When anxiety strikes, so can digestive symptoms such as diarrhea. This is because your brain and gut communicate and influence each other. When your stress response kicks in, which is what happens during anxiety (whether temporary or chronic), it can wreak havoc on your gastrointestinal tract, leading to cramping, bloating, really needing to go, and watery or soft stool. All in all, anxiety can definitely send you running for the loo.
If you’ve ever felt like your gastrointestinal (GI) tract has a mind of its own and is causing you “anxiety diarrhea” or “nervous diarrhea,” you might be onto something. Although it’s been called your “second brain,” your gut doesn’t actually have its own brain. (No surprise there.) But it does have its own nervous system branch, the enteric nervous system, which communicates with your brain through the gut-brain axis.
This communication, traveling along the vagus nerve, which connects the brain and gut, is responsible for regulating digestion. When this communication gets disrupted, you may experience poor digestion or discomfort. Anxiety can stress the nervous system, leading to disrupted gut-brain talk.
The situation can go like this: You have to give a big presentation for work or school, but public speaking makes you anxious. About an hour before your event, you find yourself in a bathroom stall, courtesy-flushing and using up all the toilet paper. You have anxiety diarrhea.
Or maybe you have generalized anxiety disorder (GAD), a chronic mental health condition where you have persistent worry and anxiety about everyday events. When your GAD symptoms ramp up, you find that your GI symptoms also flare, leaving you wanting to stay in your comfy pants and as close to the bathroom as possible.
You’re not imagining that bouts of diarrhea might be connected to your anxiety. Again, this is because your gut and brain are talking to each other, and sometimes miscommunication can occur—especially in times of high anxiety and stress. Plus, stress can do a number on your GI tract in multiple ways.
Additionally, some GI conditions that feature diarrhea as a symptom share links with anxiety, including irritable bowel syndrome (IBS) and inflammatory bowel disease (IBD)—which includes Crohn’s disease and ulcerative colitis.
In this article, we cover why anxiety can cause diarrhea, the nitty-gritty details of the gut-brain axis and your nervous system, common symptoms and triggers, and what you can do to prevent and manage anxiety diarrhea.
Understanding anxiety diarrhea
What is anxiety diarrhea? It’s exactly what it sounds like: sudden or ongoing loose or watery stool triggered by anxiety. Anxiety can be a temporary reaction to a stressful situation or event. Or it can be chronic and part of an anxiety disorder. Anxiety disorders affect up to 20 percent of people each year.
Why does anxiety cause diarrhea? Anxiety can trigger several GI symptoms, from constipation or heartburn to cramping or the dreaded “runs.” Let’s explore the nervous system to gain a better understanding of why your brain might send you running for a place you can drop trow and find relief.
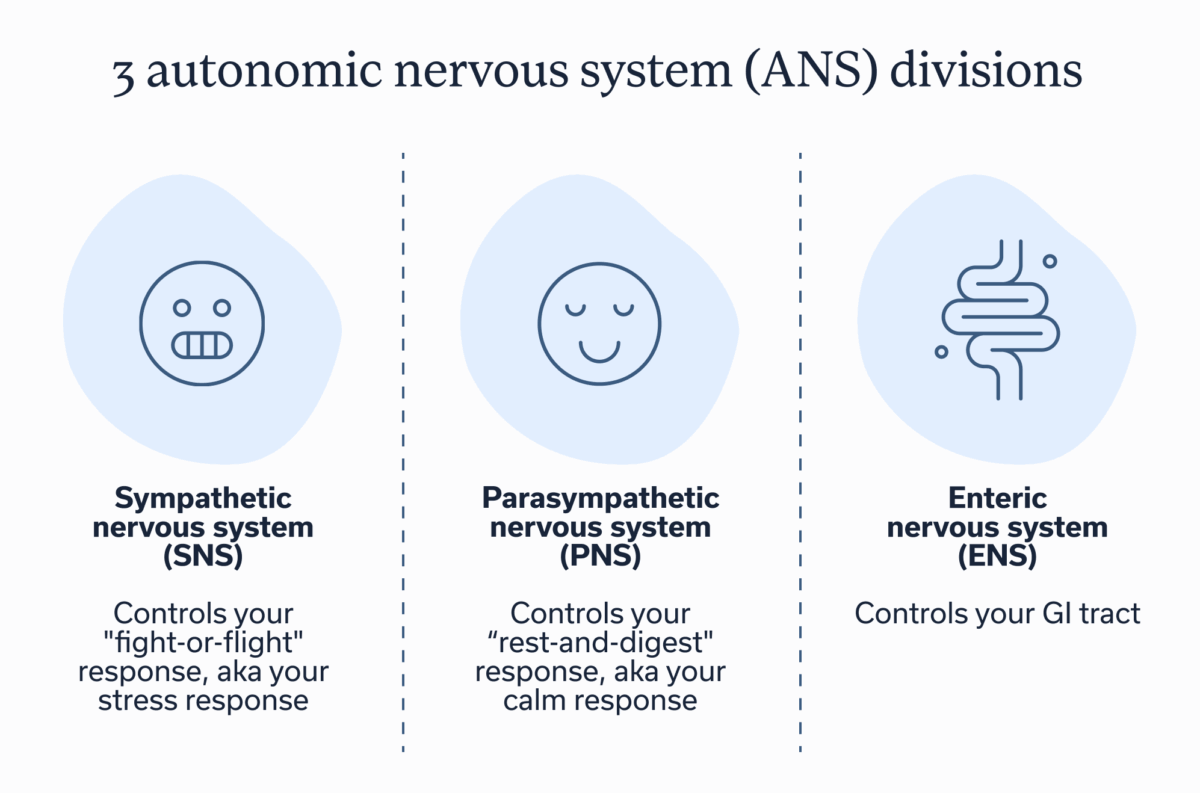
