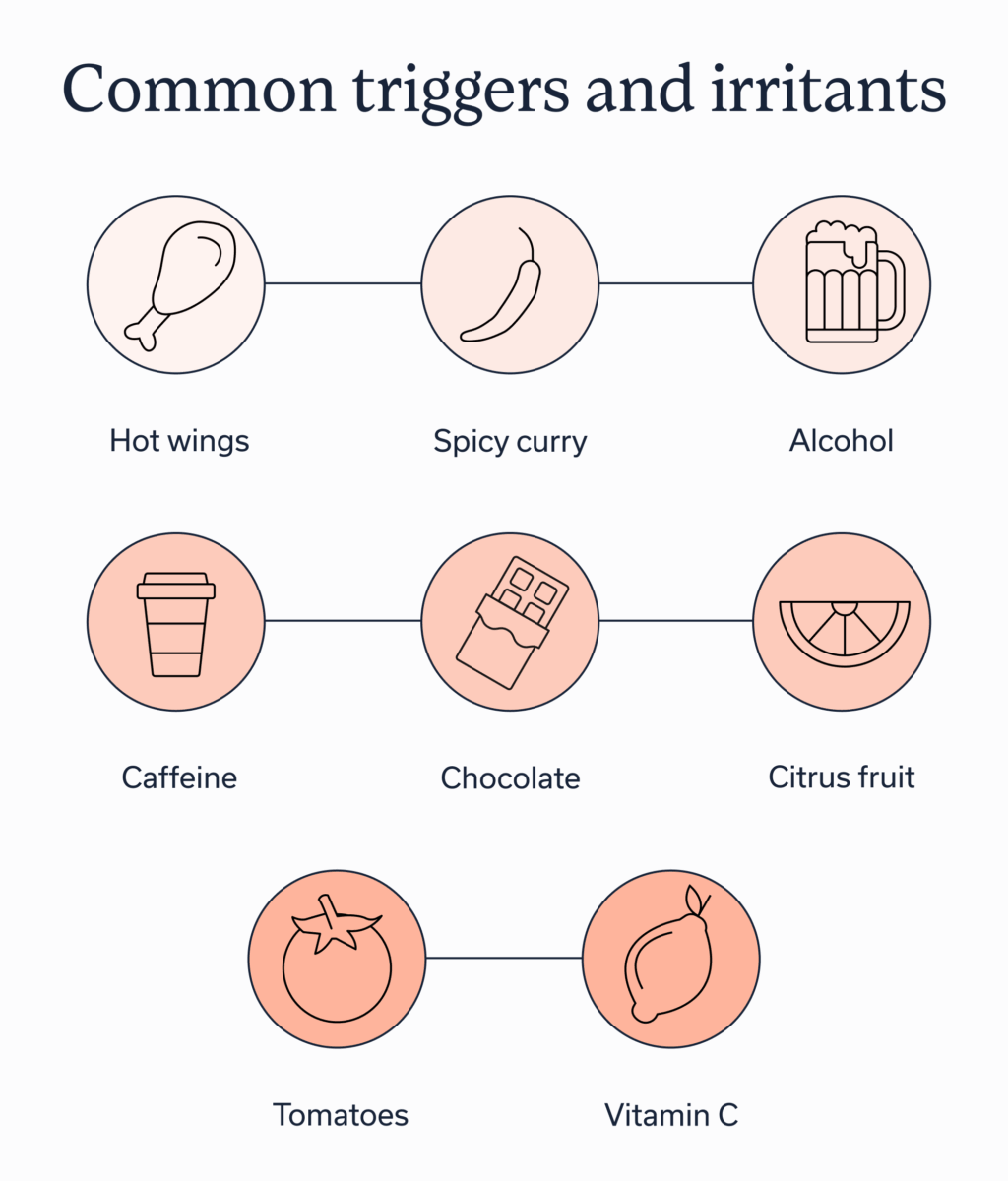
“Consumption of spicy foods containing capsaicin can irritate tissues during excretion,” says Dr. Clarke. But those hot wings or a spicy curry aren’t the only substance that causes irritation when leaving the body. Alcohol, caffeine, chocolate, citrus fruit, tomatoes, and vitamin C supplements are also common culprits.
