Irritable bowel syndrome (IBS) is one of the most commonly diagnosed gastrointestinal (GI) conditions. It involves several different types, each with different symptoms, and several ways to treat. IBS affects the female body at twice the rate as the male body and has links to menstrual cycle issues. If you have IBS, an experienced clinician can design a treatment plant that’s unique to your needs.
Having irritable bowel syndrome (IBS) means you experience abdominal discomfort with changes in bowel movements or habits. IBS can be a frustrating and confusing diagnosis—not to mention that talking about poop can sometimes feel awkward. However, with the right patient-clinician relationship and individualized treatment plan, the condition can be managed so that you can get back to feeling better.
“IBS, as a disorder of gut-brain interaction (DGBI), is best understood through an individual lens,” says Steven Feinstein, PhD, a clinical health psychologist and gut-brain specialist at Oshi Health. “[IBS] requires a provider to first listen to each patient’s story to understand and help identify specific contributing factors. These specific factors then lead to an individualized plan of empirically based treatments that best fits each person’s life situation.”
As someone diagnosed with IBS, I can concur that an individualized approach is what has helped me most. I have endometriosis, a systemic inflammatory disease that often involves pelvic pain. People with endometriosis are three times more likely to develop IBS than those without. (I was unlucky enough to get this double whammy.) My clinicians must understand my complex relationship with pelvic pain, how endometriosis affects GI health, and more to help me manage my IBS.
In this article, we’ll dive into a deep understanding of IBS, what causes or triggers it, how it’s managed with an individualized plan, and more.
Understanding irritable bowel syndrome
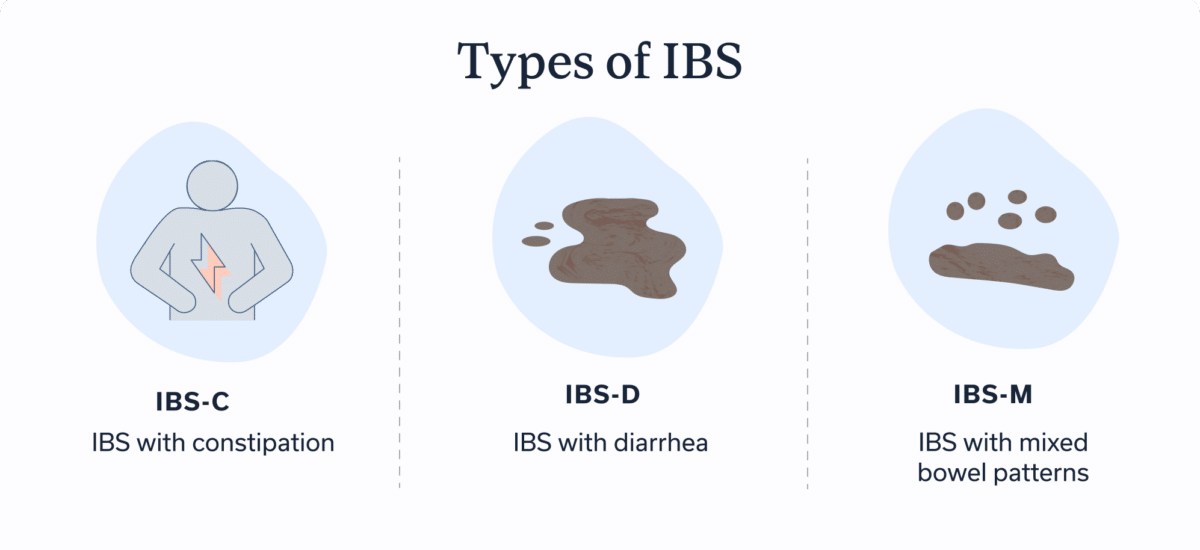
IBS is the most commonly diagnosed GI disease, with 10 percent to 15 percent of people experiencing it. IBS is a symptom-based diagnosis. This means that someone who has IBS experiences symptoms of abdominal discomfort with changes in their bowel movements. Your symptoms with IBS may vary, depending on the type. IBS involves three main types.