Your autonomic nervous system (ANS) controls the involuntary processes in your body, from your heart rate, breathing, body temperature, and blood pressure to your sexual arousal and digestion. Your ANS has three divisions.
3 ANS divisions:
- Sympathetic nervous system (SNS). Controls your “fight-or-flight” response, aka your stress response.
- Parasympathetic nervous system (PNS). Controls your “rest-and digest” response, aka your calm response.
- Enteric nervous system (ENS). Controls your GI tract.
You’ve likely heard about your fight-or-flight response before. This is the system that kicks in when you encounter a stressful moment or situation. You feel an adrenaline rush, your heart rate ratchets up, and maybe you start to sweat. It’s the system that helps keep you safe from danger by getting you ready to meet a threat head on or to flee.
Your rest-and-digest response is almost like the opposite of fight-or-flight. It’s the system engaged when you feel calm or chill. It helps regulate other bodily functions, such as digestion and waste elimination.
Your ENS is a neuronal network within the walls of your GI tract. It controls digestive functions, such as gastric secretions, motility (the movement of food and waste), and more. It works independently and in conjunction with the SNS and PNS.
These three ANS nervous system branches are involved in communication along the gut-brain axis. The ENS can operate on its own, but it also receives input from the SNS and PNS. Likewise, the ENS sends signals to the SNS and PNS.
Understanding the gut-brain axis
When you experience an acute bout of anxiety or encounter a trigger for your ongoing anxiety disorder, your body goes into fight-or-flight mode to help you address the stressor.
Imagine that your body has a switch or toggle. When fight-or-flight mode toggles on, your body switches off some of the processes of rest-and-digest mode. It does this so your body can put most of its resources toward addressing the immediate “threat” to keep you safe.
But when your body pauses rest-and-digest mode, GI symptoms, including constipation or diarrhea, can ensue. This is because the PNS greatly influences the ENS, and vice versa, affecting GI secretions, motility (the movement of food and waste), smooth muscle contractions, and more.
Let’s revisit our example of having to give a presentation. Perhaps you’ve been low-grade nervous and a bit on edge about it all week, but the “butterflies in your stomach” really start fluttering not long after lunch when you’re getting closer to the time of the main event. Your digestive system was busy breaking down the soup and salad you ate, but the sudden uptick in anxiety symptoms cranks up your fight-or-flight mode, putting your rest-and-digest system on pause. The switch has flipped. Suddenly, your gut gets confused about the pause, and diarrhea or other GI symptoms ensue.
Anxiety disorders can cause similar issues. Instead of experiencing occasional anxiousness or nervousness in the face of a stressor, you might experience chronic anxiety surrounding everyday activities, such as managing work tasks, going to the grocery store, interacting with others, and more.
With an anxiety disorder, your fight-or-flight mode can be overactive or hypersensitive and sometimes get stuck “on.”