Medications and supplements may also disrupt bowel movements, sometimes leading to constipation or diarrhea and, in a roundabout way, to burning poop. If we listed all the medications and supplements with constipation or diarrhea as a side effect, we’d be here for quite a while. Instead, here are some of the most common:
Self-care that helps most cases
Burning poop isn’t fun, but most cases improve with a few self-care measures:
- After bowel movements, pat dry with toilet paper instead of rubbing
- Avoid spicy foods, caffeine, and alcohol
- Don’t use fragmented or dyed soaps around the anus
- Rinse the anus after bowel movements. Ideally this should be gentle and with water, not with wipes, soaps, or scrubbing.
- Take a warm bath to soothe discomfort
- Wear loose clothing and cotton underwear to not irritate the area further
In some cases, you may want to consider over-the-counter creams, gels, or ointments that help with anal irritation or pain. Just make sure to read the instructions thoroughly beforehand and to double check to ensure that none you use interfere with any medications you’re taking. If in doubt about which OTC product might help, contact a healthcare provider.
When to seek care
If you try the aforementioned self-care strategies and they don’t work, or the burning poop sensation keeps returning, it’s time to visit a healthcare provider. Dr. Clarke also advises seeing a healthcare provider if there has been unprotected anal intercourse, regardless of if self-care helps, to assess the risk of STIs.
Ideally, that healthcare provider would be a GI provider, though it may make sense to see your primary care provider first if you need a referral to a specialist for insurance purposes.
Diagnosis: What a clinician may do
Burning poop isn’t an official diagnosis, and as we’ve established, there’s a laundry list of potential causes. That’s why it’s important to get a diagnosis from a GI provider. To diagnose the cause, they’ll probably look at your medical history, diet, and any medications you take. A GI provider will also consider factors like if you’ve traveled abroad lately, since some countries present a higher risk of certain infections that can affect GI health, or if burning poop is tied to any specific triggers.
In the same appointment, they’ll often conduct an anorectal exam to assess for irritation or other visible symptoms. Depending on your situation, they may also order blood tests or stool tests.
If they suspect certain causes, such as IBD or cancerous cells, they may order an endoscopy, where a camera and light are inserted into the body to look for any abnormalities. There are various types of endoscopies targeting different parts of the digestive tract, and a GI provider will recommend the right one in your situation.
Treatment options by cause
Once you have an official diagnosis, a GI provider can create a customized treatment plan. Often, this plan entails steps to treat diarrhea or constipation, as well as any underlying medical conditions.
How to stop burning from constipation
Treating constipation often boils down to looking at diet and lifestyle. Regular physical activity paired with adequate hydration and a diet high in fiber can help keep things moving. Fiber is especially important since it passes through the digestive system without being absorbed into the bloodstream, cleaning out the digestive tract along the way. This substance is found in a variety of plant-based foods, like fruits, vegetables, whole grains, and nuts.
It’s recommended to get 21 to 38 grams of fiber per day, but most Americans only eat 16 grams. Easy swaps to get more fiber include eating whole grain pasta instead of white pasta, switching white rice for brown rice, and adding one more veggie or fruit to your plate each day.
But before you go all out on fiber, there are a few things to keep in mind. Like a romantic relationship, it’s healthier to take it slow. To avoid bloating, abdominal pain, or gas, introduce fiber gradually instead of going all in. Those with GI conditions like IBS or IBD also respond differently to fiber and should work with a GI provider to safely adjust their fiber intake.
Last but certainly not least, bowel retraining can help with constipation. This often looks like:
- Setting a daily time to try and go number two, ideally 20-40 minutes after a meal
- Adapting a better toilet position
- Trying GI-focused therapy to address any emotional reasons for constipation
How to stop burning from diarrhea
Other foods and drinks to avoid include chocolate, sources of caffeine, dairy products, and fried foods.
