Gut health for women and others assigned female at birth is uniquely shaped by the menstrual cycle, menopause, pregnancy, and how the gut talks to your brain and immune system. Learning about these complicated links can improve digestive wellbeing, overall health, and your quality of life.
When we think of “women’s health,” gynecological concerns like period pain or fertility issues often come to mind. But there’s another part of the body that deserves attention, too: the gut. Turns out, the gastrointestinal (GI) system operates differently for those who menstruate, which can lead to a host of digestive symptoms, from diarrhea to bloating and beyond. But why exactly does gut health differ for people who menstruate? It all comes down to hormones, which are constantly shifting throughout the menstrual cycle. Hormonal shifts during pregnancy and menopause can impact your digestive system as well.
In turn, your gut can influence pregnancy outcomes, how we experience menopause, our mental health, and so much more. Yet despite impacting half of the population, the unique gut health challenges women and those who menstruate face aren’t talked about enough. Here’s the rundown on how to keep your gut happy, no matter what stage of life you’re in.
What is gut health, exactly?
Gut health matters for everyone, regardless of sex, age, and/or race. Smooth digestion helps you avoid stomach cramps and uncomfortable bathroom emergencies—and that’s reason enough to care about it. But gut health is also connected to pretty much everything else in your body: It impacts your immune system, cardiovascular system, cognitive health, and protects your body against harmful bacteria. Your gut and brain even communicate back and forth, meaning when your digestive system is off, your mental health can take a hit too.
And get this: Over 70% of the immune system lives in the gut, which is especially relevant to people who menstruate since we are more likely to be diagnosed with an autoimmune disease.
Gut health and gynecological health
The deep link between gynecological health and gut health goes both ways: A strong gut supports the health of a pregnant person and their baby, is associated with fewer premenstrual symptoms, and aids in balancing estrogen levels, which improves overall health.
On the less positive side, when there’s an imbalance in the gut, something doctors call “gut dysbiosis,” the risk is higher for difficult menopausal transitions, breast cancer, ovarian cancer, cervical cancer, and some gynecological conditions, such as polycystic ovarian syndrome.
“Gut health is different for women because our gut microbiome is influenced very much by our hormones,” says Pradnya Mitroo, MD, a board-certified gastroenterologist and President of Fresno Digestive Health. This is true both during the monthly menstrual cycle, pregnancy, and once someone enters perimenopause and eventually menopause.
Common gut health issues affecting women
People who menstruate experience more GI symptoms than those who don’t—and that includes bloating, constipation, diarrhea, and functional dyspepsia (FD), a condition marked by early satiety, pain in the upper abdomen, and nausea. This is true regardless of age, though premenopausal individuals report more symptoms than those in perimenopause or menopause.
Those who menstruate are also more likely to experience certain gastrointestinal diseases, including:
- Celiac disease: People who menstruate are more than twice as likely to develop celiac disease, an autoimmune condition where the small intestine cannot process gluten.
- Chronic constipation: In one study, researchers found people who menstruate may be twice as likely to experience constipation than those who don’t.
- Irritable bBowel sSyndrome (IBS): IBS is twice as likely to affect those assigned female at birth, and symptoms are more severe in this group as well.
- Inflammatory bBowel dDisease (IBD): Unlike the others on this list, biological sex doesn’t impact the likelihood of getting IBD. However, people who menstruate and have IBD report a worse quality of life and more psychological symptoms.
Menstruation and gut health
“The hormones that regulate the menstrual cycle, especially estrogen and progesterone, also affect the digestive tract,” explains Treta Purohit, MD, a board-certified gastroenterologist and hepatologist and Executive Medical Director at Oshi Health, adding that the levels of these hormones rise at different phases of the menstrual cycle, which in turn can cause different GI symptoms at different points in the cycle.