This can occur because your brain can become hypervigilant, meaning subconsciously, you’re always monitoring for a threat, even when you’re safe. Hypervigilance can occur after trauma, whether recent or from your childhood. This is because trauma can have long-term effects on your autonomic nervous system.
Additionally, ongoing stress can disrupt the gut microbiome (causing an imbalance in the bacteria and fungi that live in the gut), and the situation can occur in reverse, meaning the status of your gut health can impact your mental health. For example, having a disrupted gut microbiome can also lead to anxiety and stress.
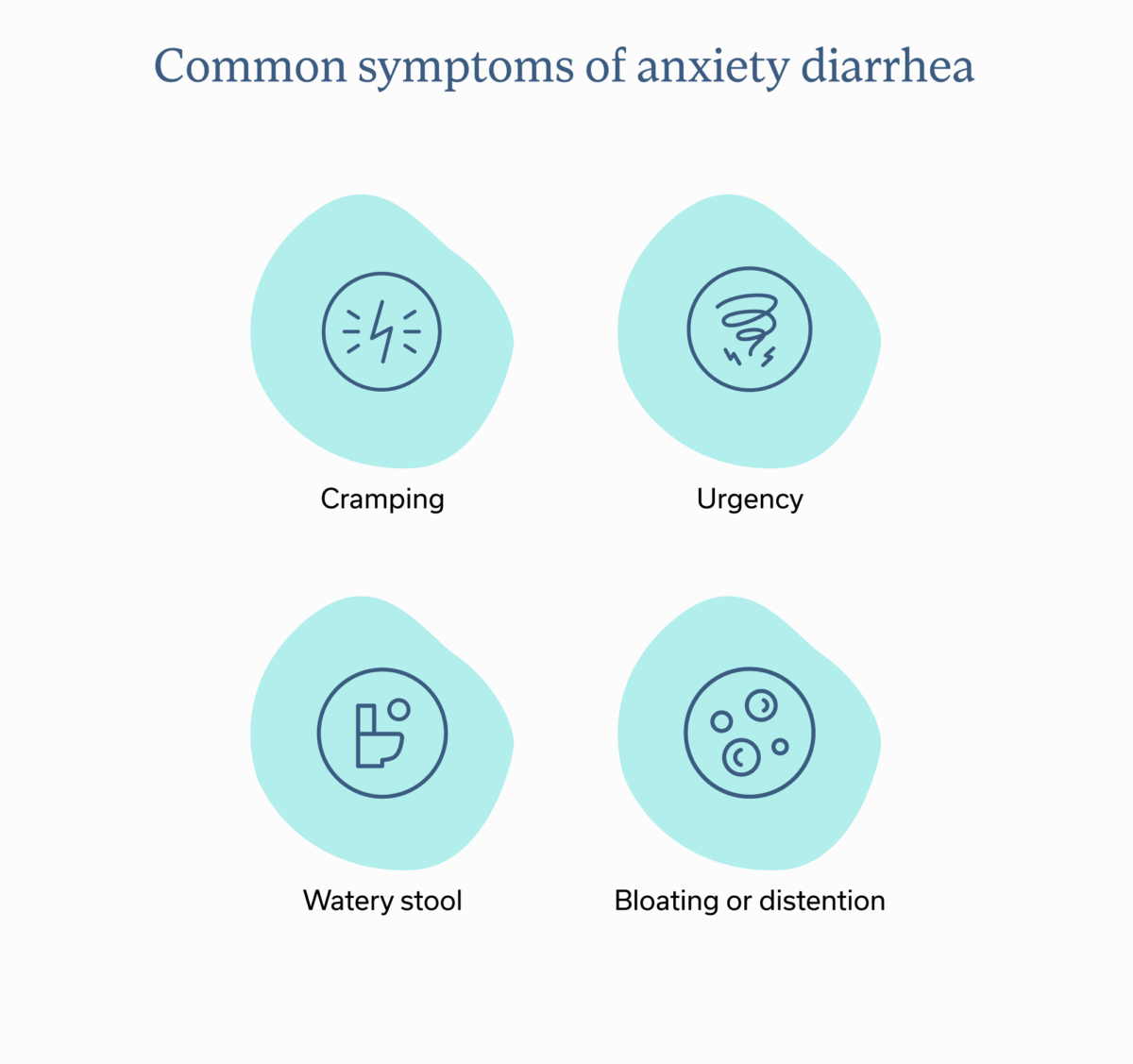
Common symptoms of anxiety diarrhea
The features of anxiety diarrhea are like any other type of diarrhea, but the symptoms coincide with anxiety.
