Have you ever wondered if you might have a gastrointestinal (GI) disease? If so, you’re not alone. GI conditions are quite common, and gastrointestinal symptoms such as heartburn, stomach pain, and abnormal bowel movements are even more common. The good news is gastrointestinal disease treatments are available and often effective—once you figure out which condition affects your GI tract.
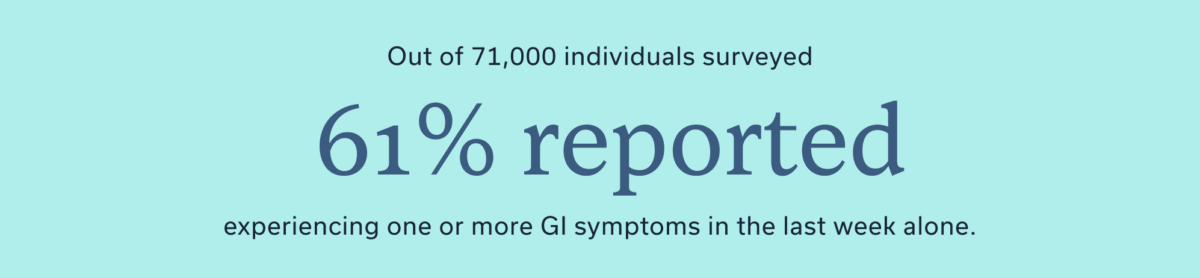
We all experience an upset stomach or bloating from time to time. In one study polling over 71,000 individuals, 61% reported experiencing one or more GI symptoms in the last week alone, and 25% of people live with a diagnosed GI condition. Gastrointestinal (GI) symptoms remind us that our digestive tract is crucial to overall health—and that effective GI treatment options are life-savers (often literally!). To help find the right treatments, we compiled a list of the 10 most common GI conditions and effective gastrointestinal disease treatments for each.
Understanding gastrointestinal (GI) diseases
“The term gastrointestinal disease refers to disorders that impact the digestive system,” says Elwood Martin, MD, a surgeon who specializes in GI disease. All GI diseases affect the digestive process, which is how the body absorbs crucial nutrients from food and liquids and gets rid of waste in the form of stool. Their effects vary quite a bit. Dr. Martin explains, “The disorders can range from mild with minimal symptoms to more severe, debilitating symptoms with significant impact on quality of life.”
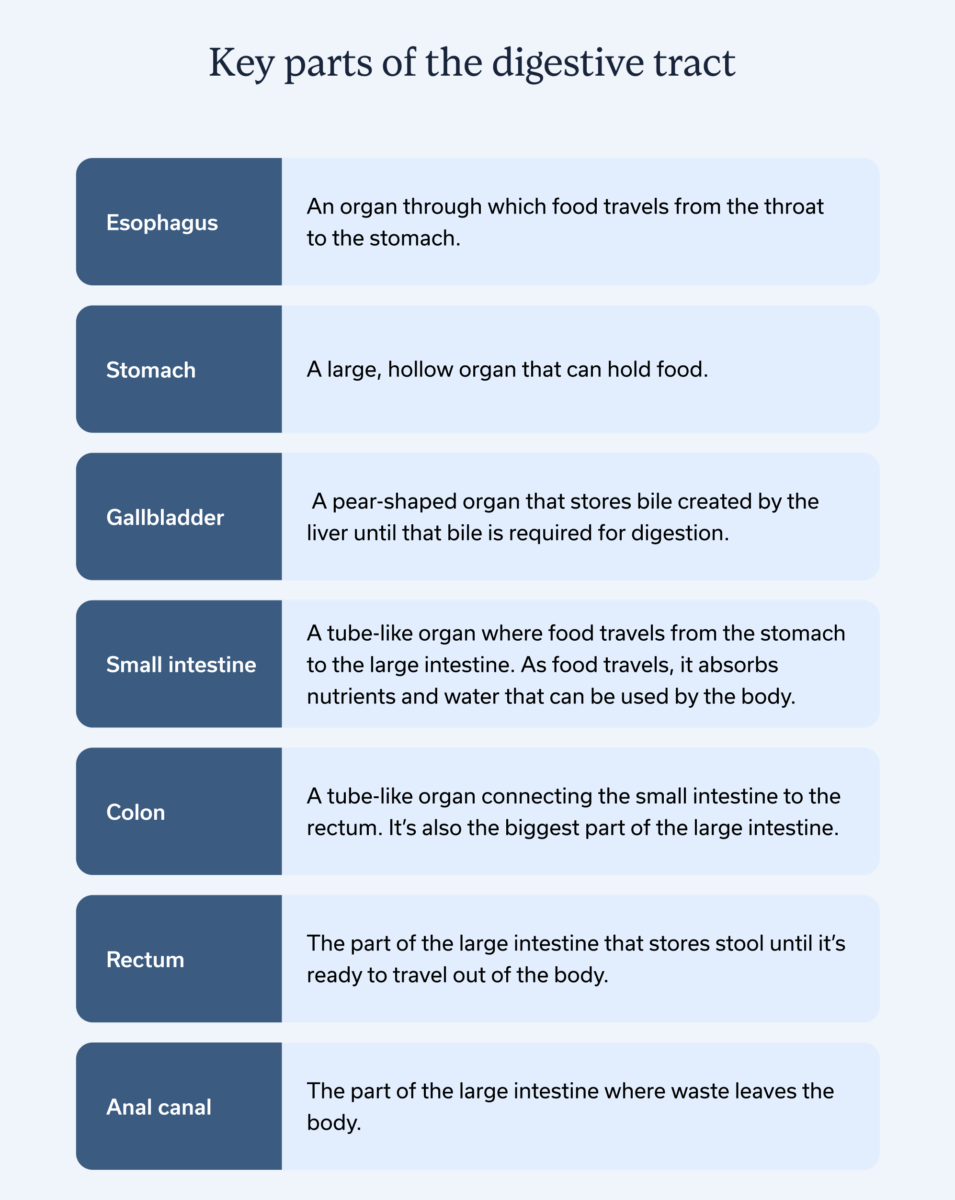
Key parts of the digestive tract
When it comes to common GI diseases, there’s a few key players in the digestive tract that may be affected:
- Esophagus: An organ through which food travels from the throat to the stomach.
- Stomach: A large, hollow organ that holds food.
- Gallbladder: A pear-shaped organ that stores bile created by the liver until that bile is required for digestion.
- Small intestine: A tube-like organ where food travels from the stomach to the large intestine. As food travels, it absorbs nutrients and water that can be used by the body.
