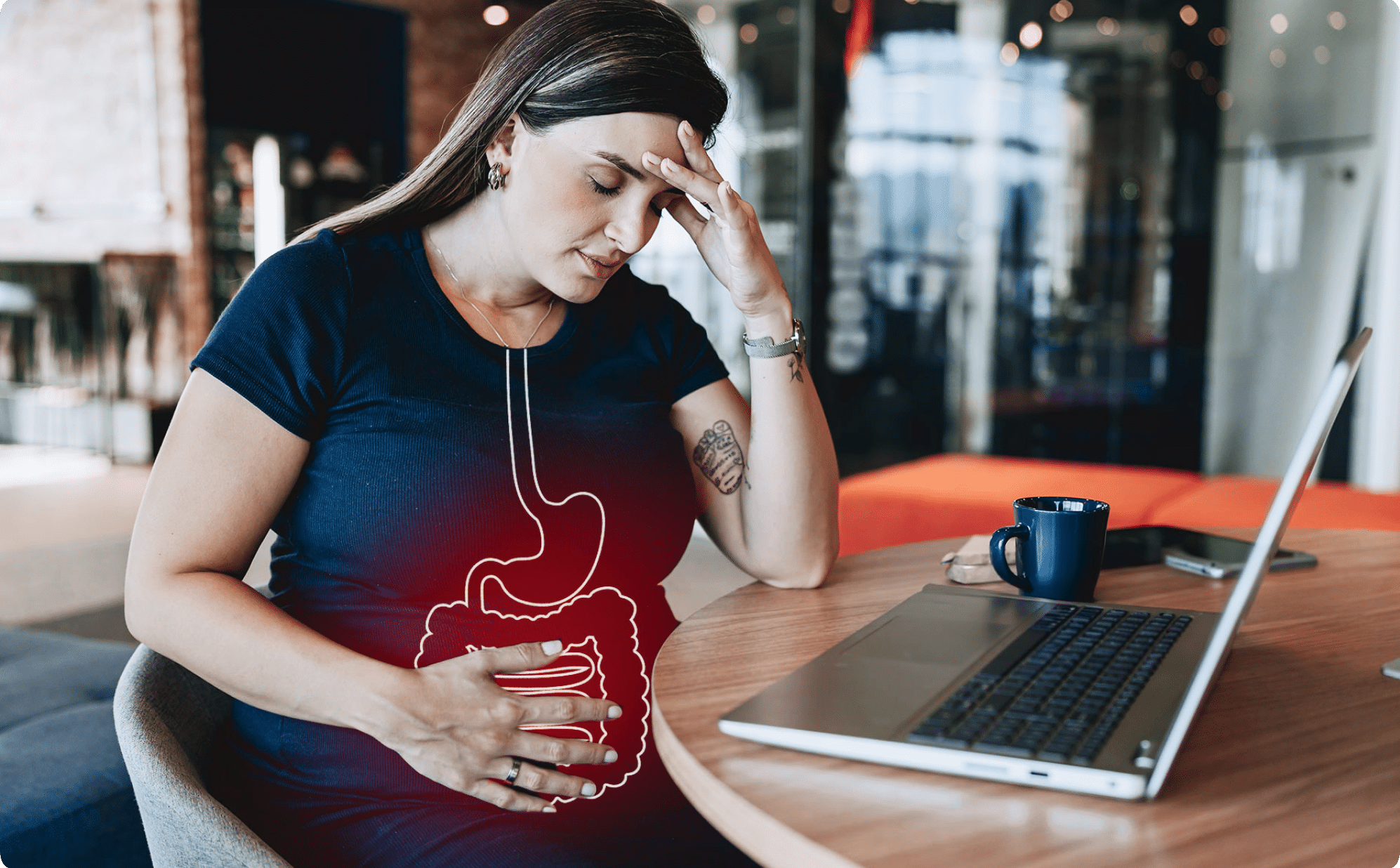
When you’re stressed, it may have an impact on your gut health. But can stress actually cause diarrhea? Yes, while the two may seem unrelated, stress can indeed cause diarrhea, due to the gut-brain connection. And if it’s chronic, that stress may also lead to more serious GI conditions where diarrhea becomes a recurring symptom.
Maybe it’s been a stressful few weeks, and you’re experiencing tension in your body, excessive worrying, and a lack of energy. At the same time, your poop is also a bit too frequent, loose, and watery (aka you have diarrhea). You might be thinking, This has to be an unfortunate coincidence, right? After all, stress occurs in the head, not the stomach. Not quite. If you find yourself asking, Can stress cause diarrhea? The answer is, unfortunately, yes.
