Most of us have experienced periods of time when our digestion wasn’t quite regular, whether it was from a dessert-filled vacation or a busy work week where we didn’t drink enough water. But if that pushing-to-poop feeling becomes a constant, it’s referred to as chronic constipation—and probably requires a treatment plan to get things moving again.
The feeling of needing to poop but not being able to is constipation, and most of us experience it at one time or another. In most cases, constipation resolves quickly with minimal treatment or intervention. But if it becomes a constant, you might be diagnosed with chronic constipation.
“Chronic constipation is where a person experiences hard defecation that continues for weeks,” says board-certified gastroenterologist Peyton Berookim, MD, MA, FACG, AGAF. “It is usually diagnosed if the symptoms persist for three months or longer.” There’s a lot to unpack with chronic constipation, from symptoms to causes to effective treatment options. Here’s what you need to know to make sense of it.
Symptoms of chronic constipation
Constipation, chronic or otherwise, is marked by four key symptoms:
- Feeling like not all your stool has passed, even right after a bowel movement
- Hard or lumpy stools
- Less than three bowel movements a week
- Pain or difficulty passing stools
Some people also report stomach pain or feeling bloated when constipated.
Recognizing constipation danger signs
Not passing regular bowel movements sounds uncomfortable, but when chronic, it can also be dangerous. Make an appointment with your PCP if you have:
- Chronic constipation lasting longer than three weeks
- Mild or moderate abdominal pain
- Changes in bowel habits
- Incomplete emptying with bowel movements
- Reduced appetite
- Weight loss without trying
- A small amount of blood in stool
- Persistent cramps
- Nausea or vomiting
Head to urgent care or the emergency room if you have:
- Significant blood in stool
- Fever and abdominal symptoms
- Inability to pass gas or stool
- Rectal bleeding
- Severe lower back pain
- Severe, constant abdominal pain
- Frequent nausea
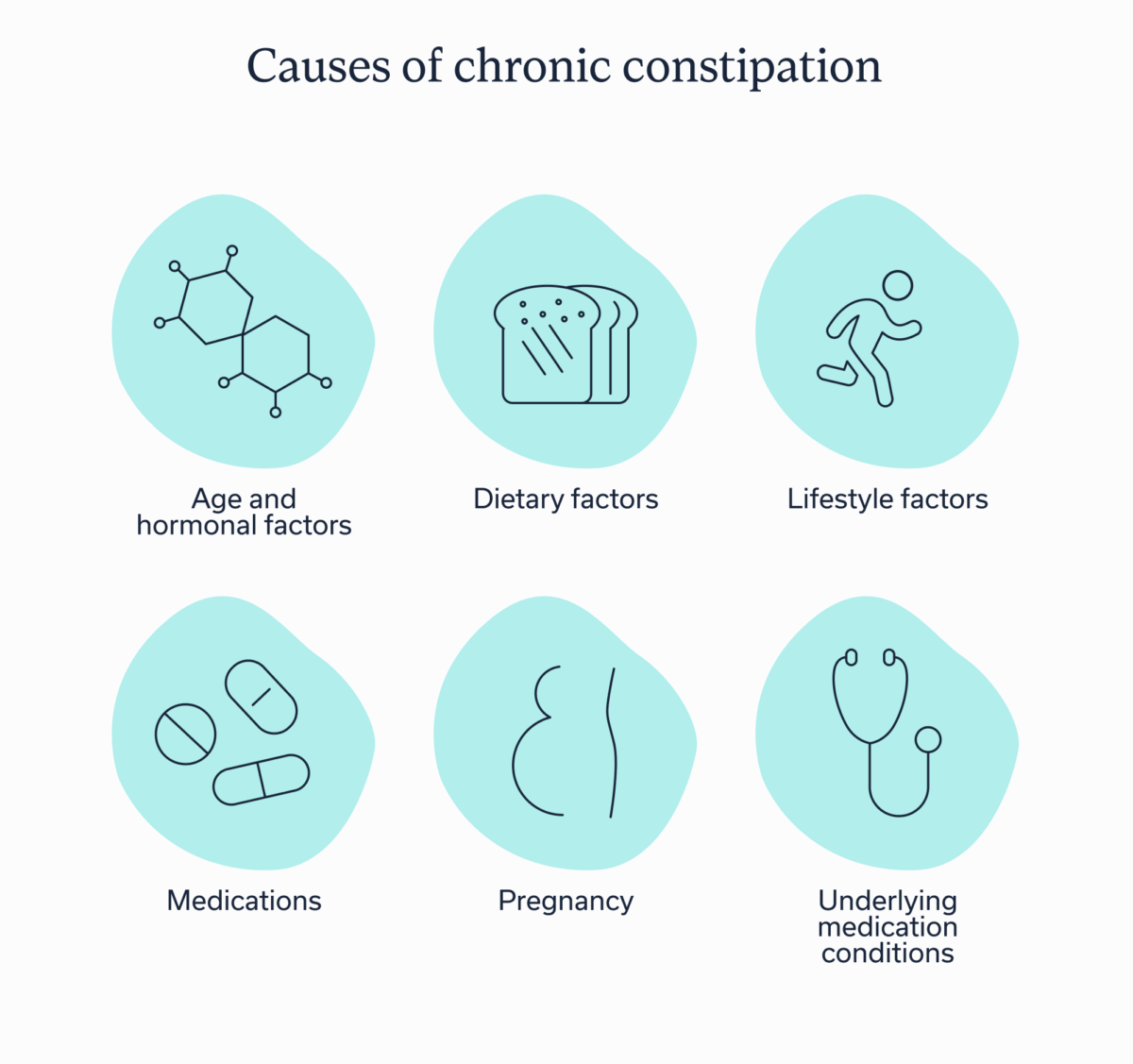
Causes of chronic constipation
There’s a laundry list of potential reasons why stool may move slowly through the colon for three or more months, with the most common being:
- Age and hormonal factors: As we age, the risk of chronic constipation increases. Certain hormonal changes, such as the menopausal transition, can also slow down metabolism, increasing the risk.