- Colon: A tube-like organ connecting the small intestine to the rectum. It’s also the biggest part of the large intestine.
- Rectum: The part of the large intestine that stores stool until it’s ready to travel out of the body.
- Anal canal: The part of the large intestine where waste leaves the body.
GI conditions affect one or a few parts of the GI tract and can range from short-term to longer, chronic conditions.
The 10 most common gastrointestinal diseases and their treatments
Gastrointestinal diseases are common. While GI symptoms do sometimes stem from acute causes, like the flu or food poisoning, the ten diseases listed below are the most common culprits (in alphabetical order) for chronic or ongoing GI symptoms.
1. Celiac disease
Celiac disease is when the small intestine cannot process gluten. If someone with celiac disease eats something with gluten (i.e. breads, baked goods, and many cereals), it triggers an immune response which damages the small intestine.
The damage celiac disease causes prevents the small intestine from doing its job: absorbing nutrients, vitamins, and minerals from food. This malabsorption results in GI symptoms like bloating, diarrhea, constipation, nausea, and abdominal pain, as well as symptoms outside the GI tract, like fatigue, anemia (iron deficiency), and joint pain.
To treat Celiac disease, a gastroenterologist or GI registered dietitian (RD) will recommend a gluten-free diet. Many who follow a gluten-free diet experience fewer symptoms and avoid further small intestine damage. About 7-30% of people with Celiac disease will still experience symptoms on the gluten-free diet, and a GI provider can help create a customized treatment plan when this is the case.
2. Constipation
In any given year, about 16% of Americans will experience constipation, which is the feeling of needing to poop but not being able to. Not being regular comes with some pretty uncomfortable side effects: bloating, hard or lumpy stools, abdominal pain, and pain when trying to poop.
