Acid reflux often manifests as a burning sensation in your chest, possibly accompanied by other symptoms, like regurgitation or a chronic cough. At first glance, this sounds undesirable but not life-threatening. But can acid reflux actually be dangerous? While acid reflux once in a while may not be of concern, repeat occurrences may lead to more serious side effects and complications, especially if left untreated.
Almost all of us get heartburn from time to time. Maybe you drank a lemonade too fast or overdid it on some amazing hot wings, experienced heartburn afterwards, and eased it up with some Tums without a problem. If acid reflux happens to you once or twice a year, it probably isn’t dangerous.
When acid reflux shows up more than twice a week, however, it’s a different story—and even a different condition, categorized as gastroesophageal reflux disease (GERD). GERD is a chronic issue that can be accompanied by some potentially serious complications. Even mild and uncomplicated cases of GERD are more than “just heartburn.” It can influence your physical health, mental wellbeing, and quality of life. Fortunately, there are tried-and-true ways to treat GERD, stave off acid reflux, and stay out of the danger zone.
But first, let’s back up: How does acid reflux work, whether you have GERD or just intermittent heartburn?
What is acid reflux?
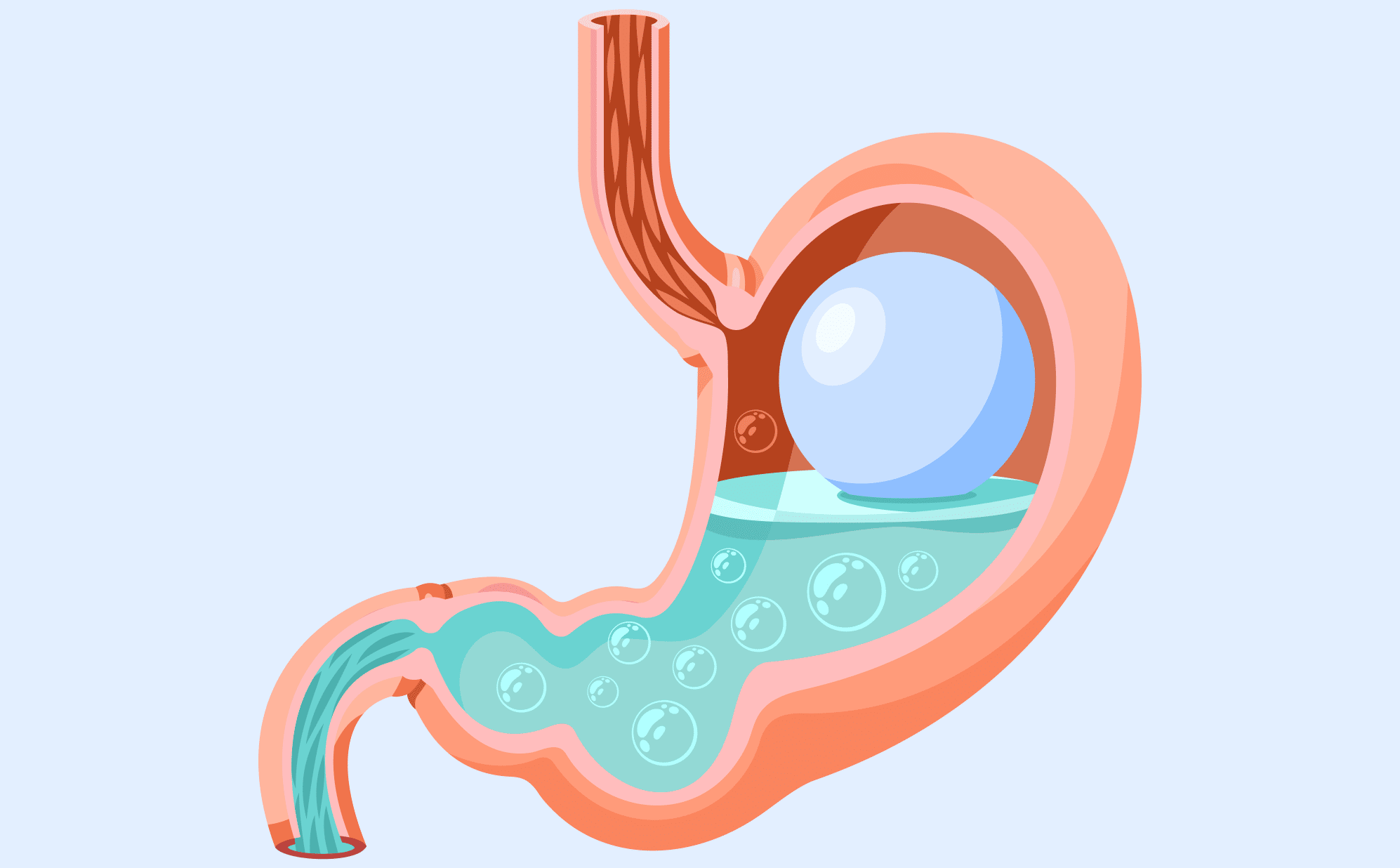
Acid reflux occurs when your stomach acid flows back up your digestive system. If that sounds unusual and unpleasant, it’s because this is not how your digestive system is designed to work. When you eat, food travels from your mouth via the esophagus, a pipe found behind your heart, to your stomach. At the end of your esophagus is your lower esophageal sphincter (LES), a ring of muscles that controls the flow of food between your esophagus and stomach.
The LES lets food flow into your stomach, closing up afterwards, so neither food nor stomach acid can travel back into the esophagus. But if your LES is weak or inappropriately relaxed, food and acid can end up flowing both ways, like a car driving the wrong way on a one-way road. And like with that car, havoc may ensue.
Common symptoms of acid reflux
While heartburn, that fiery sensation in your esophagus, is the most common symptom of acid reflux, it isn’t the only one. The second most common is regurgitation, which is when stomach content travels to your throat or mouth, and there’s a lingering aftertaste of stomach acid or food.
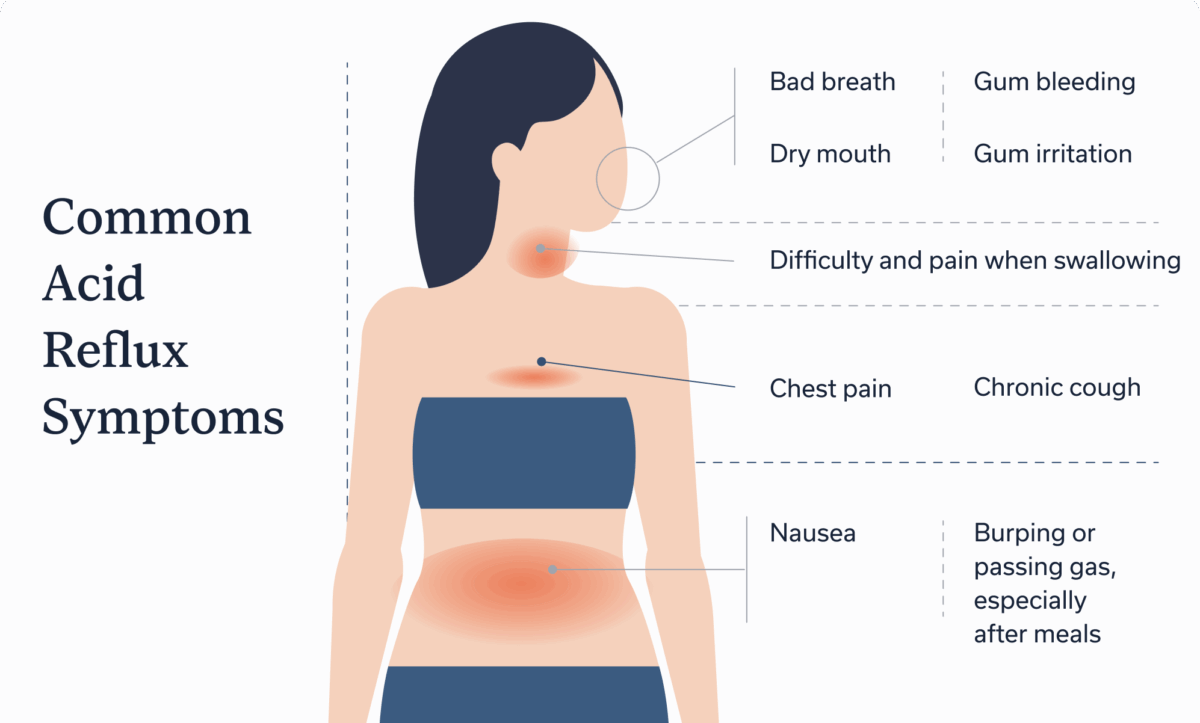
Other symptoms and signs of acid reflux include:
- Bad breath
- Bloating
- Burping or passing gas, especially after meals
- Chest pain
- Chronic cough
- Difficulty swallowing
- Gum bleeding or irritation
- Nausea
- Pain when swallowing
Untreated GERD sometimes leads to more serious complications, like loss of appetite and persistent vomiting. In severe cases, GERD may lead to blood in your digestive tract, evident by either bloody stool or blood in your vomit. If you experience either of these, seek immediate care.
Acid reflux causes and risk factors
About 20% of Americans suffer from GERD, and most people have experienced acid reflux at least once in their lifetime. There are certain factors that can increase your risk of GERD:
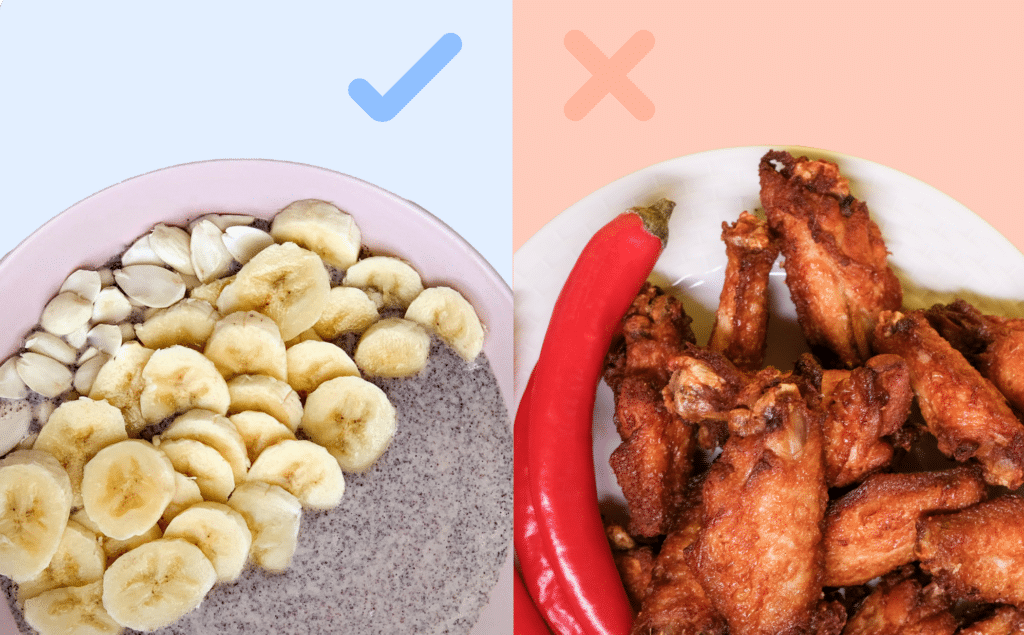
- Above average intake of sweets, acidic foods, or fried foods
- Bariatric surgery
- Certain medications
- Depression
- Inactive lifestyle
- Heavy drinking
- High amount of belly fat
- Hiatal hernia, when the stomach protrudes up into the chest
- Low fiber intake
- Obesity
- Pregnancy
- Smoking
At first glance, these factors may seem unrelated to each other, or to acid reflux. However, any of these risk factors increase the likelihood of your LES becoming weaker or relaxed, allowing stomach acid and food to leak back up your digestive tract.