- Dietary factors: What you eat and drink impacts your bowel movements. Dehydration, low fiber intake, and a diet high in processed foods can all contribute to chronic constipation.
- Lifestyle factors: A lack of physical activity and/or a sedentary lifestyle slows down the bowels, potentially contributing to constipation.
- Medications: Opioids, certain antidepressants, iron supplements, some weight management drugs, and other medications may slow down the movement of stool through the colon.
- Pregnancy: Pregnancy constipation is all too real. Globally, about 21.1% of pregnant people experience constipation during the first trimester, 34% during the second, and 30.3% during the third.
- Underlying medical conditions: Constipation is a symptom of many medical conditions. These include irritable bowel syndrome (IBS), inflammatory bowel disease (IBD), volvulus (which is when the intestine wraps around the bowel and causes bowel obstruction), an underactive thyroid (hypothyroidism), pelvic floor disorders, and diabetes.
Often, chronic constipation is due to a mix of causes. A pregnant person experiencing constipation, for example, could also have gestational diabetes or lead an inactive lifestyle. Someone with IBS who experiences constipation may also not eat enough fiber and be entering perimenopause. Because of the various potential causes, it’s often best to work with a GI provider who uses a whole person approach to diagnose and treat the cause(s).
Effects of chronic constipation on the body
“Chronic constipation can have several consequences on the body beyond making it difficult to pass stools,” says Dr. Berookim. The most common complications include:
- Anal fissures: Anal pain and bleeding may occur when someone tries to pass hard or oversized stool, which is more common when constipated.
- Fecal impaction: “Severe constipation can lead to a hard mass of stool clogging up the rectum or colon,” says Dr. Berookim, “On occasion, this requires manual removal or medical intervention.
- Heartburn: “One of the most common causes of heartburn is constipation,” says Dr. Berookim, “Many patients are on anti-acid medications such as proton pump inhibitors (PPI’s) for what is believed to be heartburn. A lot of these patients are in fact constipated and treating their constipation can alleviate their heartburn.”
- Hemorrhoids: Strained bowel movements can compress veins around the anus, increasing the risk of hemorrhoids.
- Rectal prolapse: “Long-term straining can cause the rectum to protrude part-way out the anus,” says Dr. Berookim.
- Urinary problems: “A full rectum may press on the bladder, leading to more frequent urination, urgency, or even urinary retention,” explains Dr. Berookim.
Chronic constipation may also lead to a poorer quality of life, thanks to these potential complications and the discomfort and stress of not being able to go regularly. Plus, not being able to go regularly can have a ripple effect on your mental health. In a 2022 study, 30.3% of constipated people also had depression and 21.3% had anxiety.Why? Research suggests mental distress increases the chance of constipation, and constipation increases the likelihood of mental distress, creating a vicious cycle.
When to consult a healthcare professional
Unless you already see a gastroenterologist, you’ll most likely make an appointment with a primary care provider for chronic constipation, who may refer you to a gastrointestinal specialist if symptoms are chronic or not responding to conservative treatment, like lifestyle modifications or over-the-counter medications.
Effective treatments for chronic constipation
“Effectively managing chronic constipation generally starts with modifications to diet and lifestyle,” says Dr. Berookim. When this doesn’t work, medications, both prescription or over-the-counter, or in rare cases surgery may be recommended.