With constipation, the number to remember is three. Someone has constipation when they have fewer than three bowel movements a week, and constipation is considered chronic when it persists for three months or longer.
To treat constipation, a healthcare provider will likely recommend staying hydrated, regular exercise, and increasing dietary fiber. When constipation is chronic, they’ll also look for, and treat, any underlying conditions.
3. Diarrhea and gastroenteritis
If someone has frequent loose or watery bowel movements, nausea, vomiting, and abdominal pain, they may be experiencing diarrhea or gastroenteritis, aka the stomach flu. While most of us have experienced one or the other at some point, 20.2% of Americans will experience diarrhea annually and 1 out of every 15 people get gastroenteritis each year.
Treatment depends on what’s causing symptoms. If viral or in reaction to food or a medication, symptoms will probably disappear on their own, though staying hydrated and resting may help. For bacterial or parasitic causes, medication will probably be prescribed.
When chronic, diarrhea may point to an underlying condition, such as inflammatory bowel disease or a persistent infection. When this is the case, a GI provider may create an appropriate treatment plan, likely involving dietary changes, probiotics, medications, and working with a gut-brain specialist.
4. Diverticular disease
Diverticular disease, aka diverticulosis (when small pouches form in the lower digestive tract) or diverticulitis (when that small pouch becomes inflamed or infected), mainly in the colon wall. They push out of the colon wall, resulting in symptoms like lower abdominal pain, rectal bleeding, bloating, and changes in bowel movements, usually constipation.
It’s more common as we age, and over 30% of those over 45 have experienced it. The likelihood of diverticulosis increases with age. Plus, symptoms can be quite serious—the disease is responsible for 300,000 hospitalizations each year.
Treatment often involves medication, such as antibiotics, aspirin, or naproxen, and adopting a high-fiber diet. Fiber helps soften stool and may relieve pressure on the colon wall. That said, if someone currently has diverticulosis they should adopt a high fiber diet slowly, ideally under the guidance of a registered dietitian with specialized GI training.
5. Gallstones
The gallbladder is part of the GI tract most of us don’t think about very often, unless we have symptomatic gallstones. Gallstones are hard deposits ranging from the size of a grain of sand to a golf ball. They may block the tube from which bile leaves the gallbladder. About 6% of people globally have gallstones, and it’s more common in women than men.
Many gallstones are asymptomatic, though if a large stone blocks the entirety of the tube, they cause abdominal cramping and pain in the upper right abdomen. When the gallstone travels to the small intestine, symptoms disappear. While some painful gallstones pass through on their own, surgery or medication may be required.
6. Gastroesophageal reflux disease (GERD)
About 20% of Americans have GERD, a chronic condition where the stomach contents regularly travel back into the esophagus and sometimes the throat, causing a chest pain we refer to as heartburn. Alongside heartburn, GERD may also cause nausea, difficulty swallowing, pain when swallowing, and loss of appetite.
A weak esophageal sphincter, the part of the GI tract that lets food flow from the esophagus, causes GERD. You can think of this sphincter like a club bouncer for the stomach. If that bouncer slacks on the job (i.e. the sphincter weakens), food may travel the wrong way, causing acid reflux (aka heartburn)—and GERD when that heartburn becomes chronic.
“Medical management focuses on minimizing symptoms, as there is no medical cure for GERD,” says Dr. Martin. He adds that both over-the-counter and prescription medications may be recommended to soothe current symptoms.
“Other medical management strategies include lifestyle and diet modifications,” says Dr. Martin, “These modifications may include maintaining a healthy weight, smoking cessation, elevating the head of the bed, sleeping on the patient’s left side, not lying down for 3-4 hours after the last meal, not eating after 6 PM, and wearing loose clothing. Beneficial eating habits include taking small bites, chewing the food well, eating smaller meals, and avoiding consumption of foods or beverages that trigger symptoms.”
7. Hemorrhoids
About 5% of Americans have hemorrhoids, though they become more common with age. 50% of those over 50 experience these swollen veins around the anus and lower region of the rectum at least once. These swollen, often inflamed, veins result in itching and pain in the anal and rectal region, as well as possible rectal bleeding.