While the two may initially appear unrelated, it’s true that stress can lead to diarrhea. That said, treating a stressed belly is a multi-pronged (and often multi-week) project. Continue reading to learn more about how stress impacts your digestive system—and what to do if a stressful situation causes the runs.
How stress impacts the digestive system
Stress and digestive issues often go hand in hand. Think back to the last time you were awaiting test results from a doctor or had a big work presentation. Odds are, one (or both) scenarios caused your stomach to flip or feel like it’s in knots. Emotional events, whether big or small, can elicit reactions like these from the gastrointestinal (GI) system.
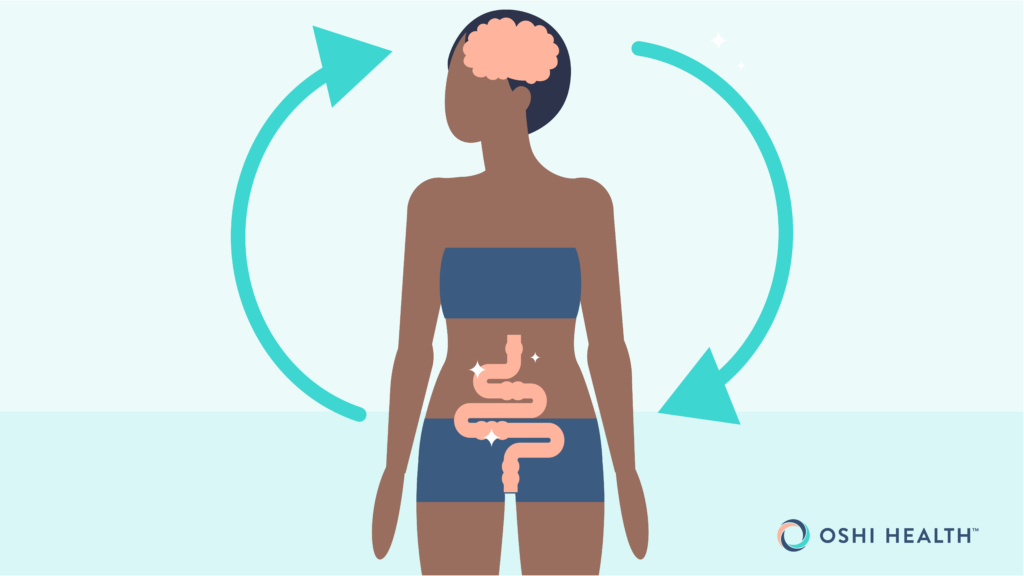
But why are these two physically distant parts of your body influencing each other? Enter: the gut-brain axis. This term refers to the communication channel between the gut and brain, formally referred to as the vagus nerve. The vagus nerve carries messages to and from the central nervous system in the brain and the enteric nervous system in the gut.
And these messages don’t just sit in a metaphorical mailbox. The brain and gut use these cues to regulate your digestion, metabolism, mood, energy, and immune system. When your mind experiences high levels of stress, it sends not-so-nice messages down this communication channel. Your gut, in turn, sets off a series of actions that can disrupt normal gut functioning, according to gastroenterologist Ali A. Khan, MD, MPH. He explains, “The brain-gut axis enables communication between the two systems, meaning stress or anxiety can directly lead to gastrointestinal (GI) distress, including diarrhea.”
Acute vs. chronic stress
Not all stress is created equal. An acute amount of stress (in moderation) can actually motivate us. For example, after registering for my first marathon, I felt a small amount of stress that inspired me to develop—and stick to—my training plan. If that stress had become overwhelming or persistent, however, I might not have made it to the starting line at all.
When stress lasts longer than four weeks, chronic stress makes its entrance. With chronic stress, your body acts as if it’s always in danger. For many people, this level of stress becomes a new norm. But chronic stress is not normal; it has an impact on your mental health, heart health, immune functioning, and—you guessed it—digestive system.
