“Stress belly” is a slang term that refers to increase in abdominal fat or gastrointestinal issues, such as bloating or distention, resulting from chronic stress. Because the gut and brain are closely linked, chronic stress can interfere with their communication and lead to digestive symptoms.
“Stress belly,” at its root, is a term for when we don’t feel quite like ourselves, whether experiencing digestive issues or noticing changes in body fat distribution. If you’re noticing an increase in fat around your abdominal area, even though your lifestyle hasn’t changed, you may have a case of “stress belly.” Likewise, if you’re experiencing bloating and distention or other gastrointestinal (GI) issues, stress may be a culprit.
As an example, my friend Amelia says that when she was going through her high-stress divorce several years ago, she noticed an increase in fat accumulation, strictly around her abdomen, despite keeping up her usual habits and lifestyle. Her symptoms eventually resolved once she’d settled into her new and happier normal.
And, for myself, when I was on a book deadline a few years ago, I noticed an uptick in bloating and gastrointestinal (GI) discomfort in the last few weeks before my manuscript was due. The symptoms calmed not long after I hit the “send” button, getting that sucker off to my editor.
What exactly is stress belly?
“‘Stress belly’ is a term often used to describe a condition of both brain-gut disruption (e.g., abdominal discomfort and bloating) and physiological changes (e.g., abdominal fat),” says Steven Feinstein, PhD, a Clinical Health Psychologist and Gut-Brain Specialist at Oshi Health. “Abdominal fat is often due to hormonal changes, while discomfort and bloating are mainly a function of disruption along the brain-gut axis of the nervous system.”
“Stress belly”—also called “hormonal belly” and “cortisol belly”—are not medical terms. They’re used colloquially to describe two distinct, but often overlapping, issues:
- Fat accumulation from stress
- GI issues, such as bloating and distention from stress
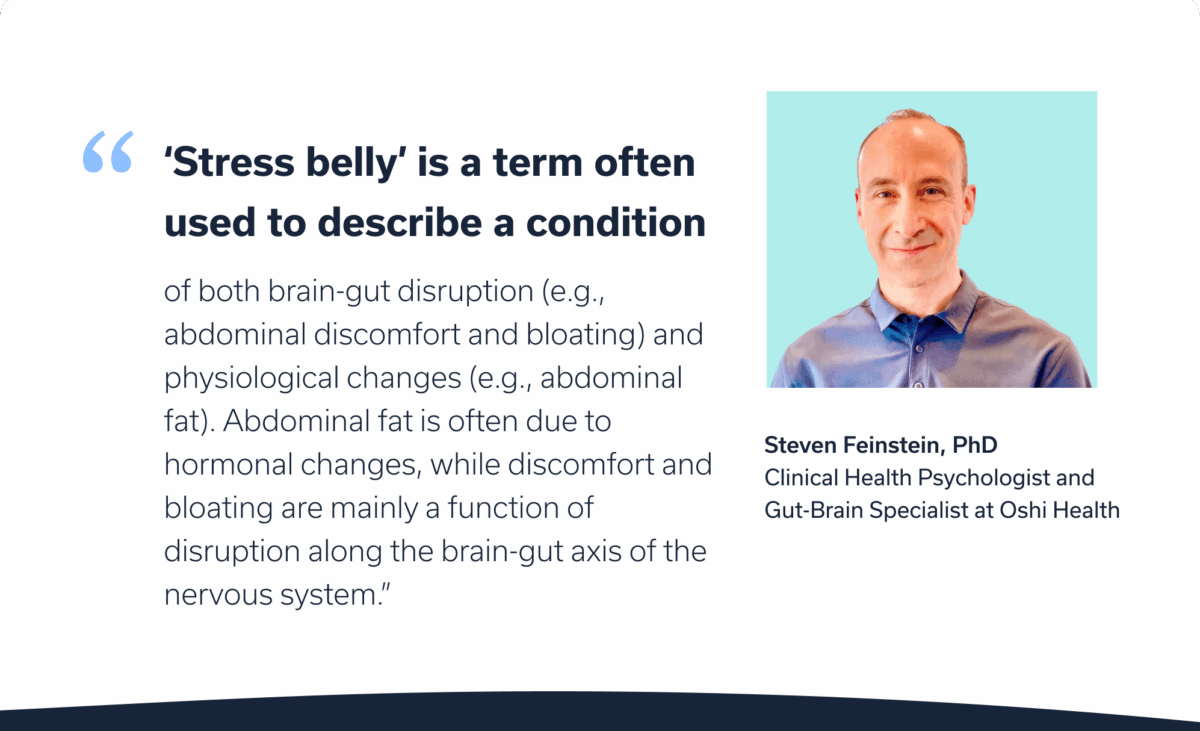
Stress belly can be frustrating, because you may be noticing changes in the amount of fat around your abdomen, even if your habits or weight haven’t changed. “Stress belly is not about willpower,” Dr. Feinstein says. “It comes about from real physiological changes, often triggered by the nervous system under stress.”