There’s many potential causes for hemorrhoids, including weakening of anus and rectal tissues due to aging or pregnancy, strained bowel movements, and chronic constipation or diarrhea.
Hemorrhoids can be treated at home with stool softeners, staying hydrated, increasing fiber intake, and using over-the-counter creams or pain relievers. A GI provider can provide guidance to quicken recovery and can assess if hemorrhoids are severe enough to require surgery or a more minimally-invasive procedure.
8. Irritable bowel syndrome (IBS)
IBS is a common chronic condition that disrupts daily life. When someone has IBS, the colon and small intestine become more sensitive to normal GI functions, such as contractions or passing gas.
That hypersensitivity leads to symptoms like abdominal pain and abnormal bowel movements. There’s three different types of IBS: IBS-C, marked by chronic constipation, IBS-D, marked by chronic diarrhea, and IBS-M, when someone has a mix of chronic diarrhea and constipation.
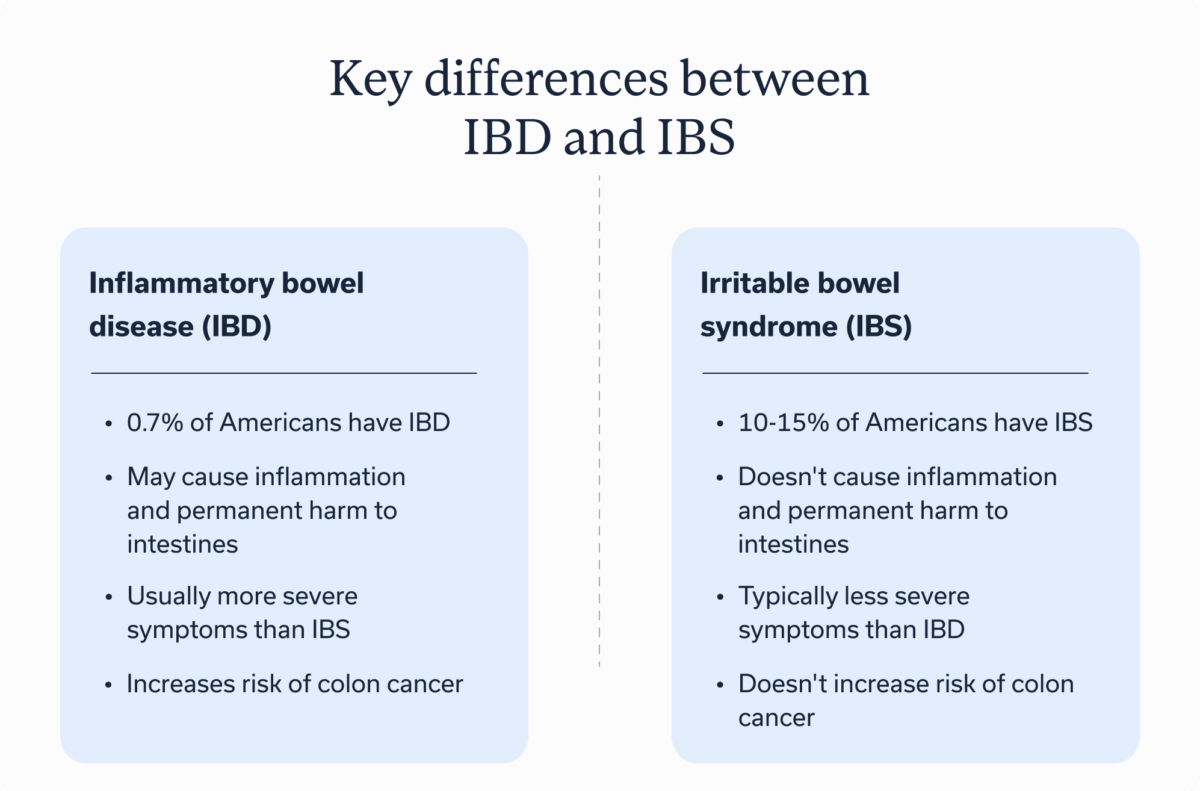
About 10-15% of Americans have IBS, and women are twice as likely as men to develop it. Treatment options include medications, supplements, a mix of dietary adjustments, and GI behavioral health treatment with a gut-brain specialist.
