GLP-1 drugs are a hot topic for a reason: They can help with weight management and type 2 diabetes. But for over 40% of those on the medication, they also cause a sick-to-the-stomach feeling, aka nausea. Fortunately, there are strategies to manage GLP-1 nausea and prevent future bouts.
One in eight Americans are taking or have taken a glucagon-like peptide-1 receptor agonist (GLP-1). And if GLP-1 isn’t a familiar term, you’ve probably heard of one of the medications in this drug class, such as Ozempic or Wegovy. There’s no denying that this drug class can lead to significant health benefits, particularly for those with type 2 diabetes and/or obesity. But GLP-1s also come with some tricky-to-manage side effects.
One of the most common is nausea. No matter your reason for taking a GLP-1—whether for blood sugar control, weight management, or to reduce the risk of heart disease—it’s possible to develop a sick-to-the-stomach feeling while on the drug. Depending on the individual, drug, and dosage, GLP-1 nausea can be persistent or infrequent, mild or severe. No matter how GLP-1 nausea manifests, there are ways to manage this side effect.
What is GLP-1 and how does it work?
Most of us probably hadn’t heard of GLP-1 before the release of Ozempic and other popular drugs, but GLP-1 is actually a naturally occurring hormone. All of us produce GLP-1, which is an incretin hormone that gets released into our bloodstream when we eat. Once in the bloodstream, this hormone helps regulate digestion, appetite, and blood sugar.
If someone has type 2 diabetes and/or obesity, however, their naturally occurring GLP-1 may not be as robust. And that’s where GLP-1 medications come in. This drug class mimics the effects of this naturally occurring hormone, boosting metabolism regulation.
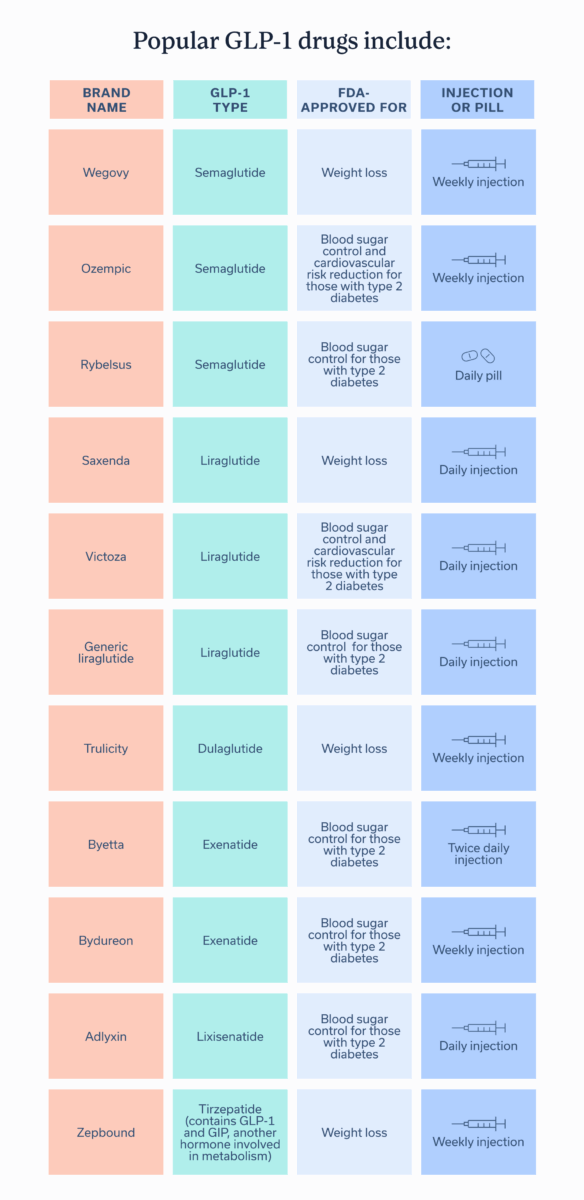
Depending on the exact brand name drug, GLP-1s are FDA-approved to help manage type 2 diabetes, to facilitate weight management, or to help with both. These drugs are available as a daily or weekly injection or a daily pill.