Types of IBS
- IBS-C: IBS with constipation
- IBS-D: IBS with diarrhea
- IBS-M: IBS with mixed bowel patterns
IBS symptoms and diagnosis
Your symptoms may vary, depending on the type of IBS you have. And even across these subtypes of IBS, symptoms can be different from one patient to the next.
Common IBS symptoms
- Abdominal pain
- Bloating
- Changes in how often you pass stool
- Changes in stool form or appearance
- Constipation
- Diarrhea
- Distension
- Feeling like you’ve had an incomplete bowel movement
- Feeling unwell
- Gas
- Mucus in the stool
- Pain with bowel movements
- Straining with bowel movements
- Urgency
- Vacillating between constipation and diarrhea
Just an FYI: The acronym for irritable bowel syndrome (IBS) is sometimes confused with IBD. IBD stands for inflammatory bowel disease, which is an umbrella term that includes the conditions Crohn’s disease and ulcerative colitis. Having IBD means you have chronic inflammation of the GI tract. In IBD, you have damage to your intestines. In IBS, there’s no structural damage; rather, it’s an issue with how your gut functions. However, IBD and IBS can have similar symptoms, and some people have both conditions.
Diagnosing IBS
Before researchers had a better understanding of IBS, the consensus was that IBS was a diagnosis of exclusion. This meant that clinicians worked to rule out other GI conditions, sometimes with invasive procedures, before diagnosing IBS. Experts now say that IBS is an affirmative or positive diagnosis, meaning that doctors base a diagnosis on symptoms by looking at what’s called the Rome IV criteria, an international method for diagnosing functional GI disorders that the nonprofit Rome Foundation created.
Rome IV criteria for diagnosing IBS
- Recurrent abdominal pain for an average of at least one day per week over the past three months.
- Two or more of the following
- Symptoms are related to going number two.
- Symptoms are associated with a change in how often you’ve got to go..
- Symptoms are associated with a change in how your poo looks.
Despite the change in diagnostic criteria, most clinicians who aren’t experts in IBS still treat the condition as a diagnosis of exclusion. This often results in unnecessary and expensive testing. These factors highlight the need for knowledgeable and empathetic GI experts. At Oshi Health, we view the patient in a “whole-person” manner, which allows us to identify and treat GI issues for lasting relief.
Meet Oshi Health
An integrated team of GI specialists, working together for you
Our expert gastroenterologists, GI providers, registered dietitians, and gut-brain specialists are leaders in their fields, with advanced education and training in gastroenterology. Our comprehensive team approach is personalized to meet your unique needs and address the root cause of your symptoms.
IBS and the female body
IBS affects the female body at nearly double the rate of the male body. One reason may be that people with conditions that cause pelvic pain, such as endometriosis, polycystic ovary syndrome (PCOS), and premenstrual dysphoric disorder (PMDD), are more at risk for IBS. My dual diagnosis of endometriosis and IBS serves as a good example. I have an impaired stress response from experiencing chronic pain, and this impaired stress response likely contributes to my IBS symptoms.
By the way, those assigned female at birth tend to experience IBS-C and abdominal pain, whereas those assigned male tend to have IBS-D. One possible factor in this difference may be the menstrual cycle. Research shows that more people with IBS experience constipation during the luteal phase, which begins just after ovulation and ends when you get your period.
Additionally, childhood sexual abuse and sexual abuse in adulthood, such as assault and rape, have links to IBS. Though sexual abuse is underreported in males, it is more prevalent in females.
What causes IBS?
Researchers don’t yet know the exact causes of IBS. However, various factors likely play a role. IBS is a functional disorder, meaning that it occurs because the GI tract is having trouble performing its functions for one reason or another. Several factors can disrupt optimal functioning of the GI tract.