9. Inflammatory bowel disease (IBD): Crohn’s disease & ulcerative colitis
IBD is an autoimmune disease that affects the intestines and bowels. The two most common are:
- Crohn’s disease: Chronic inflammation that can impact any part of the GI tract but is most common in the small intestine.
- Ulcerative colitis: When there’s chronic inflammation and ulcers in the colon and large intestine’s lining.
Common symptoms of IBD include abdominal pain, chronic diarrhea, stomach pain, fatigue, weight loss, and nausea. And while those symptoms—and the name—sound similar to IBS, there’s a few key differences:
- IBD is marked by inflammation and structural damage to the intestines (IBS causes neither)
- IBD often has a higher risk of hospitalization
- IBD increases the risk of colon cancer while IBS does not
- IBD is also less common, with around 0.7% of Americans having an IBD diagnosis, though people can have IBS and IBD overlap
Treatment varies depending on IBD type, though common treatments include medications, dietary changes to stay well nourished and reduce future flares, and working with a GI specialist to improve the gut-brain connection. In more severe cases, surgery may be recommended.
10. Peptic ulcers
5-10% of Americans will have peptic ulcers at some point in their lives. Also referred to as a stomach ulcer or simply an ulcer, peptic ulcers are sores on the small intestine. The most common symptom is a burning stomach pain, especially between meals or when stressed.
There are various causes for ulcers, though the most common are nonsteroidal anti-inflammatory drugs (NSAIDs) and other medications and H. pylori infections. H. pylori is a type of bacteria that can be treated by antibiotics, as well as acid-blocking medications in some cases. If ulcers are caused by NSAIDs or another medication, treatment involves stopping medication and finding alternative treatment.
When to see a healthcare provider
Whenever GI symptoms are ongoing and unexplained, it’s best to make an appointment with a gastroenterologist or other GI provider. They can assess symptoms, provide an accurate diagnosis, and create a customized treatment plan.
Symptoms that indicate it’s time to book an appointment with a GI provider include:
- Abdominal pain
- Bloating
- Bloody stool
- Constipation
- Diarrhea
- Difficulty passing gas
- Heartburn
- Chronic nausea or vomiting
When looking for a healthcare provider, Dr. Martin says it’s best to work with a collaborative team with a multidisciplinary approach. He explains, “A well-informed patient being cared for by experienced experts should result in the best patient outcomes and have the least financial impact.”
Key takeaways
- Gastrointestinal diseases are conditions in the esophagus, stomach, small intestine, colon, and rectum that cause uncomfortable GI symptoms.
- The most common chronic GI conditions include celiac disease, chronic constipation, chronic diarrhea, diverticular disease, gallstones, GERD, hemorrhoids, IBS, IBD, and peptic ulcers.
- If experiencing persistent, painful, or unexplained GI symptoms, consult a GI provider like Oshi Health. They can provide an accurate diagnosis and create a treatment plan.
Frequently asked questions (FAQs)
-
The right treatment for gastrointestinal disease depends on the specific condition and individual. That said, treatment often involves dietary changes, living a more active lifestyle, GI-focused therapy, and taking appropriate medications.
-
Some gastrointestinal diseases can be treated at home through a mix of over-the-counter medications, rest, hydration, and dietary changes. If symptoms are ongoing or extremely painful, it’s best to consult a healthcare provider on the best treatment options.
-
Solving stomach problems is nuanced, since there are many GI conditions that could be to blame. For comprehensive guidance, reach out to a GI provider, such as a gastroenterologist, who can provide treatments specific to your stomach problems.
Oshi is your partner in digestive health
Feel like your digestive concerns are running your life? You’re not alone—and we’re here to help you find lasting relief.
Oshi Health GI providers, gut-brain specialists, and registered dietitians work together to address your symptoms and find solutions that actually work for you.
Whether you’re dealing with chronic digestive issues or unpredictable symptom flare-ups, our GI specialists deliver:
✔ Personalized care plans tailored to your lifestyle
✔ Science-backed strategies to calm your gut
✔ Compassionate, whole-person care
✔ And so much more!
Ready to take control of your gut health?