Popular GLP-1 drugs include:
| Brand name | GLP-1 type | FDA-approved for | Injection or pill |
| Wegovy | Semaglutide | Weight loss | Weekly injection |
| Ozempic | Semaglutide | Blood sugar control and cardiovascular risk reduction for those with type 2 diabetes | Weekly injection |
| Rybelsus | Semaglutide | Blood sugar control for those with type 2 diabetes | Daily pill |
| Saxenda | Liraglutide | Weight loss | Daily injection |
| Victoza | Liraglutide | Blood sugar control and cardiovascular risk reduction for those with type 2 diabetes | Daily injection |
| Generic liraglutide | Liraglutide | Blood sugar control for those with type 2 diabetes | Daily injection |
| Trulicity | Dulaglutide | Weight loss | Weekly injection |
| Byetta | Exenatide | Blood sugar control for those with type 2 diabetes | Twice daily injection |
| Bydureon | Exenatide | Blood sugar control for those with type 2 diabetes | Inject weekly |
| Adlyxin | Lixisenatide | Blood sugar control for those with type 2 diabetes | Inject daily |
| Zepbound | Tirzepatide (contains GLP-1 and GIP, another hormone involved in metabolism) | Weight loss | Inject weekly |
Why do GLP-1 drugs cause nausea?
While GLP-1 drugs offer various benefits, they come with side effects, many of which can have an impact on your stomach or other parts of your digestive tract. One of the most commonly reported side effects across GLP-1 types is nausea, a sick-to-the-stomach feeling that often creates an urge to vomit, and a loss of appetite. We’ve all experienced this sensation at one point or another, whether after eating something that didn’t agree with us or when we contracted a stomach flu. The problem is that some people experience that nausea persistently while on GLP-1s.
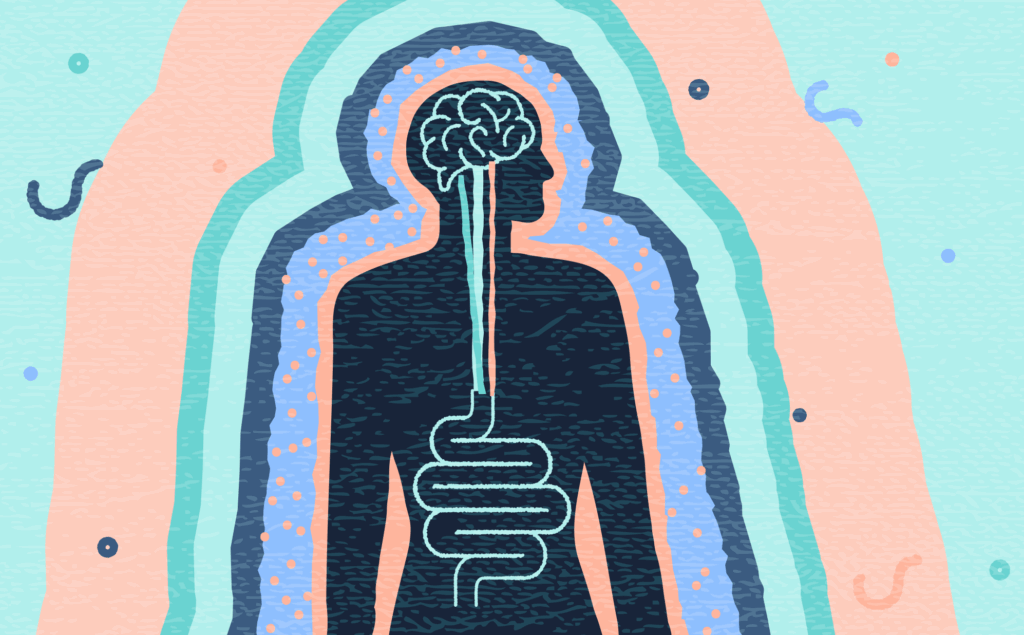
“There are basically two mechanisms that cause nausea. One is due to slowed gastric emptying. GLP1s delay gastric emptying which causes food to sit in the stomach for longer periods of time, which triggers nausea,” says Micheal Currier, PA-C, “The other mechanism resides in the central nervous system and is due to how the medication activates GLP-1 receptors in the area of the brain that controls nausea and vomiting, which then leads to an increase in nausea.”