Disrupted gut-brain connection
The gut and the brain communicate along what’s called the gut-brain axis. But sometimes this communication can become disrupted. Your GI tract has an extensive network of millions of neurons along its walls. This network is called your enteric nervous system (ENS). It controls your digestive functions, including gastric secretions and motility, which is the movement of food and waste.
The enteric nervous system is a division of your autonomic nervous system (ANS), which controls the involuntary responses in your body. Other divisions of the ANS include your parasympathetic nervous system (PNS), also called “rest and digest,” and the sympathetic nervous system (SNS), also called “fight or flight.” As you may have guessed the PNS is your “calm” response, whereas the SNS is your “stress” response.
When we’re stressed, depressed, or feeling anxious, our stress response can disrupt our PNS and ENS and cause a jam-up on the gut-brain communication highway. “It is when the nervous system responds to a perceived threat, ‘stress,’” Dr. Feinstein says, “that this communication is disrupted, and can become a significant contributing factor to an increase in gut dysregulation, and the often-associated increase in GI symptoms.”
As an example, let’s consider my pelvic pain from endometriosis. After more than three decades of living with the condition, my body is hardwired to perceive anything related to my abdominal area as a threat even when it’s not. Perceived threats include, in some cases, eating food and going to the bathroom. Therefore, the dysregulation between my gut and brain can lead to IBS symptoms.

Not all in your head
Having a disrupted gut-brain connection does not mean that IBS is “all in your head.” Instead, your brain and gut are having difficulty communicating, and therefore your gut has trouble performing its functions.
Disruptions to the gut-brain axis are common in people who have the following:
- Adverse childhood experiences (ACEs)
- Anxiety
- Chronic pain conditions
- Chronic stress
- Depression
- Post-traumatic stress disorder (PTSD)
When the gut-brain axis is disturbed or upset, effects (primarily GI symptoms) can show up as IBS.
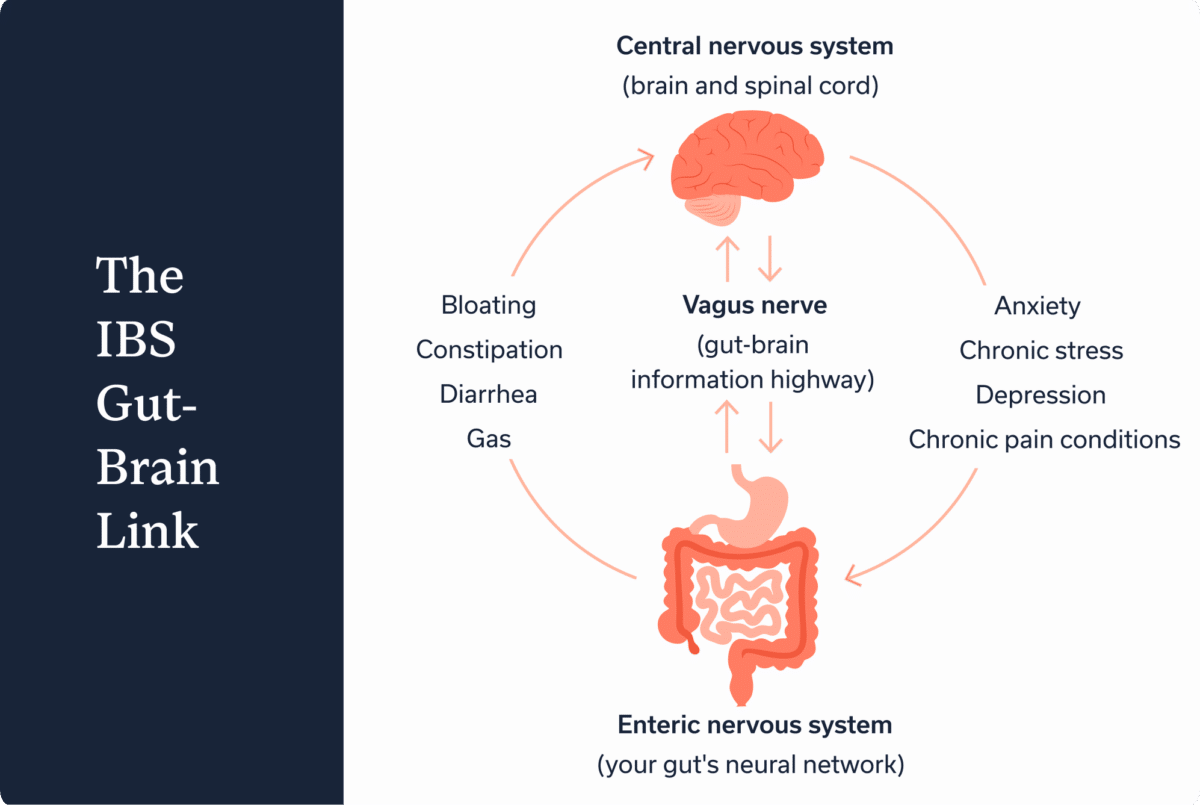
Motility disturbances. If the gut and brain aren’t communicating effectively, the movement of food and waste through the digestive tract may be impaired. This impairment might lead to diarrhea, constipation, or a mix. It could also lead to gas, bloating, or other not-so-fun symptoms.
Visceral hypersensitivity. We shouldn’t experience pain when our organs are just doing their jobs. However, this is exactly what happens when people have visceral hypersensitivity. Sometimes visceral hypersensitivity involves a heightened sense of pain in response to stimuli that actually is painful. Or, it involves a sense of pain in response to stimuli that doesn’t generally cause pain.