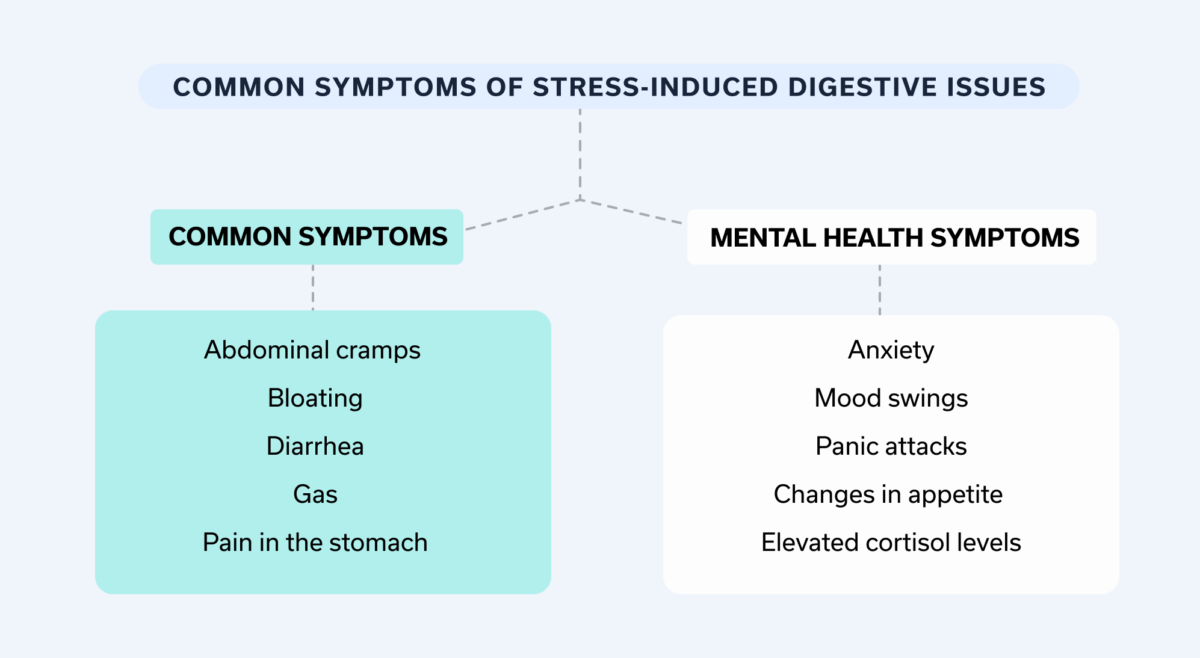
Common symptoms of stress-induced digestive issues
One common symptom is anxiety-induced stomach pain. If you’re wondering, “what does anxiety stomach pain feel like?” the answer is that it varies from person to person—it can feel like a pulling, pinching, or flipping sensation. Additional common symptoms include:
- Abdominal cramps
- Bloating
- Diarrhea
- Gas
- Pain in the stomach
But the gut-brain connection is a two-way street. The chaos in the digestive tract sends similar messages to the brain, which can spark mental health symptoms such as:
- Anxiety
- Mood swings
- Panic attacks
- Changes in appetite
- Elevated cortisol levels
Who is most likely to experience stress-related diarrhea?
Anyone can experience stress-related diarrhea, though those with irritable bowel syndrome (IBS) or inflammatory bowel disease (IBD) may be more likely to. In a 2024 study, those with diarrhea caused by IBS were more likely to experience psychological stress, creating a cruel back-and-forth where IBS symptoms made stress worse and stress exacerbated IBS symptoms.
It’s important to note, though, that stress-induced diarrhea is not always a disease process or a sign that something is amiss. Often, it’s just a normal stress reaction. Even if you don’t have a GI condition and you only experience temporary stress, that can still trigger “fight or flight,” an emergency response that causes a change in your nervous system. When this happens, your body begins to shut down and focus all its energy on fleeing or fighting an assumed threat; in these moments, digestion becomes a very low priority for your body. This can lead to different kinds of GI symptoms, including diarrhea—all as a result of this automatic physiological stress response.
Managing stress-induced diarrhea
So you’re stressed and experiencing diarrhea. Do you just have to suffer through it? Of course not: There are many practical techniques to manage a stressed belly.
Stress management techniques
“Once stress-related diarrhea or IBS is diagnosed, stress reduction becomes a key focus,” says Dr. Khan. There are many at-home strategies you can do to help reduce stress, including meditation and breathing exercises—there is even a type of meditation called gut-directed hypnotherapy that’s designed specifically to reduce GI symptoms. Even just taking a few minutes to be mindful works wonders—UCLA has a free app that can help you get started with mindfulness.
Many people also find stress relief when they move their body. Studies suggest stress levels decease when we move, whether that’s a vigorous workout or a walk around the block.
While stress management is a daily practice, you don’t have to go at it alone. Many people who don’t experience anxiety or stress throw around phrases like, “just stop worrying,” or “stress less.” But those of us who actually experience stress or anxiety regularly know it’s not that easy.