How common is nausea on GLP-1 drugs?
In one study, 42.23% of those on GLP-1 drugs reported nausea and 21.90% reported vomiting. Another meta-analysis, which looked at relevant data from multiple clinical studies, estimated that 40-70% of people on GLP-1 drugs will experience nausea at some point while taking the medication.
Tirzepatide, followed by semaglutide, is the most likely to cause nausea and vomiting. The meta-analysis further broke down how common nausea is for the five FDA-approved GLP-1 drug types, and another study looked at tirzepatide’s rate:
- Dulaglutide: 5-29%
- Exenatide: 5-59%
- Liraglutide: 10-48%
- Lixisenatide: 16-40%
- Semaglutide: 8-58%
- Tirzepatide: 20.43%
You’ll notice that these percentages vary quite a bit. That’s because a variety of factors can impact if, and which, side effects someone may experience. These could include an individual’s genetics, current health status, GLP-1 dose, and other medications they take.
Strategies to manage GLP-1 nausea
Experiencing nausea doesn’t mean you have to stop taking your medication. It does mean you should discuss the symptom with a healthcare provider, who can assess how severe the nausea is and suggest ways to manage it.
Work on eating habits
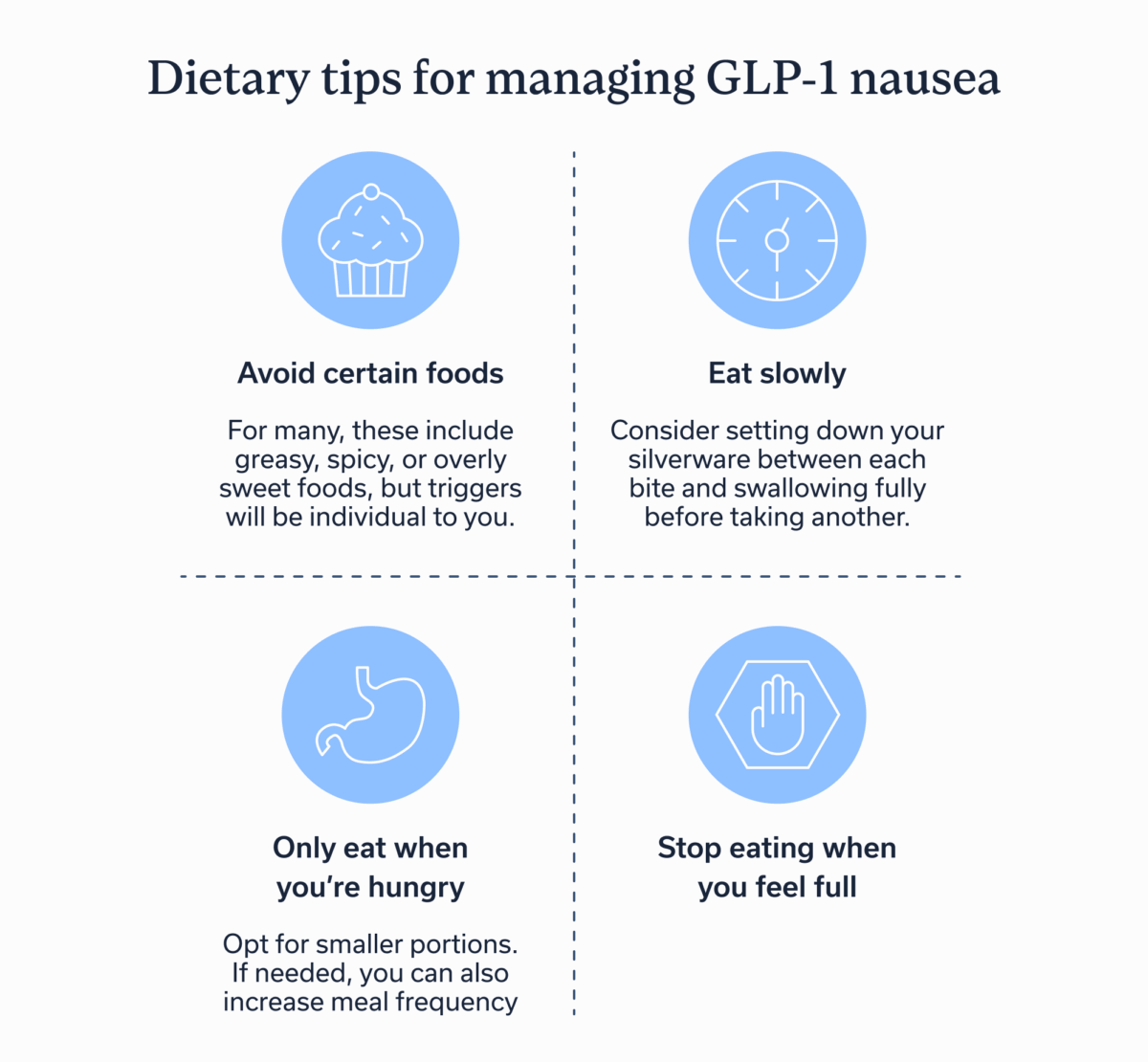
GLP-1s work best alongside a healthy diet and regular exercise—and “work best” means minimal to no nausea. Researchers have developed specific dietary guidelines to avoid GLP-1 nausea, including:
- Avoid trigger foods. For many, these include greasy, spicy, or overly sweet foods, but triggers will be individual to you.
- Eat slowly—consider setting down your silverware between each bite and swallowing fully before taking another.
- Opt for smaller portions and increase meal frequency if needed.