Other concerns associated with IBS
These often appear alongside IBS but aren’t necessarily the cause.
Gastrointestinal infection. In some cases, an acute gastrointestinal infection, such as norovirus, may trigger post-infection IBS (PI-IBS).
Gut dysbiosis. The gut microbiome, all the bacteria and fungi that live in the gut, can become disrupted, which may play a role in IBS.
Intestinal barrier damage or dysfunction. Many people with IBS have dysfunction in their gut barrier, the several-layer lining of the gut that absorbs nutrients and helps protect the rest of the body from pathogens.
Bile acid malabsorption. People experiencing IBS-D may have bile acid malabsorption, where your intestines don’t absorb bile acids properly. Instead you end up with excess bile acids, which can result in diarrhea.
IBS trigger foods
Food is not a cause of IBS, but if you have IBS, some foods may trigger symptoms. Which foods trigger one person may be different for another person with the condition. Working with a GI registered dietitian can help you determine which foods are triggering for you. That way you can avoid eliminating foods unnecessarily.
IBS trigger foods:
- Alcohol
- Caffeine
- Citrus
- Dairy
- Fatty foods
- Fried foods
- FODMAP foods
- Histamine foods
- Legumes (beans and lentils)
- Spicy foods
Treatment options for IBS
“Living with IBS can be overwhelming and frustrating,” says Idequiz Paez, RD, a GI registered dietitian with Oshi Health. “But with the right support, it can be effectively managed. In my seven years specializing in GI nutrition, I’ve seen countless patients who silently struggled for years, only to experience significant symptom improvement once they found the right interventions.”
The right interventions for you will depend on your specific circumstances and lifestyle factors. “When all these factors are considered and treatment is designed to match,” Dr. Feinstein says, “it leads to better outcomes. To reach symptom control, this individualized approach by an integrated multidisciplinary treatment team is best practice.”
Paez agrees that what works for one person may not work for the next. “Individualizing a care plan is important in the treatment of IBS due to the variety of symptoms patients can experience and the complexity from one patient to the next,” she says. “It is also important to consider patient preferences and lifestyle to find an approach that not only works for them but can be sustainable for long-lasting relief.”
Your care plan may include a combination of mental health therapies to enhance the gut-brain connection, medications or supplements if needed, and diet and lifestyle changes that can help you reduce exposure to food and other triggers, such as stress. Oshi Health takes a team-based approach, which often proves more effective than working with just one GI expert.