Where these risk factors differ, at least in relation to acid reflux, is that some cause a temporary weakening of the LES and others a more permanent relaxation or structural changes. A hiatal hernia, for example, causes structural problems that may lead to GERD, whereas eating more sweets than usual at a birthday party or overdoing it on Champagne at a wedding may only cause temporary acid reflux.
When acid reflux becomes dangerous
Most cases of acid reflux resolve without treatment, and isolated incidents of acid reflux often fall into the “annoying” category, not the danger zone. But while acid reflux’s most common symptoms aren’t life-threatening, it’s important to remember that stomach acid is powerful. Its job is to break down food. And when stomach acid enters your esophagus, throat, or mouth time and time again (as in GERD), it could potentially lead to:
- Barrett’s esophagus: A condition that causes the line of your esophagus to change. It doesn’t cause additional symptoms, but it can increase your risk of esophageal cancer.
- Breathing issues: When your stomach content flows back up your digestive tract, there’s a chance it will enter your lungs, and can trigger or worsen asthma or asthma-like symptoms as well as increase your risk of respiratory infections.
- Dental complications: With GERD, it’s possible for stomach acid to enter your mouth, causing damage to your teeth and gums.
- Esophagitis: This condition occurs when your esophagus lining becomes damaged, irritated, or inflamed.
- Esophageal stricture: A condition where inflammation causes a narrowing of your esophagus, making it difficult to eat or drink.
- Esophageal cancer: GERD, especially if it develops into Barrett’s esophagus, can increase your risk of esophageal cancer. This doesn’t mean everyone with GERD or Barrett’s esophagus will get this type of cancer, just that the risk is higher than for the general population.
- Laryngopharyngeal reflux: When stomach acid travels into and causes damage to your throat and vocal cords.
- Severe upper gastrointestinal bleeding: If esophagitis remains untreated, it may cause GI bleeding, a condition that can be life threatening.
GERD can also decrease your overall quality of life, especially if it becomes severe. Dealing with GERD symptoms and complications can cause discomfort and inconvenience, as well as mental health impacts. A 2024 study demonstrated that GERD can directly increase someone’s risk of experiencing anxiety and depression. The study also stated that GERD, especially at nighttime, can make it difficult to sleep, meaning those with GERD are more likely to have sleep disorders.
Hidden or atypical symptoms to watch for
Let’s make one thing clear: Any symptoms of acid reflux or GERD that happen more than twice a week merit a visit to the doctor, ideally a gastroenterologist or other GI provider who can provide you with tailored, whole-person care.
That said, there are some symptoms that may indicate something is awry and one of the above complications may be present or developing. In these cases, you should seek care immediately. Atypical symptoms of GERD include:
- Bloody stool
- Difficulty swallowing
- Laryngitis or asthma-like symptoms
- Persistent cough or throat clearing
- Vomiting, especially with blood in vomit
Acid reflux treatment options
While GERD and acid reflux can be dangerous, they’re also treatable. When looking at how to treat acid reflux and GERD, there are three options to consider: medications, lifestyle adjustments, and surgery.
Acid reflux medicine
For more serious cases, a GI provider may recommend one of three prescription drugs that reduce the production of stomach acid:
- H2 blockers: Famotidine (Pepcid, Zantac), cimetidine (Tagamet), and nizatidine (Axid) are three popular H2 blockers.
- Proton pump inhibitors (PPIs): The most common drugs in this class are omeprazole, esomeprazole, and lansoprazole.