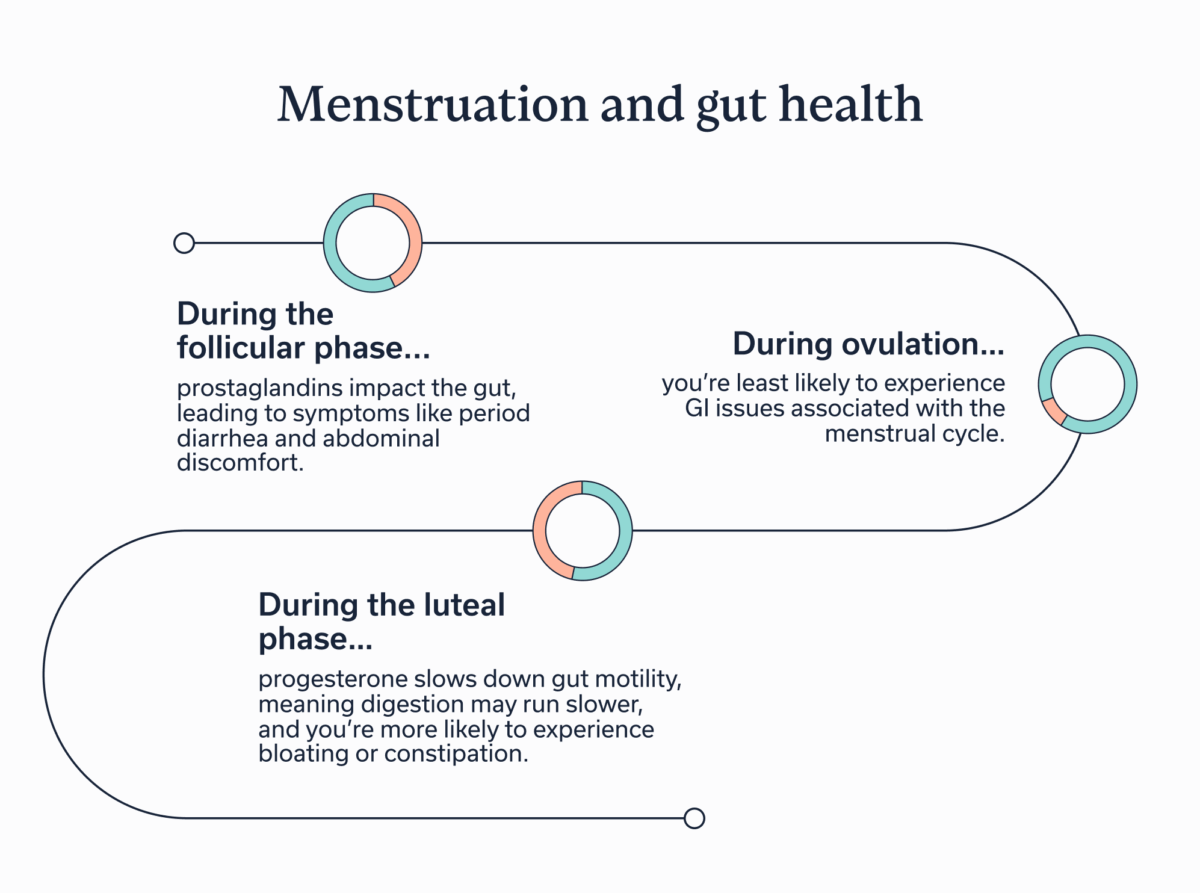
If you’re fuzzy on the details of your menstrual cycle, here are the exact phases, along with the GI symptoms that often accompany them:
- Follicular phase: This phase runs from the first day of your menstrual period until ovulation begins, and it’s when prostaglandin levels rise. Prostaglandins are natural chemical messengers that, among other functions, tell the uterus to contract and shed its lining, which results in period blood. Prostaglandins also impact the gut, leading to symptoms like period diarrhea and abdominal discomfort.
- Ovulation: A transitional period between the follicular and luteal phase when you’re least likely to experience GI issues associated with the menstrual cycle.
- Luteal phase: This phase starts after ovulation and runs until you get your period. During the luteal, progesterone levels rise. Progesterone slows down gut motility, meaning digestion may run slower, and someone’s more likely to experience bloating or constipation.