But you’re not at the mercy of a stressed-out belly. In this article, we explore what stress belly is, why it occurs, and how you can address it so you can feel better.
What are the symptoms of stress belly?
You may be wondering, “What does stress belly look like?” It can show up differently from person to person. Some people may only notice a change in their body shape, while others may experience GI issues.
Fat accumulation and importance
One note on body fat (or (adipose tissue), which this article discusses in depth: We need it for our bodies to function properly. It supports our bodies’ hormonal processes, cellular functions, and vitamin absorption. It also protects our internal organs and regulates body temperature.
But you may (understandably) feel frustrated when your body changes unexpectedly. So let’s dig into this complicated topic.
We have three key types of fat:
- Essential fat. Essential fat is exactly what it sounds like. It’s the fat we need to keep us healthy because it regulates hormones and body temperature. It’s stored in various tissues throughout the body, including the brain.
- Subcutaneous fat. Subcutaneous fat is the type that’s just under the skin. It’s stored all over the body, but you might notice it more in your arms, thighs, and abdominal area. A certain amount of subcutaneous fat is also necessary for health.
- Visceral fat. Visceral fat is the kind that lines our internal organs. Some is necessary for organ protection, but too much is dangerous because it contributes to negative health issues, such as heart disease, diabetes, and stroke.
Belly fat generally contains all three of these fat categories, with subcutaneous as the most visible, or the type you can pinch, and visceral lying deep inside the belly. Visceral fat can push the belly out, even if the number on the scale hasn’t changed much. Doctors often measure visceral fat by checking waist circumference and waist-to-hip ratio or through dual-energy X-ray absorptiometry (DEXA) scan. When it comes to stress belly, an increase in visceral fat is often the main culprit—driven by chronic stress and hormonal changes like elevated cortisol. We’ll discuss this in more depth later in the article.
GI issues from stress
Stress might also cause you to experience GI issues that affect your abdominal area. Bloating and distention can result from glitches along the gut-brain axis.
“Stress causes a change in the nervous system,” Feinstein says. “Nervous system change disrupts the messages between the brain and gut. A disruption in these signals results in the abdominal discomfort and bloating often characteristic of “stress belly.”
Why stress causes abdominal fat and digestive issues
Now let’s dig into why stress can have an impact on your abdominal area.
Why stress drives abdominal fat
Cortisol, the stress hormone, is a steroid that can contribute to abdominal fat accumulation, especially visceral fat. You might have a high cortisol level from chronic stress, lifestyle factors, exposure to environmental toxins, or even rare adrenal or pituitary gland tumors. Dysregulated cortisol is often a result of chronic stress rather than acute stress.
Acute stress: Our built-in survival mechanisms (aka fight-or-flight response controlled by our sympathetic nervous system) activates when an acute (immediate) stressor pops up, like if you hear an unusual noise in your house in the middle of the night.
Your bloodstream floods with adrenaline and glucose (blood sugar) so you can act if need be. But when you realize the noise was just your cat having a personal party in your living room, your body quickly calms again so you can go back to sleep.
Chronic stress: Chronic stress is ongoing and can result from more serious stressors (or an accumulation of smaller stressors), including work obligations, relationship issues, family responsibilities, financial hiccups, yadda-yadda.
You can also experience chronic stress from the ongoing psychological distress from past traumas.
Chronic stress involves your fight-or-flight response, but it takes things a step further. Instead of calming after the initial flood of adrenaline, your stress response takes things to the next level and floods your body with cortisol to help you continue to respond to the “threat.” High or dysregulated cortisol encourages your body to store visceral fat.
Additionally, elevated glucose and insulin levels from dysregulated cortisol can cause fat storage.
Why stress drives digestive issues
Digestive issues can also ensue from stress. To explore this, we have to outline the different branches of the autonomic nervous system (ANS), which controls your involuntary bodily processes, including your heart rate, body temperature, blood pressure, and digestion. Your ANS has three divisions.
3 ANS divisions:
- Sympathetic nervous system (SNS). Controls your “fight-or-flight” response, aka your stress response.
- Parasympathetic nervous system (PNS). Controls your “rest-and digest” response, aka your calm response.
- Enteric nervous system (ENS). Controls your GI tract.