Dietary changes
Changing what you eat and drink is often the frontline defense against constipation but that doesn’t necessarily mean you need to follow a highly restrictive diet. You can think of this as more of a game of addition rather than subtraction. Instead, there’s a trio of dietary changes that can help your stool movements become more regular:
- Increase fiber intake: The recommended fiber intake is 22 to 34 grams daily, with the exact amount depending on age and sex. High fiber foods include most fruits and veggies, nuts, legumes, like beans and chickpeas, and whole grains, such as whole wheat pasta and oatmeal.
- Stay hydrated: Fiber often works better when paired with adequate liquid to keep it moving. Ideally that liquid should be water, fruit juice that’s naturally sweetened, or clear soups. While there’s a common myth that we should be drinking 64 ounces of water a day, the actual recommended amount depends on age, sex, breastfeeding status, and activity level.
- Avoid certain foods: It may be helpful to reduce processed foods or prepared foods, like hot dogs and frozen dinners, or excessive dairy and meats. Foods with minimal fiber (think: chips, fast food, baked goods) are best consumed in moderation.
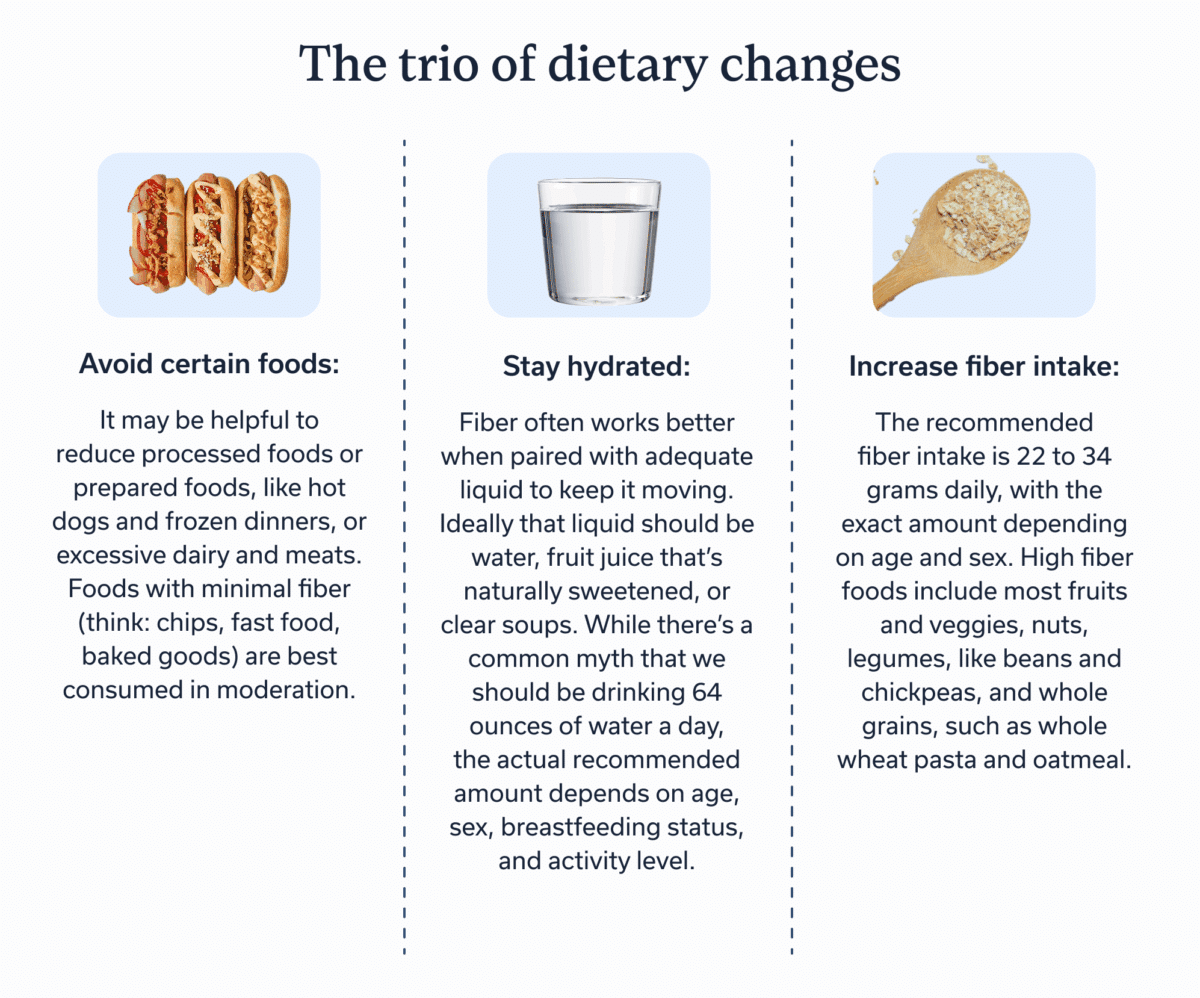
There are exceptions to this dietary trio. Those with gastrointestinal conditions like IBS or IBD often respond differently to fiber, making it important to work with a registered dietitian who specializes in GI conditions to determine what types of fiber your body can tolerate and how much to consume.