- Potassium-competitive acid blockers: Vonoprazan and tegoprazan both fall into this class.
While these prescriptions may be effective in the short term, 20-40% of those with GERD don’t respond to PPIs, the most common of the three. And whether over-the-counter or prescription, medications decrease symptoms but don’t address the direct cause of acid reflux: a weak or relaxed LES.
Lifestyle modifications
So if medication doesn’t address the actual cause, what does? For many, the answer is lifestyle modifications. By making dietary and lifestyle choices that help strengthen the LES, you reduce the risk of future GERD flare-ups. You can:
- Avoid trigger foods
- Work with a therapist and/or gut-brain specialist to decrease your anxiety and stress
- Exercise regularly
- Increase fiber intake
- Quit (or don’t start) smoking
- Sit or walk after meals; don’t lie down
- Stop eating two to three hours before bed
- Reduce or eliminate alcohol consumption
- Wear loose-fitting clothing
Treating acid reflux and GERD through lifestyle changes is an ongoing process. Many people with GERD implement as many changes as they can gradually—and view them as lifelong habits, not temporary adjustments.
Surgery
A 2024 study reports that acid reflux surgery has an 80% average success rate, with reduction of symptoms lasting for over 20 years. While effective, surgery is not a first-line treatment option. Instead, a gastroenterologist may recommend surgery when: the alternative is ongoing prescription medication, when your GERD stems from structural issues like a hiatal hernia, or when someone has developed complications associated with GERD, such as Barrett’s esophagus.
GERD typically responds to three different surgeries, depending on the underlying cause:
- LINX device implantation: A newer surgery that places a medical device around the LES, helping to control what direction food moves in and what does (and doesn’t) get through the LES.
- Nissen fundoplication: A procedure that wraps the stomach around the esophagus, fixing a hiatal hernia.
- Transoral incisionless fundoplication (TIF): A more minimally invasive version of Nissen fundoplication that doesn’t involve an incision and offers a faster recovery.
When to see a doctor
If acid reflux occurs more than twice a week, it’s time to see a GI provider. Even if you decide to treat acid reflux with lifestyle changes and OTC medications, a GI provider can help create an effective treatment plan tailored to your symptoms, triggers, and lifestyle.
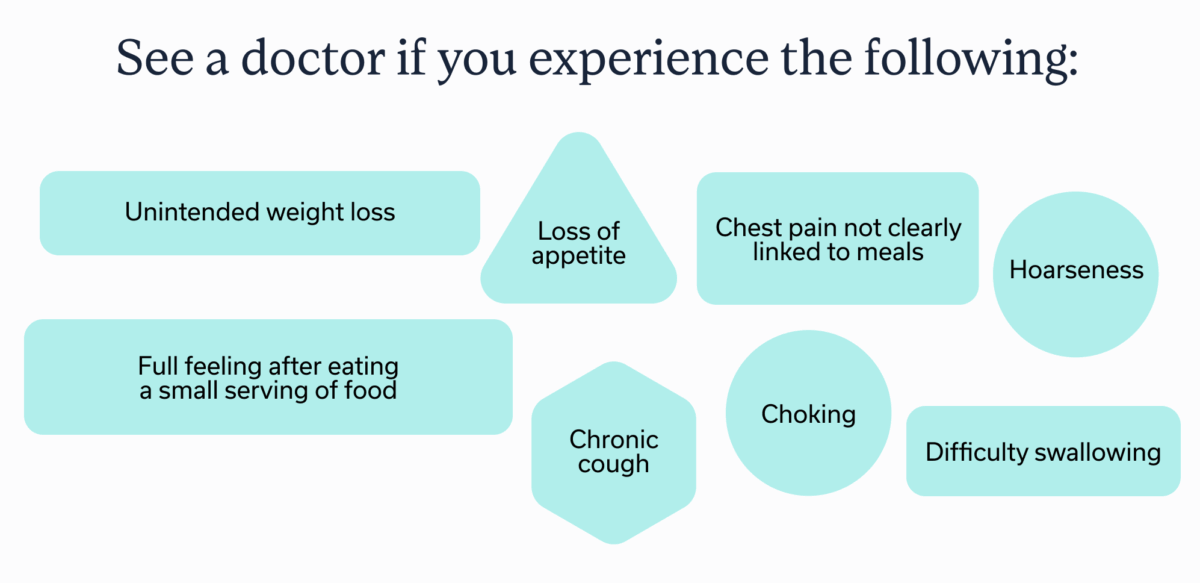
Regardless of how often your acid reflux occurs, contact a doctor if you experience:
- Chest pain not clearly linked to meals
- Choking
- Chronic cough
- Difficulty swallowing
- Hoarseness
- Full feeling after eating a small serving of food
- Loss of appetite
- Unintended weight loss
If you have blood in your stool, dark tarry stools, or are vomiting non-stop, especially if your vomit contains blood, contact emergency medical services.