Because stress management is complicated, many people benefit from working with a mental health provider to lower their stress levels. There are even gut-brain specialists, like those at Oshi Health, who can provide psychoeducation about the gut-brain axis and specific breathing practices to control the nervous system’s effect on the gut, as well as other action-based strategies and cognitive behavioral therapy (CBT) tailored to GI conditions.
And no matter what route you take to manage stress, remember: It takes time. Dr. Khan explains, “Coping with stress is a lifelong skill, and progress takes time, so patience is vital.”
Dietary adjustments
Dietary triggers are personal. If you tend to experience GI issues, certain foods might worsen your symptoms. It’s important to keep a food journal during these bouts and record what might trigger you.
That said, there are a few general dietary recommendations that may reduce the likelihood of future GI symptoms, including diarrhea. On a daily basis (and when you’re not experiencing a flare of GI symptoms), opt for tried-and-true gut-friendly options such as:
- Cooked vegetables: Vegetables are a great addition to a gut-friendly diet (though if you’re experiencing a flare-up of GI symptoms, including diarrhea, it may help to cook them before eating).
- Fiber: Okay, this one is more of a frenemy, but when you aren’t experiencing a flare-up of GI symptoms, fiber (whole grains, seeds, nuts, etc.) helps you feel full longer and aids digestion. If you have a GI condition, talk with your GI provider before changing up your fiber intake—and consider prioritizing soluble fiber, such as avocados, cantaloupe, and bananas.
- Fermented foods: Options like kimchi, miso, and yogurt promote healthy digestion. You may want to discuss this one with your GI specialist first if you have a GI condition.
- Low-fat dairy products: If you want to enjoy cheese, milk, or other dairy products, opt for low-fat options.
When writing up your next grocery list, add fewer (or no) foods that tend to trigger GI symptoms and/or stress for many people. These include caffeine, ultra-processed foods, items that are high in sugar, and alcohol.
If you have diarrhea at the moment, you’ll also want to avoid fried foods and perhaps even certain healthy foods that are high in fiber and can cause GI symptoms (think: lentils, chickpeas, peas, beans, green leafy veggies, and berries).
Mindful eating
Anyone else love to kill two birds with one stone (even though that’s a wildly violent metaphor)? If so, mindful eating, the act of cultivating awareness while you eat, may be the move: It helps regulate both stress and GI symptoms, according to a 2019 study.
In theory, mindful eating should be easy. You sit down, focus on your meal, and don’t do anything else. But like many things in life, it’s easier said than done. Some tips to make mindful eating easier include:
- Eat in a calm, distraction-free area (yep, that means no scrolling on socials or watching TV).
- Pay attention to the texture, smell, and flavor of what you eat.
- Eat when you’re hungry (often characterized by low energy and/or stomach grumbling), not when you’re bored.
- Notice when guilt or anxiety pop up around eating. Treat those thoughts with compassion, but note that they are thoughts, not facts.
- Set your eating utensils down between each bite and fully swallow. Plus, slowing down allows you to fully enjoy the flavors of what you’re eating.
- Take a few deep breaths, from your diaphragm, between bites throughout your meal as a way to practice slow and mindful eating.
Lifestyle changes
Your daily routine makes or breaks your gut health as well as your mental health. Let’s say you scroll on social media past your bedtime (we’ve all been there), only to wake up right before work starts, grab an ultra-processed granola bar, and rush out the door. That routine will likely lead to stress and possibly GI symptoms, since it doesn’t prioritize good sleep, mindfulness, or a nutritious diet.
Alternatively, you could set a bedtime for yourself (yes, even as an adult) and stock up on the ingredients for a gut-friendly breakfast. In the morning, you could wake up with enough time to walk the dog, eat that pre-planned breakfast, and complete a five-minute meditation. Just reading that second routine makes me feel calmer.
While our routines will look different per person, most of us could swap one (or a few) stressful habits with healthier ones. Some healthy habit examples might include:
- Swapping nighttime screen time for a book
- Bringing a water bottle to work to stay hydrated all day long
- Making a grocery list so your fridge is stocked with the right ingredients for gut-friendly meals
- Reserving time in your schedule for stress management, whether that looks like a good workout or a meditation
- Deleting the work email off your phone (if you know, you know)
Medications
The solutions above are part of the long game. Over time, they create a lifestyle that isn’t conducive to stress-induced diarrhea. But when you get the runs, you need a more immediate solution—and that’s where medication comes in.