Pregnancy and gut health
Pregnancy brings some of the most dramatic hormonal shifts a person will ever experience, and those changes can directly influence digestion, gut bacteria, and overall gut health. During pregnancy, progesterone levels increase, resulting in around 40% of pregnant people and 52% of postpartum individuals experiencing constipation.
But constipation isn’t pregnancy’s most famous GI side effect. That award goes to nausea and vomiting—aka morning sickness, though it can happen at any time day or night. About 80% of people experience vomiting or nausea during pregnancy, usually in the first trimester. The reason for this symptom is unknown, though it’s probably a combination of hormone fluctuations, enhanced smell, and a higher likelihood of acid reflux, food leaking back into the esophagus and throat once it has passed into the stomach, during pregnancy.
While not a change per se, those who have certain gastrointestinal conditions, such as inflammatory bowel disease and liver disease, also have a higher risk of complications during conception, pregnancy, and postpartum. Successful management of these conditions greatly decreases these risks.
Perimenopause, menopause, and gut health
Perimenopause is the transition from having menstrual cycles (and thus, being able to get pregnant) to menopause, which is marked by having no menstrual cycles for 12 consecutive months. Perimenopause typically takes place between the ages of 45 and 55, and the average age of menopause itself is 52 in the United States.
“There are a lot of hormone changes that occur with perimenopause and menopause which change the bacteria in our gut,” explains Mitroo, pointing out that these changes often lead to a change in the ratio of different bacteria in the gut. This adjustment in the gut microbiome contributes to common menopause symptoms like a slower metabolism and weight gain.
We’ve already touched on how constipation can affect people when they’re pregnant or during certain phases of the menstrual cycle, but it’s also a concern during menopause. “Constipation is a major issue for women in menopause as the gut microbiome changes and slows down the colon,” explains Dr. Mitroo.
Gut-brain connection in women
If you’ve felt knots in your stomach before a first date or big work presentation, you’ve experienced the gut-brain connection in action. But for people who menstruate, this connection works a bit differently.
This is because the hypothalamic pituitary adrenal (HPA) axis, the part of the brain that’s connected to the gut, behaves differently in women.
“Women exhibit greater activation of the hypothalamic-pituitary-adrenal (HPA) axis under stress, which can exacerbate GI symptoms,” says Dr. Purohit, “Anxiety and depression—more prevalent in women with IBS—further amplify this response.”
How to improve gut health: practical steps for women
So, what can you do to heal your gut and/or keep it in tip-top shape? The answer lies in your diet and lifestyle. “It is most important for women to eat a whole food unprocessed diet to maintain a healthy microbiome,” says Dr. Mitroo.
If you’re wondering what a whole food, unprocessed diet means, keep reading. We’re about to detail what foods you should and shouldn’t eat, plus two lifestyle changes that support these gut-friendly eats.
Foods that promote a healthy gut
As a general rule of thumb, opt for minimally-processed foods that contain good gut bacteria. Many ingredients fit this profile, and a GI registered dietitian, like those at Oshi Health, can help you create a nutritional plan that suits your taste and help you find the specific foods that do, and don’t, agree with your gut.
That said, there are a few general recommendations most of us can benefit from:
- Eat more fiber: “Women should have at least 35-40 g of fiber daily,” says Dr. Mitroo, “These foods feed the gut bacteria and then act like a broom to move things along.”
- Aim for more soluble fiber: While fiber is a great place to start, you ideally want to increase the soluble fiber in your diet. Dr. Purohit recommends, “Favor soluble fiber (like oats and fruits) over insoluble fiber, and increase gradually.”
- Go heavy on the plants: “Plant foods, with their robust profile of micronutrients— vitamins, minerals, and antioxidants, along with fiber—are among the most powerful, supporting digestion and a diverse microbiome,” explains Kaitlin Voicechovski, MS, RD, LDN, the Lead Registered Dietitian at Oshi Health, “Women can benefit from adding plants into their diets, which can be inclusive of everything from fruit and vegetables to grains, legumes, and fresh herbs and spices.”