Get moving
Physical activity gets all parts of your body moving, including the bowels. This doesn’t mean you have to sign-up for a half-marathon or start an intense CrossFit class to treat chronic constipation (but more power to you if you want to). It does mean you should aim to meet recommended exercise guidelines: two strength training sessions a week and 150 minutes of moderate aerobic activity, like a brisk walk, or 75 minutes of more intense aerobic activity, like a run or swim. These are minimums, meaning you can exceed these guidelines too.
Bowel training
Another lifestyle change that may help treat chronic constipation is bowel training, which consists of:
- Establishing a daily time for a bowel movement, ideally 20 to 40 minutes after a meal
- GI-focused therapy to address any emotional reasons for chronic constipation
- Adopting a proper toileting position
Many people can successfully retrain their bowels within a few weeks. That said, consulting a GI specialist often makes training more effective, similar to how a personal trainer provides clarity and faster progress at the gym.
Over-the-counter (OTC) treatments
When lifestyle modifications aren’t working, medications are often the next option. “Meds are also appropriate if the constipation is causing severe discomfort or complications,” says Dr. Berookim.
Common over-the-counter medications include:
- Fiber supplements
- Laxatives
- Stool softeners
While you can drive to the pharmacy and get over-the-counter medications without a prescription, this may not be the best idea. Instead, discuss potential side effects, interactions with other medication you’re taking, and which of the three is the best option with a GI provider before visiting the pharmacy.
Prescription medications
When constipation is more severe or part of an underlying medical condition, a clinician may prescribe a stronger or more targeted medication, such as:
- Lubiprostone: A medication that increases fluid in the dietary tract
- Linaclotide or plecanatide: Two common IBS-C medications to make bowel movements more regular
- Opioid antagonists: Prescribed when opioid use causes constipation
- Prucalopride: A medication to help the colon move stool faster. It’s often prescribed when there’s long lasting constipation but no known cause.
These medications are all prescription drugs, meaning a GI or primary care provider must write a prescription in order for a pharmacy to provide you with any of the above.
Preventing chronic constipation
We can all take steps to prevent chronic constipation, regardless of age or our medical history. Many are the same as the front-line treatment options:
- Develop a consistent bowel movement routine
- Eat a balanced diet that meets fiber intake recommendations
- Exercise regularly
- Stay hydrated
If someone is at a higher risk due to age, a medical condition, or another factor, regular check-ups with a GI provider are another preventative measure. Those with certain conditions, like IBS or IBD, may also prevent chronic constipation by treating the underlying condition.
Key takeaways
- Chronic constipation occurs when someone experiences difficulty passing stool for three or more months.
- Lifestyle factors, such as diet and activity level, as well as various medical conditions can cause chronic constipation. A GI provider, including those at Oshi Health, can diagnose and treat any underlying conditions.
- Adopting a high-fiber diet, staying hydrated, exercising regularly, and bowel training can treat chronic constipation—and prevent future occurrences.
Frequently asked questions (FAQs)
-
For most, eating more fiber, staying hydrated, consuming fewer processed foods, exercising regularly, and having a set time for bowel movements helps fix chronic constipation. When these don’t work, a doctor may recommend medication or, in rare cases, surgery.
-
If constipated all the time, it could be due to not getting enough fiber in your diet, dehydration, age-related changes, or a number of medical conditions, including IBS, hypothyroidism, or IBD. Pregnancy also increases the likelihood of constipation.
-
Chronic constipation can lead to a number of complications, including heartburn, hemorrhoids, and anal fissures. It can also impact mental health, decrease appetite, and reduce overall quality of life.
-
If you’re still constipated after eating fiber and drinking water, an underlying medical condition may be to blame. Visit a primary care provider or GI provider who can run diagnostic tests and provide a diagnosis and treatment plan.
-
Chronic constipation often decreases someone’s overall quality of life. However, it’s usually treatable and someone with chronic constipation can lead a normal life, especially after following a treatment plan created by a GI provider.
Oshi is your partner in digestive health
Feel like your digestive concerns are running your life? You’re not alone—and we’re here to help you find lasting relief.
Oshi Health GI providers, gut-brain specialists, and registered dietitians work together to address your symptoms and find solutions that actually work for you.
Whether you’re dealing with chronic digestive issues or unpredictable symptom flare-ups, our GI specialists deliver:
✔ Personalized care plans tailored to your lifestyle
✔ Science-backed strategies to calm your gut
✔ Compassionate, whole-person care
✔ And so much more!
Ready to take control of your gut health?