Oshi Health’s approach to treating GERD
Of course, deciding that you’re going to change how you eat and exercise, among other lifestyle factors, and actually making those changes are two different things. The latter is much harder, especially if you have a busy schedule (and who doesn’t nowadays?).
Fortunately, a 2023 study found four key components to sticking to GERD lifestyle interventions:
- Working with a collaborative care team (i.e. a GI provider, GI dietitian, and gut-brain specialist who all work together to provide support)
- Staying motivated to change your habits
- Utilizing strategies that make implementation of lifestyle changes less challenging/more effective
- Understanding the impact of the disease
Oshi Health has combined all four of those factors into a collaborative GI care model. The Oshi team approaches GERD from behavioral, dietary, and medical angles, working with patients to discover and treat GERD symptoms. If you’re looking for a personalized treatment plan based on your symptoms and lifestyle, you can take the first step here.
Key takeaways
- Although occasional acid reflux isn’t dangerous, GERD can be: When left untreated, acid reflux can cause serious complications.
- GERD can reduce quality of life: Untreated GERD can negatively impact someone’s quality of life, mental health, and overall well being.
- GERD treatment is effective: GERD can usually be treated through medication, lifestyle changes, or, in severe cases, surgery.
- A GI care team, like the one at Oshi Health, can offer guidance and support to those looking to treat the underlying causes of GERD and acid reflux.
Frequently asked questions (FAQs)
-
Acid reflux is serious when you regularly experience more than two occurrences per week. Signs of more severe cases also include difficulty breathing, pain when swallowing, loss of appetite, and vomiting.
-
There isn’t a set time frame before acid reflux becomes dangerous. As a rule of thumb, it’s best to seek treatment if you experience symptoms more than twice a week. Prompt treatment and lifestyle changes can help you avoid more serious complications.
-
Over-the-counter medications, like antacids, and gentle movement after eating can help make acid reflux go away. Prescription medications and surgery may help in severe cases. Many people may also prevent future acid reflux flares by changing their diet and exercise routine, reducing stress, and avoiding food triggers, like spicy foods or citrus fruits.
-
Acid reflux, especially chronic acid reflux, which is referred to as GERD, can potentially lead to serious complications. These include respiratory infections, Barrett’s esophagus, esophagitis, esophageal strictures, and a higher risk of esophageal cancer.
Oshi is your partner in digestive health
Feel like your digestive concerns are running your life? You’re not alone—and we’re here to help you find lasting relief.
Oshi Health GI providers, gut-brain specialists, and registered dietitians work together to address your symptoms and find solutions that actually work for you.
Whether you’re dealing with chronic digestive issues or unpredictable symptom flare-ups, our GI specialists deliver:
✔ Personalized care plans tailored to your lifestyle
✔ Science-backed strategies to calm your gut
✔ Compassionate, whole-person care
✔ And so much more!
Ready to take control of your gut health?