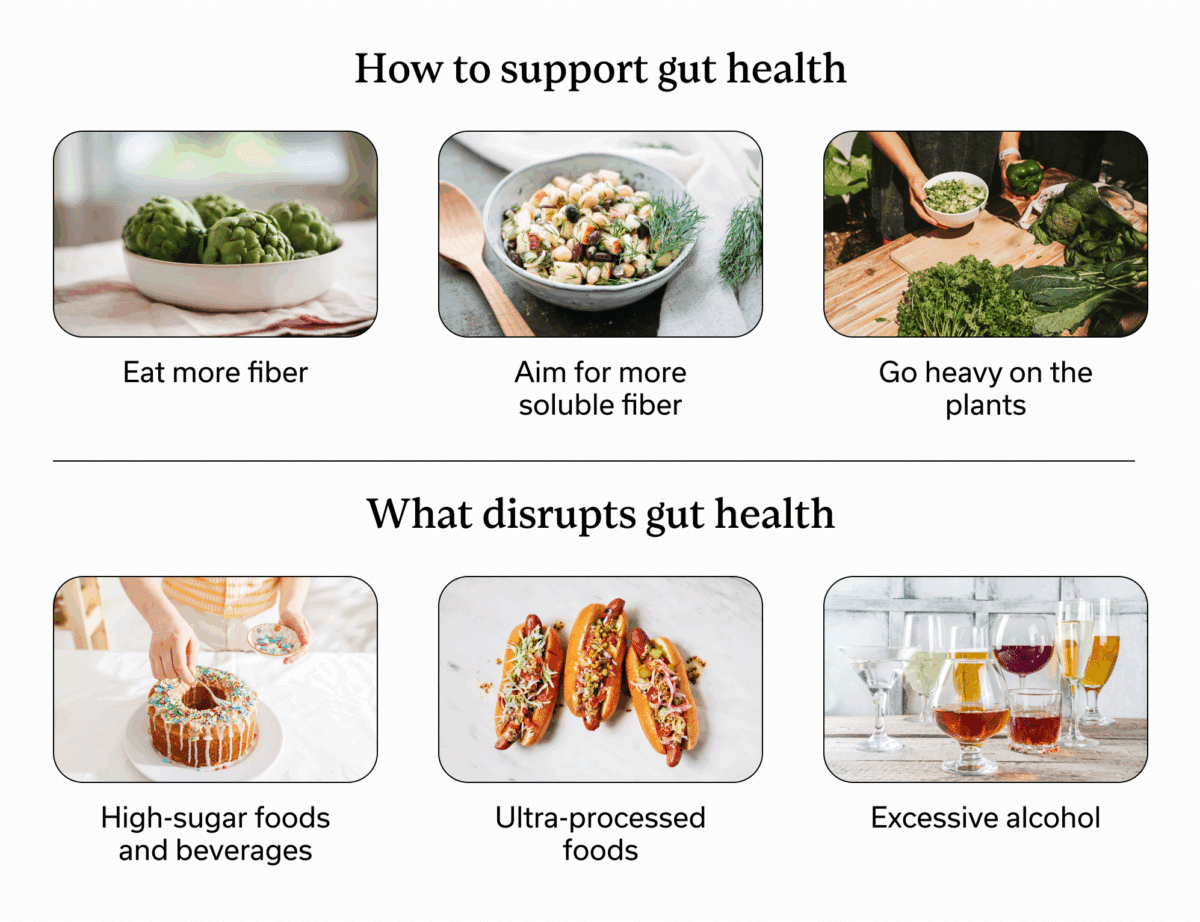
Foods that can disrupt gut health
Foods that disrupt gut health vary from person to person, depending on your unique gut microbiome. An apple, for example, may cause IBS symptoms for one person but be perfectly ok for someone else.
While a GI registered dietitian can help you find personal no-go foods, there are a few common culprits to avoid:
- High-sugar foods and beverages: These contribute “bad” bacteria to the gut and increase intestinal inflammation.
- Ultra-processed foods: All foods are processed in order to be safe for eating, but ultra-processed foods harm the gut microbiome and contribute to intestinal inflammation. As a rule of thumb, the longer the ingredient list and the more items you don’t recognize as real foods, the more processed it is.“Women should consider limiting ultra-processed foods,” advises Voicechovski, “These foods tend to offer fewer health-promoting nutrients and may be higher in salt, added sugars, saturated fats, etc., which, for some, can impact digestion and exacerbate unwanted symptoms.”