- Stop eating when you feel full.
To discover what foods or eating habits trigger GLP-1 nausea, you can keep a food log where you document what you eat, when and how much you eat, and how you feel after. This food journal can also be helpful to your healthcare providers, who can use food logs to help you identify what eating habits are leading to nausea.
Stay upright after eating
“Staying upright for at least 30 minutes after eating is very helpful to avoid nausea because it more easily allows the food to pass through the stomach using gravity,” says Currier. “By lying down, it causes the food to stay in the stomach longer, which will trigger more nausea and acid reflux.”
Admittedly, it’s all too easy to watch Netflix in bed after eating dinner. But scheduling a short walk in the evening or investing in a standing desk for your post-lunch work sessions can help you avoid GLP-1 nausea.
Hydrate wisely
Drinking fluids between meals instead of with them may help with nausea. Ideally, it’s best to drink any liquids 30-60 minutes before or after meals when taking a GLP-1 drug.
Use of anti-nausea remedies
Depending on the severity of the nausea, a healthcare provider may recommend over-the-counter medications or even prescription anti-emetics like Zofran to relieve symptoms. Other anti-nausea remedies, such as ginger or peppermint tea or anti-nausea
Run any anti-nausea remedies by a healthcare provider before using them. Your provider can check to ensure that remedies won’t cause adverse effects specific to the GLP-1 you’re taking.
Timing and dosage adjustments
Most of us have been prescribed a medication at one time or another that starts and finishes at the same dose. Although the majority of medications work this way, GLP-1s don’t. Instead, they fall into the “titration” camp.