Loperamide (imodium) is one of the most popular over-the-counter (OTC) solutions for diarrhea. It’s FDA-approved for chronic diarrhea related to IBS, traveller’s diarrhea, and acute diarrhea. IB Guard is another potentially helpful option: Made with peppermint oil, it’s a natural antispasmotic that can work well for IBS. A provider may also recommend a prescription medication for severe cases of diarrhea. Of course, you should only take any medication as instructed by your provider.
When to seek medical advice
Diarrhea isn’t usually a reason to visit the emergency room. However, “certain symptoms could indicate that diarrhea is not stress-related and could be signs of a serious illness,” says Dr. Khan. These red flags include:
- Abdominal pain, especially if severe
- Blood in stool
- Mucus in stool
- Nausea
- Tarry, black stool
- Persistent fever
- Stool with an unusual color or odor
- Vomiting
If you experience these red flags, head to the emergency room or call 911.
These red-flag symptoms aren’t the only time you should see a healthcare provider, though—they’re just signifiers of a potential emergency situation. Many people who experience anxiety and stomach issues benefit from working with a qualified gut health provider, such as a gastroenterologist, a nurse practitioner (NP), or a physician associate (also known as a physician assistant or PA), to help manage GI problems. This is especially true when diarrhea is constant, since chronic diarrhea impacts quality of life.
Whole-person GI care—now available from almost anywhere
Oshi Health is where medical, dietary, and gut-brain treatments come together under one virtual roof, all provided by leading GI specialists. With virtual visits available within 72 hours—including evenings and weekends—we make it easy to see a GI provider within days.
Final thoughts
Many things can cause diarrhea, including stress. But before you worry over the stress-diarrhea connection, know that there are ways to manage both your mental health and your GI symptoms, including:
- Change up your eating habits: The dream team for gut and mental health definitely includes a diet full of gut-friendly foods (think cooked veggies, soluble fiber, and fermented foods) as well as mindful eating techniques.
- Reduce stress: Stress management techniques, such as meditation or breathing exercises, can help you lower your stress levels.
- Switch up your routine: Most likely, there are a few stressors in your routine. You can’t control all of them (like that construction project on your street that starts at 7 a.m.). But there are ways to get rid of the stressors within your control (staying up too late, for example, or a lack of daily movement).
If you’re interested in learning whether stress, or something else, is to blame for your diarrhea, contact Oshi Health. Our GI specialists can help you discover what’s causing your GI symptoms and develop a customized treatment plan for lasting relief.
Frequently asked questions (FAQs)
-
If diarrhea is from stress, you may also experience mental health symptoms, such as feeling panicked or worrying excessively. Stress can also cause tension or pain in your body, as well as headaches and/or difficulty sleeping.
-
Stopping stress-related diarrhea is twofold: You must address the stress or anxiety and the digestive symptoms. Stress management techniques, like meditation or regular exercise, can work well—often alongside treatment from a mental healthcare provider. For diarrhea and other GI symptoms triggered by stress, changes to your diet can also help in the long term, while medications can provide short-term relief when symptoms are severe.
-
Anxiety can cause diarrhea, thanks to the gut-mind connection. When you’re stressed or anxious, your mind sends messages, via your vagus nerve, to your gut that can disrupt digestion. A disruption to this connection could lead to many potential symptoms, including diarrhea.
-
The gut and mind are interrelated, meaning that when you’re stressed, you’ll likely feel it in your gut. When there’s a short-term and manageable stressor, you may feel knots in your stomach or as if your stomach is doing somersaults. When that stress becomes chronic, though, it can trigger more serious gut symptoms, like diarrhea, bloating, and abdominal pain.
-
Diarrhea isn’t a comfortable situation, but there are ways you can relax your body when experiencing the runs. Stress management techniques including meditation, breathwork, and mindfulness often help.
-
Stress can upset the stomach due to its impact on the mind-gut connection. Our nervous system runs between the gut and the mind, carrying messages back and forth. If the mind communicates that it’s stressed, the gut may slow down or speed up digestion—the latter may lead to diarrhea.
Oshi is your partner in digestive health
Feel like your digestive concerns are running your life? You’re not alone—and we’re here to help you find lasting relief.
Oshi Health GI providers, gut-brain specialists, and registered dietitians work together to address your symptoms and find solutions that actually work for you.
Whether you’re dealing with chronic digestive issues or unpredictable symptom flare-ups, our GI specialists deliver:
✔ Personalized care plans tailored to your lifestyle
✔ Science-backed strategies to calm your gut
✔ Compassionate, whole-person care
✔ And so much more!
Ready to take control of your gut health?