- Cramping. The stress response, including the hormones it releases, can lead to heightened action of the lower GI tract, causing increased colonic propulsive activity, which stimulates bowel movements and can lead to pain or other sensations when your colon is ready to empty.
- Urgency. Stress can ratchet up visceral hypersensitivity in the colon, sending your brain signals that you need to go “right now.”
- Watery stool. Stress can also cause a reversal of small bowel water and electrolyte absorption, meaning you may have increased fluid in your small intestine, contributing to watery, soft, or loose stools.
- Bloating or distention. Increased water in the bowel, increased muscle contractions, and other factors can also lead to bloating or abdominal distention.
Risk factors and triggers
Risk factors for anxiety diarrhea can include anxiety disorders and underlying GI conditions.
Anxiety disorders
Anxiety disorders—such as social phobias, obsessive-compulsive disorder (OCD), post-traumatic stress disorder (PTSD), and panic disorder—are chronic conditions, and they are strongly associated with GI symptoms, such as diarrhea.
Chronic stress
Even if you don’t have an anxiety disorder, you might be experiencing chronic stress. What’s the difference between acute and chronic?
Acute stress is temporary. It can occur when you have to take a test, are experiencing a relationship conflict, are nearing a big deadline, or you’ve gotten into a fender bender, etc. It resolves once the stressor passes.
Chronic stress, on the other hand, is ongoing. It can occur when a bunch of acute stressors pile up. Or maybe you’re going through a longer-term relationship issue such as a breakup or divorce, you have too many things on your proverbial plate, or you are frustrated with the state of the world, your country, or your community. Chronic stress can turn your fight-or-flight mode on too often, leading to tummy trouble. And it can create a new normal of gut-brain communication disruption that can be lasting, even after stress resolves. For example, chronic stress affects the gut microbiome and causes inflammation in your GI tract, both of which can lead to diarrhea.
IBS
IBS subtypes include IBS-D (where diarrhea is a prevalent symptom), IBS-C (where constipation is more prevalent), and IBS-M (where you experience a mix of diarrhea and constipation as symptoms). If you have a diagnosis of IBS, you may be more likely to experience anxiety diarrhea. Or if you commonly experience diarrhea, you could have IBS. People with anxiety have a more than two-fold risk of developing IBS.
IBD
Diarrhea is a common symptom of IBD. And people with IBD have a higher risk of developing anxiety and depression. Likewise, anxiety and depression can cause IBD flares. So if you have IBD, you may be more at risk for experiencing anxiety diarrhea.
Diagnosing anxiety diarrhea
Since anxiety diarrhea shares connections with underlying GI conditions, consulting with an experienced GI provider can help. They can determine if you have a condition that’s contributing to your diarrhea and work with you to address it. GI providers can include gastroenterologists, GI registered dietitians, nurse practitioners, physician assistants, and licensed behavioral health providers, who specialize in gut brain treatment. These gut-brain specialists teach interventions that manage GI symptoms by calming the nervous system and enhancing gut brain communication.
Treating anxiety diarrhea involves an individualized approach, since each person is different. Your provider might ask you about your medical history, GI symptoms, anxiety symptoms, diet, lifestyle, and other factors unique to you, in order to create a personalized treatment plan.
Managing and treating anxiety diarrhea
If you’re a frequent rider on the unfun anxiety diarrhea train, you may be wondering how to exit the car. What works for you will be different from the next person. That’s why consulting a GI provider is a great idea. But here are a few general tips.
Lifestyle adjustments
Healthy lifestyle changes can be excellent tools to help manage anxiety diarrhea. Some of the basics include getting adequate sleep and getting regular physical activity, both of which can help manage stress. Tapping into additional stress-management tactics, such as yoga or meditation, can also keep your stress response in check.
Dietary changes
Dietary changes can be helpful, especially if certain foods are triggers for your anxiety diarrhea or exacerbate the symptoms of an underlying GI condition such as IBS or IBD. Common triggers for IBS-D, for example, include beans, legumes, caffeine, some grains, dairy, and more.