Another thing to look at is your stress levels. Stress, anxiety, and other negative emotions can cause diarrhea or make it worse, thanks to the gut-brain connection. If you’ve experienced butterflies on a first day or before a big presentation at work, you’ve already experienced this connection firsthand. When there’s distress in the brain, it can cause disruptions to the GI tract, sometimes manifesting as the runs.
If the gut-brain connection is contributing to recurring diarrhea, working with a gut-brain specialist can help. For quick relief, at-home strategies to reduce stress, like meditation or breathwork, may do the trick.
Depending on the cause of diarrhea, medications may also help. This could include anti-diarrheal medications or medications for an underlying condition, such as an antibiotic for a viral infection. If you opt for anti-diarrheal medications, keep in mind that they help in the short term, but you shouldn’t rely on them for the long haul. What does lead to lasting relief? Dietary changes, GI-focused therapy, and stress management.
Treating underlying conditions
The above treatments for constipation and diarrhea are safe and effective, but they aren’t always enough on their own. To say goodbye to that burning poop sensation, you may need to treat any underlying causes like those we’ve discussed above—IBD, constipation, etc. A GI provider can diagnose these and create a customized treatment plan.
Working with Oshi Health
No matter what’s causing your bowel movements to burn, a GI provider can help pinpoint the exact cause, help you map out triggers, and create a personalized treatment plan. For the best results, work with a GI provider who understands that gut health is important and that it’s connected to the brain. That provider should also help you implement lifestyle changes that can help alleviate painful bowel movements, such as GI-focused therapy or implementing dietary changes.
Oshi Health checks all these boxes. Our patients work with a team of GI providers, GI registered dietitians, and gut-brain specialists who tackle burning poop and any other GI symptoms. Our team can provide a diagnosis and tailor a treatment plan so it addresses underlying causes and works with your lifestyle.
Key takeaways
- Burning poop sensation is quite common. When it’s temporary, it may be caused by spicy food, caffeine, alcohol, or an environmental irritant, like scented toilet paper. If ongoing, a condition like diarrhea, constipation, IBD, IBS, anal fissures, or hemorrhoids may be present.
- Discovering the cause of ongoing burning bowel movements isn’t a DIY project. Instead, work with a GI provider who can take into account your symptoms, conduct a physical examination, and order any necessary tests.
- From there, your GI provider can create a tailored treatment plan. This may include changes to diet and lifestyle, GI-focused therapy, bowel retraining, and treatment for any underlying medical conditions.
Frequently asked questions (FAQs)
-
Acidic poop can indicate a variety of things. If it happens once or twice, it may be due to something you ate or drank, such as a spicy curry or a caffeinated beverage, or from an environmental irritant, like a scented or dyed soap. When it lasts for weeks on end, it could stem from constipation, diarrhea, IBS, IBD, hemorrhoids, anal fissures, or other medical conditions. Some medications may also cause this symptom. A GI provider can diagnose the exact reason for acidic poop.
-
To get rid of acidic poop, start with self-care steps, such as gently washing the anus with water after a bowel movement, patting the area dry with toilet paper instead of rubbing it, and taking a soothing, warm bath. You may also want to avoid irritants like spicy food, scented or dyed toilet paper, and alcohol. If symptoms persist after using these self-care strategies, see a GI provider.
-
If stool feels like acid, it typically means something is irritating the anus or rectum. Many things may cause this irritation, ranging from spicy foods to some medications to diarrhea, constipation, and other underlying medical conditions.
-
Spicy foods containing capsaicin are one of the most common causes of acidic poop, but they aren’t the only food that may be to blame. Citrus fruits, alcohol, caffeine, and tomatoes may also lead to irritation or pain during bowel movements.
Oshi is your partner in digestive health
Feel like your digestive concerns are running your life? You’re not alone—and we’re here to help you find lasting relief.
Oshi Health GI providers, gut-brain specialists, and registered dietitians work together to address your symptoms and find solutions that actually work for you.
Whether you’re dealing with chronic digestive issues or unpredictable symptom flare-ups, our GI specialists deliver:
✔ Personalized care plans tailored to your lifestyle
✔ Science-backed strategies to calm your gut
✔ Compassionate, whole-person care
✔ And so much more!
Ready to take control of your gut health?