We’ve already explored your fight-or-flight response in relation to acute and chronic stress. Your rest-and-digest, or calm, response works somewhat in opposition to your fight-or-flight, and vice versa. If we think back to our example of the middle-of-the-night noise, once you realize it was your naughty cat rather than an intruder, you return to your calmer state and can go back to sleep.
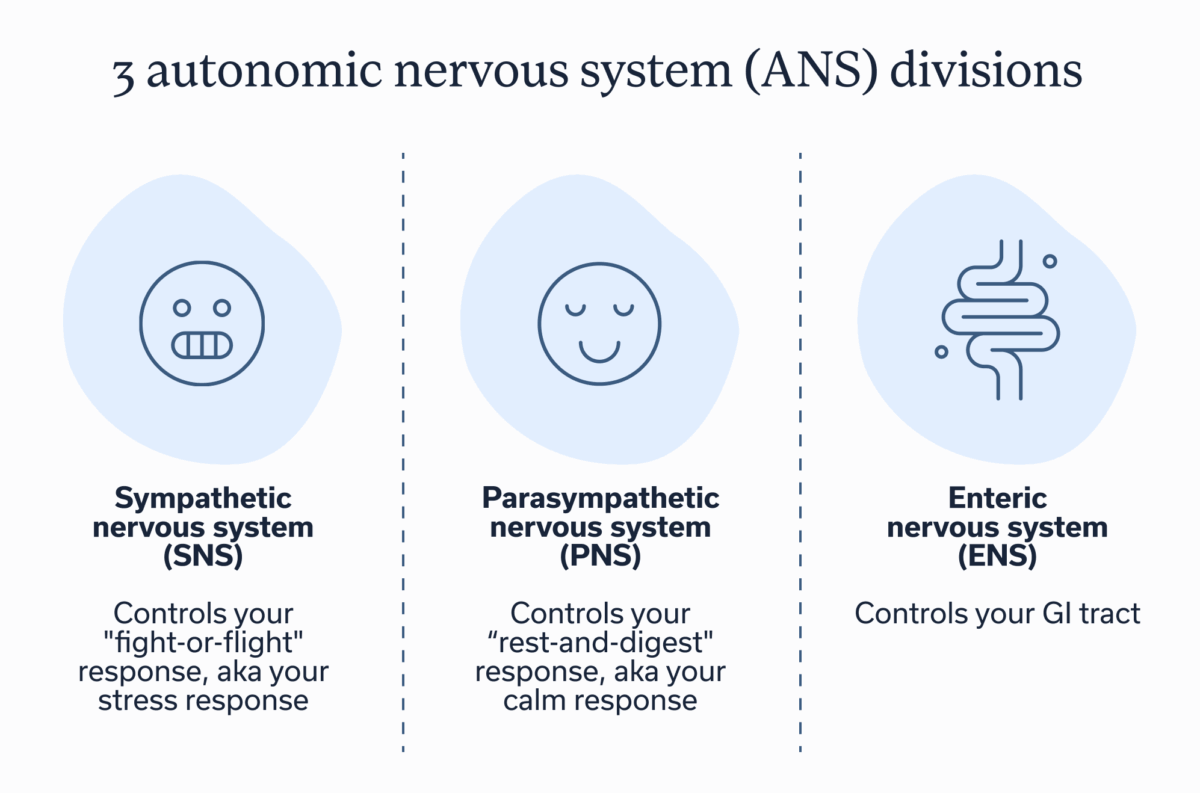
Your ENS is a neuronal network within the walls of your GI tract. It’s in charge of digestive functions, such as gastric secretions, motility (the movement of food and waste), etc. It works independently and in collaboration with the SNS and PNS. But disruptions or miscommunication can ensue.
“A significant difference is that a more acute short-term stressor creates disruption that generally returns to normal state not long after the stress is gone,” Dr. Feinstein says. “However, chronic stress creates longer term disruption to gut-brain signaling, which, over time, creates lasting changes in the gut. These changes tend to persist, along with associated symptoms, even after the period of chronic stress ends.”
How to address stress belly: practical approaches
Now that you have a better understanding of stress belly and its causes, you may be wondering how to resolve it or ease symptoms.
Reduce stress
You’ve probably guessed that stress and anxiety reduction is the heart of resolving stress belly, whether you’re concerned about visceral fat gain or want to find relief from frustrating GI symptoms.
Of course that’s easier said than done sometimes, and once gut-brain disruptions have been ongoing, they can be hard to resolve on your own. Instead, you may need the help of a knowledgeable provider.
“Brain-gut behavioral interventions (BGBT) can reduce stress belly by targeting symptoms (e.g., abdominal discomfort and bloating),” Dr. Feinstein says. “Interventions take the form of behavioral change (e.g., diaphragmatic breathing), cognitive strategies focused on GI symptoms, and integrative GI treatments such as gut-directed hypnotherapy. These are just some of the evidence-based interventions our gut-brain specialists provide to our members at Oshi.”