Some foods or ingredients in general can also worsen anxiety, which could contribute to diarrhea. For example, foods with added sugar can cause blood sugar spikes and crashes, which can affect mood. And ultra-processed foods—think fried items, packaged foods with additives and preservatives, and more—are linked to worsened mental health. A high caffeine intake can also give you the jitters and worsen anxiety. Plus, caffeine can worsen IBS symptoms, increase gut motility, and cause more frequent or loose stools.
Working with a GI registered dietitian can help you uncover which foods are triggers for you. That doesn’t necessarily mean you can’t eat the foods you love or that are important to your culture. Your provider can help you figure out the best dietary strategies. They will take an additive approach rather than a restrictive one whenever possible; sometimes this may mean finding a comparable alternative.
Finally, a GI registered dietitian can help you address any imbalances in your gut microbiome that could be contributing to anxiety diarrhea.
Psychological treatments and techniques
Working with a licensed behavioral health provider, who specializes in gut brain treatment can help you determine what the best treatments and techniques are for you, but here are a few that may help.
- Cognitive-behavioral therapy for GI (CBT-GI): CBT helps you analyze thought patterns that may contribute to mental health symptoms, including anxiety, and learn how to reframe them. CBT-GI helps you do this in the context of your GI conditions and symptoms.
- Gut-directed hypnotherapy. Hypnotherapy uses clinician-guided hypnosis to help improve gut-brain communication, which can then help ease GI symptoms.
- Mindfulness. This approach helps someone focus on the present moment to ease stress and anxiety. Gut-brain specialists often employ guided meditations, among other activities, to promote mindfulness.
- Breathing techniques. Mindfulness techniques sometimes use breathwork, such as diaphragmatic breathing, to help you tap back into your rest-and-digest mode when you notice you’ve slipped into fight-or-flight mode.
Medication options
In some cases, you may need medications to help address anxiety and diarrhea. For example, anti-diarrheal medications can help in the short term. But they shouldn’t be taken regularly. Additionally, medications, including neuromodulators, can help to improve communication between the brain and nervous system in the gut, often leading to an improvement in symptoms.in the long term.
When to seek medical help
Many people experience anxiety diarrhea. The occasional instance of loose or watery stool is generally not cause for concern. But if you have ongoing anxiety diarrhea or ongoing diarrhea in general, you should talk to a clinician to help understand why.
Seek urgent medical care for the following symptoms:
- Sudden and severe stomach pain that impacts your daily functioning
- GI issues that are accompanied by a high fever
- Blood in your stool
- Black or tarry stool for several days
- A hard abdomen
- GI issues that cause you to feel dizzy or to faint
- GI issues accompanied by heart palpitations or shortness of breath
Key takeaways
- When anxiety strikes, so can diarrhea because of how your gut and brain interact.
- Your stress response can trigger diarrhea by halting some GI processes and stimulating others.
- You can ease anxiety diarrhea through techniques that help you manage your stress response, making other lifestyle changes, and taking medications if needed.
- A knowledgeable GI provider, such as those at Oshi Health, can help you manage your symptoms by customizing a treatment plan that’s best for you.
FAQ
-
Yes, anxiety can cause diarrhea because of the way your stress response impacts the digestive tract and because the brain and gut communicate via the gut-brain axis.
-
If you are experiencing stress diarrhea, you can use techniques that help you switch from your stress response (fight or flight) to your calm response (rest and digest). Techniques might include deep breathing exercises, meditation, and more. Taking an over-the-counter anti-diarrheal medication can also help ease loose stool in the short term.
-
The 3-3-3 rule for anxiety is a technique you can use in the moment to help calm you. Name three things you see, followed by three things you hear. Then move three body parts. The process helps you focus on the present, rather than on anxious thought patterns.
-
Yes, diarrhea can be a part of a panic attack because the situation ramps up your stress response, placing some digestive processes on hold while speeding others up, which can lead to loose and watery stool and the urgency to “go.”
Oshi is your partner in digestive health
Feel like your digestive concerns are running your life? You’re not alone—and we’re here to help you find lasting relief.
Oshi Health GI providers, gut-brain specialists, and registered dietitians work together to address your symptoms and find solutions that actually work for you.
Whether you’re dealing with chronic digestive issues or unpredictable symptom flare-ups, our GI specialists deliver:
✔ Personalized care plans tailored to your lifestyle
✔ Science-backed strategies to calm your gut
✔ Compassionate, whole-person care
✔ And so much more!
Ready to take control of your gut health?