- Excessive alcohol: The third in this trifecta is excessive alcohol. Too much alcohol negatively alters the gut microbiome, can damage the liver, and may lead to nutritional deficiencies.
Managing stress
The gut-brain connection is a two-way street, meaning that when you reduce stress and anxiety, gut health may also improve. Working with a gut-brain specialist, such as a GI psychologist, can help, and there are some at-home strategies to try as well. Meditation, positive self talk when a GI event occurs, and hypnotherapy, for example, may reduce mental health symptoms and stress-related GI symptoms.
Physical activity
Regular exercise improves gut motility (how well food moves through the digestive system) and mental health. It also enhances microbiome composition (aka it leads to more healthy gut bacteria) and is correlated with fewer symptoms for those with GI conditions like IBS and IBD.
And when we say regular exercise, we don’t mean that you have to become a powerlifter or sign up for a marathon (though more power to you if either is your workout of choice). Moderate exercise, such as regular walks or pilates classes, provides these benefits too.
When to see a healthcare provider
We all experience GI symptoms from time to time, whether it’s bloating during your period or diarrhea when you have the flu. But when do GI symptoms merit a visit to a healthcare provider? Specific symptoms to watch out for include:
- Constipation or diarrhea that is severe or persistent
- Frequent digestive discomfort, like bloating or abdominal pain
- Mood changes, anxiety, or depression linked to gut discomfort
- Pain during bowel movements or when urinating
- Trouble getting pregnant
- Unexplained, sudden weight gain or loss
- Very irregular or heavy bleeding during menstruation
For people who menstruate, there’s yet another reason to see a GI provider: Many symptoms overlap between GI and gynecological conditions, and a trained medical professional needs to diagnose what’s actually going on.
“When considering women’s gut health, it’s important to consider the nuances of hormones and the common overlap that exists between gynecological conditions, GI conditions, and their associated symptoms,” explains Voicechoski, “Some GI conditions and gynecological conditions can present similarly, making diagnosis challenging; one example of this overlap is IBS and endometriosis. Pelvic floor dysfunction is also more prevalent in women versus men, which may contribute to concerns such as constipation.”
Key takeaways
- Gut health differs based on biological sex, with hormone fluctuations often leading to a higher risk of certain GI symptoms and conditions for those who menstruate.
- The gut microbiome balance also shifts throughout the menstrual cycle and during pregnancy, perimenopause, and menopause.
- No matter what stage of life you’re in, it’s possible to have a healthy gut. If experiencing GI symptoms or if you are concerned about your gut, contact a GI specialist, such as the providers at Oshi Health.
Frequently asked questions (FAQs)
-
Some of the best ways to improve gut health as a woman are to eat a balanced diet full of fiber, fruits, vegetables, and other whole foods, to reduce stress, and to exercise regularly. If symptoms are ongoing or disrupt daily life, working with a GI provider is essential to improve GI health.
-
Signs of bad gut health include bloating, constipation, diarrhea, and passing more gas often than usual. Abdominal pain, irregular digestion, and pain during bowel movements or urinating point to an underlying gastrointestinal condition as well.
-
Some of the best foods for women’s gut health are fiber, especially sources of soluble fiber like oats and fruits, and plant-based foods, such as legumes, grains, vegetables, herbs, and spices.
Oshi is your partner in digestive health
Feel like your digestive concerns are running your life? You’re not alone—and we’re here to help you find lasting relief.
Oshi Health GI providers, gut-brain specialists, and registered dietitians work together to address your symptoms and find solutions that actually work for you.
Whether you’re dealing with chronic digestive issues or unpredictable symptom flare-ups, our GI specialists deliver:
✔ Personalized care plans tailored to your lifestyle
✔ Science-backed strategies to calm your gut
✔ Compassionate, whole-person care
✔ And so much more!
Ready to take control of your gut health?