Prioritize sleep
Getting about seven hours of good quality sleep is also crucial for mitigating stress and regulating cortisol levels. If you’re struggling with sleep disruptions, consider ways to minimize noise and light pollution and carve out time before bed to engage in a regular sleep-prep routine that allows your body time to settle in.

Adjust diet as necessary
Changing your diet may also help improve symptoms, but what works for one person may not work for the next. That’s why consulting with a GI registered dietitian may be of benefit.
They can help you assess any foods that tend to trigger GI symptoms and perhaps help you find alternatives that fit your taste and cultural preferences.
Additionally, sticking to an anti-inflammatory diet may help. Stress and dysregulated cortisol can drive inflammatory processes, but certain dietary approaches, such as the Mediterranean diet, can counteract some inflammation, perhaps helping to ease symptoms of stress belly.
Engage in physical activity
Exercise helps reduce stress, and therefore cortisol. It’s also a strategy for helping you to become more resilient to stress in the long run. Research shows that highly active people have blunted cortisol responses to psychological stress.
This may sound odd, since exercise itself is a stressor and it activates your fight-or-flight response. Think about it: Your body temp rises, your heart rate increases, your heart works harder and elevates your blood pressure, etc. But then you finish that run or high-intensity-interval-training workout, and you return to your rest-and-digest state. Your heart rate slows, your body cools, and your blood pressure chills out.
This process teaches your body to adapt to acute stressors; it becomes better at toggling between sympathetic and parasympathetic nervous system activation.
Plus, when you exercise, you tend to burn visceral fat first, which can help resolve a stress belly from dysregulated cortisol.
Focus on gut microbiome health
Your gut microbiome, the community of bacteria and fungi in the gut, can also play a role in stress. Brain signals after stress can alter your gut microbiome, which then could cause GI symptoms and further exacerbate stress.
The relationship that the brain and gut have with each other is complicated. But improving the gut microbiome may be a strategy to help reduce stress or GI symptoms related to stress. Strategies might include taking a provider-recommended probiotic or eating prebiotic- or probiotic-rich foods.
Key takeaways
- “Stress belly” refers to either cortisol causing abdominal fat gain or GI issues that can ensue because of stress’s impact on gut-brain communication.
- The two main contributors to stress belly include: 1) disrupted gut-brain communication, which influences digestion and can lead to GI symptoms; and 2) elevated cortisol levels, which contribute to the accumulation of visceral fat.
- Ways to address stress belly involve using behavioral therapies to help you learn to manage your body’s stress response and minimize the disruption of gut-brain communication.
- A GI psychologist, such as those at Oshi Health, can help you improve gut-brain communication and ease your symptoms.
FAQ
-
“Stress belly” is a colloquial term, rather than a clinical one, and it describes two potential issues that can occur alone or together: chronic stress causing increased visceral fat storage or stress causing GI symptoms, such as bloating and distention because of disrupted communication between the gut and brain. To resolve a stress belly, you will need to understand the root cause. If it’s chronic stress, then stress mitigation techniques can help. If it’s miscommunication along the gut-brain axis, you may need to work with a knowledgeable clinician who can help you restore optimal gut-brain communication.
-
Stress belly can feel heavy, painful, bloated, distended, constipated, and more.
-
“Cortisol belly” is a nonclinical term used to describe how elevated cortisol from chronic stress can contribute to the accumulation of visceral fat, the type of fat that surrounds your organs. It can push the belly out, regardless of someone’s weight or body composition. The term also describes how stress can contribute to GI symptoms. Though many GI symptoms are invisible, bloating and distention are two you might notice when putting on clothing or looking in the mirror.
-
When you’re chronically stressed, weight management can be tricky. This is because elevated cortisol from ongoing stress can drive the storage of visceral fat, which is generally located deep within your abdominal area and can push the belly out. The first step to managing weight when stressed is to reduce stress. But increasing physical activity, eating an anti-inflammatory diet, and getting optimal sleep, are also important.
Oshi is your partner in digestive health
Feel like your digestive concerns are running your life? You’re not alone—and we’re here to help you find lasting relief.
Oshi Health GI providers, gut-brain specialists, and registered dietitians work together to address your symptoms and find solutions that actually work for you.
Whether you’re dealing with chronic digestive issues or unpredictable symptom flare-ups, our GI specialists deliver:
✔ Personalized care plans tailored to your lifestyle
✔ Science-backed strategies to calm your gut
✔ Compassionate, whole-person care
✔ And so much more!
Ready to take control of your gut health?