Mental health therapies for IBS
Some mental health therapies that support the gut-brain connection can be helpful for IBS. “Tools that control the nervous system help us learn how to better maintain this important regulating connection and control symptoms,” Dr. Feinstein says. “When providing gut-brain specialty treatment, communication along the gut brain axis is the focus of treatment.”
Cognitive-behavioral therapy (CBT), for example, helps you retrain your brain to alter dysfunctional patterns of thinking. For example, in the case of my endometriosis, I might think that eating will make me bloated and experience pelvic pain. This thought pattern can fuel my anxiety around eating, which can disrupt my gut-brain connection and increase the likelihood of my experiencing bloating and pain. Instead, I can practice retraining that thought pattern through CBT.
CBT also builds your problem-solving skills to take a solutions-based, empowering approach rather than getting caught up in negative thought patterns. For example, I know I have methods to prevent bloating and reduce it if it occurs. When I focus on these solutions, I feel empowered to relax and enjoy my food.
As a treatment for IBS, CBT can also help you build relaxation strategies and make you more aware of where you’re holding tension that may lead to IBS symptoms.
Lifestyle and diet changes for IBS
Stress management and dietary changes can also help manage IBS symptoms.
Stress-management techniques. Managing stress can help you reduce your stress response so that you can tap into your calm response. This can help lessen disruption to your gut-brain connection. Stress management can take many forms, including meditation, yoga, exercise, and more.
Dietary changes. Working with a GI registered dietitian can help you investigate which foods or eating habits tend to trigger your symptoms.
Medications and supplements for IBS
In some cases, your clinician may prescribe medications to treat IBS. Medications for IBS are help gut motility, alleviate pain or cramping, or ease constipation or diarrhea. Other medications, such as antidepressants, can help support mental health.
Supplements may also help you support your gut microbiome, gut motility, intestinal barrier, and more. However, you should consult your clinician before starting new supplements or medications to ensure they won’t cause an IBS flare.
FAQ
-
You can manage IBS with a customized treatment plan from a clinician who is well-versed in the condition. Your treatment plan may include therapies that help enhance gut-brain communication, as well as lifestyle and dietary changes that help reduce triggers and ease symptoms. It may also include medications or supplements if needed.
-
IBS can include many symptoms, including constipation, diarrhea, bloating, gas, abdominal pain, and more.
-
Although no definitive cure exists for IBS, you can find effective ways to reduce and manage symptoms. Your symptom management will likely be different from the next person’s with IBS. A personalized approach from an experienced clinician is best.
-
How to stop an IBS flare will depend on your unique symptoms and other factors. Working with an experienced clinician can help you develop a flare prevention and treatment plan.
-
Researchers don’t yet know the cause of IBS. However, a disruption between how the gut and brain communicate is a common issue in people who have IBS.
Takeaway
IBS can feel like a frustrating condition because it can lead to uncomfortable symptoms. However, with the right individualized treatment plan, you can manage your IBS in a way that lessens your discomfort and GI issue, while avoiding unnecessary and expensive testing.
If you frequently have abdominal discomfort associated with changes in bowel habits, whether constipation, diarrhea, or both, you should talk to an IBS expert who can help. Oshi Health takes a multidisciplinary approach, which may include working with a gut-health behavioral specialist, a GI registered dietitian, and more. Schedule a visit.
Oshi is your partner in digestive health
Feel like your digestive concerns are running your life? You’re not alone—and we’re here to help you find lasting relief.
Oshi Health GI providers, gut-brain specialists, and registered dietitians work together to address your symptoms and find solutions that actually work for you.
Whether you’re dealing with chronic digestive issues or unpredictable symptom flare-ups, our GI specialists deliver:
✔ Personalized care plans tailored to your lifestyle
✔ Science-backed strategies to calm your gut
✔ Compassionate, whole-person care
✔ And so much more!
Ready to take control of your gut health?