Titration, the process of slowly increasing dosage over time and only when the medication is well-tolerated, helps manage GLP-1 side effects. “Slowly increasing the dose of a GLP-1 medication allows the body time to adjust to the changes that are occurring, especially the slowing of gastric motility,” says Currier, “So the key to avoiding the nausea as much as possible is to take the titration phase slowly and allow the body time to acclimate appropriately.” If someone increases the dose too quickly or overdoses, they’re more likely to experience severe nausea.
But don’t panic about figuring out the right dose; your provider will follow the appropriate clinical protocols to start you at the lowest dose and move up as needed. They can advise you on the right dosage schedule, address GLP-1 nausea or any other side effects that come up, and help you stay motivated during titration.
When to talk to a healthcare provider
Only take GLP-1s alongside the guidance of a healthcare provider, and with regular touchpoints where you can talk to that provider about your symptoms. If you’re experiencing any nausea, let them know so they can adjust your medication dose or recommend alternative treatments if necessary.
See a healthcare provider immediately if you experience:
- An inability to eat
- Persistent or severe nausea that impacts your daily life
- Signs of dehydration (extreme thirst, dizziness, dry mouth, peeing less often)
If your nausea is severe, consult with your prescribing physician or your GI team. Missing doses or taking a lower dose than prescribed decreases the efficacy of these medications. That isn’t to say you can’t (or shouldn’t) stop taking these medications if your side effects are severe. Just don’t stop them on your own. Your provider can evaluate your specific situation and recommend a safe transition plan to a different type of GLP-1 or an alternative strategy.
While clinically effective, GLP-1s are complicated. Results sometimes occur slower than you may expect, increasing your dosage safely can be confusing, and even choosing between the many FDA-approved GLP-1s can prove challenging. That’s why a healthcare provider’s guidance is crucial.
Working with a provider whose background is in gastrointestinal health can be particularly beneficial, since many of GLP-1s benefits and side effects affect the digestive tract. The multidisciplinary team of GI providers, gut-brain specialists, and registered dietitians at Oshi Health can offer a tailored treatment plan to help you implement the lifestyle and behavioral adjustments needed to reduce GI side effects associated with GLP-1 drugs.
Key Takeaways
- GLP-1 nausea is common but manageable with the right strategies.
- Some of the best strategies include changing your eating habits, hydrating wisely, staying upright after eating, using anti-nausea remedies, and following a titration schedule.
- For support managing GLP-1 side effects and staying on track with your blood sugar or weight management goals, consider working with a GI provider, such as the team at Oshi Health.
Frequently asked questions (FAQs)
-
GLP-1 nausea can be a persistent side effect, or can go away less than an hour after eating. The exact duration depends on the individual, the type and dose of medication they take, and how quickly they increase their GLP-1 dose.
-
Some of the most effective ways to stop nausea on Ozempic are, as mentioned above: to hydrate between (not during) meals, to stay upright after eating, and to follow a healthcare provider’s timeline to increase dosage. Many also find it useful to develop certain eating habits, such as not eating when full and eating smaller meals more frequently.
-
Any GLP-1 medication might make you feel nauseous. That said, nausea is most commonly reported for semaglutide and least commonly reported for dulaglutide.
-
As discussed earlier, getting rid of GLP-1 nausea often boils down to: changing your eating habits, using anti-nausea remedies like over-the-counter medications or peppermint tea, hydrating between (not during) meals, and staying upright after eating. If you’re experiencing severe nausea accompanied by dehydration or an inability to eat, contact emergency health services.
Take charge of your gut health on GLP-1 medications with expert dietary support
If you’re taking a GLP-1 medication and experiencing side effects like nausea or digestive discomfort, you’re not alone. Our team of GI-specialized, registered dietitians is here to help.
Your nutrition plays an important role in how you feel day to day, especially when adjusting to a new medication. Oshi dietitians can work with you to:
✔ Ensure you stay nourished and offer practical tips for navigating common GLP-1 side effects
✔ Build personalized meal plans that fit your lifestyle and medication schedule
✔ Guide you through small, sustainable changes to help you feel your best
✔ And so much more!
Ready to make mealtimes less stressful and feel in control again?