Constipation can be incredibly frustrating and uncomfortable. Understandably, you may be in search of relief. Magnesium, an essential mineral and electrolyte, can come to your aid, generally producing a bowel movement within hours. But not all magnesium types are created equal when it comes to their laxative effects. Magnesium oxide and citrate are gentle yet effective.
Anyone who’s ever been constipated knows how it can affect your overall well-being. You might feel full, uncomfortable, sluggish, and fatigued when visits to the loo deliver either nothing or the smallest of pebble poops, leaving you frustrated and seeking relief.
You’re not alone. About 16 percent of all adults and 33 percent of those over 60 have ongoing constipation symptoms. Those who are more at risk include people who are assigned female at birth, who are pregnant, who are seniors, or who fit into more than one of those categories. People who have health problems such as irritable bowel syndrome (IBS), take certain medications, or eat a diet deficient in fiber are also at a higher risk.
Increasing fiber can be a helpful solution if a lack of it is the culprit, but it can take a while to work. When constipation strikes, you want faster relief. Magnesium, a mineral and electrolyte, can be a superhero in these instances, generally working within several hours.
That said, not all magnesium is created equal. There are multiple different types of magnesium, and they each work in different ways. For this reason, understanding exactly what each one does can be helpful for finding the right kind of constipation relief for you.
What is magnesium?
Magnesium is a mineral necessary for more than 300 enzymatic reactions in the body that regulate processes such as blood pressure regulation, protein synthesis, glucose (blood sugar) control, and nerve and muscle functioning.
Magnesium is also one of the body’s seven essential electrolytes, which help maintain fluid balance by “pulling” fluids from one area in the body to another in a process you may remember from middle school biology: osmosis. And osmosis is how magnesium can help with constipation.
Does magnesium really help you poop?
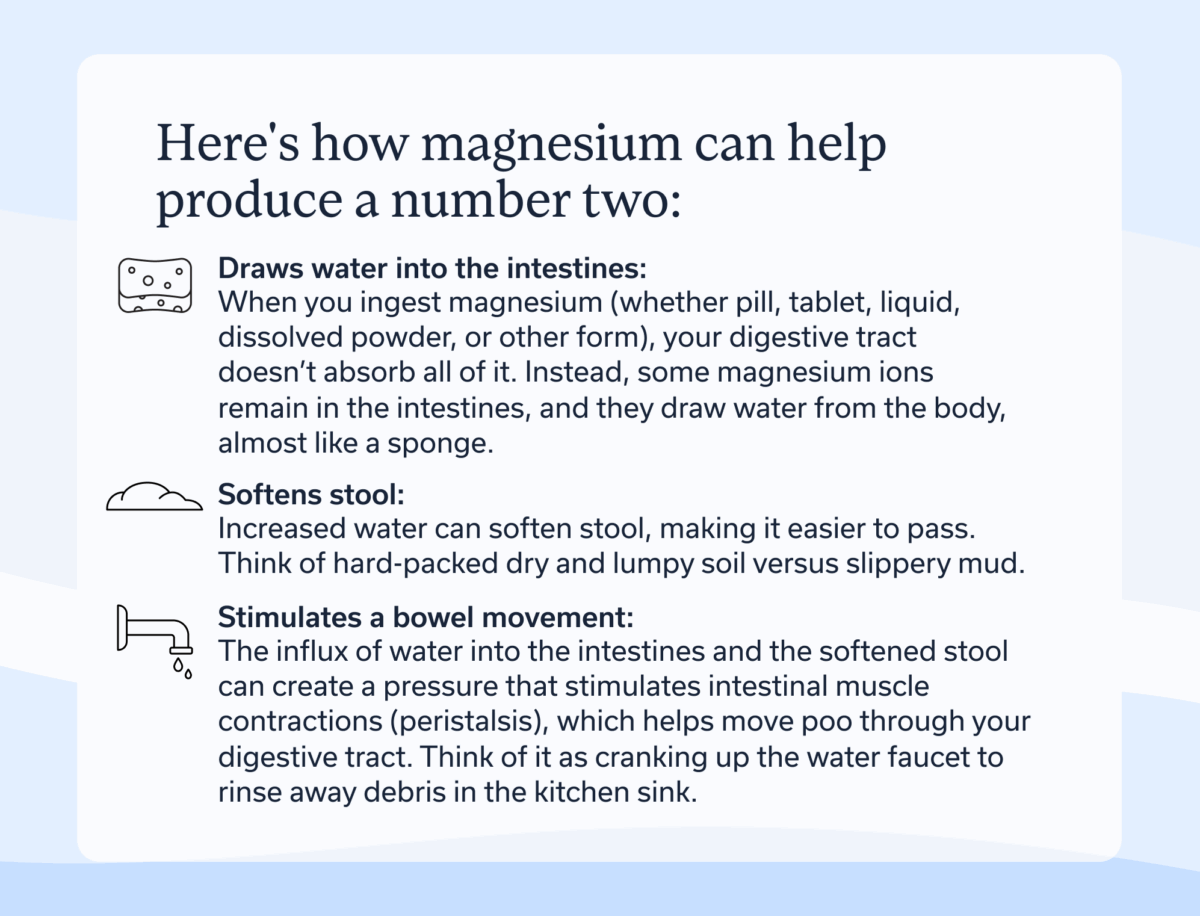
Yes. Here’s how magnesium can help produce a number two:
Magnesium:
- Draws water into the intestines: When you ingest magnesium (whether pill, tablet, liquid, dissolved powder, or other form), your digestive tract doesn’t absorb all of it. Instead, some magnesium ions remain in the intestines, and they draw water from the body, almost like a sponge.
- Softens stool: Increased water can soften stool, making it easier to pass. Think of hard-packed dry and lumpy soil versus slippery mud.
- Stimulates a bowel movement: The influx of water into the intestines and the softened stool can create a pressure that stimulates intestinal muscle contractions (peristalsis), which helps move poo through your digestive tract. Think of it as cranking up the water faucet to rinse away debris in the kitchen sink.
Types of magnesium supplements for constipation relief
As mentioned earlier, not all magnesium is created equal—nor will it all relieve your discomfort. The body absorbs some types of magnesium better than others. A highly absorbed form, such as magnesium glycinate, is beneficial for correcting magnesium deficiencies, but it leaves little in the intestine to have its osmotic, and therefore, laxative effects.
On the other hand, when too much left is in the intestines, as is the case with magnesium hydroxide, it can produce the strong urge to go, causing discomfort such as cramping. But it will generally produce a bowel movement if you want to take a strong approach to finding relief.
All that said, your symptoms may require a Goldilocks approach with a magnesium that has a “just right” level of absorption, acting as a moderate laxative. In this case, magnesium citrate would fit the bill.
Let’s explore the different types of magnesium supplements and which is best for constipation. These types are ranked from least absorbed (producing a strong laxative effect) to most absorbed (less likely to produce a bowel movement). Options that fall in the middle will still help you go number two but will be gentler on your system.
Magnesium hydroxide
Magnesium hydroxide (aka milk of magnesia) is poorly absorbed, which can be a good thing for urgent constipation relief (under six hours), as it stays in the intestines to do its osmotic work. However, it should be used sparingly because it can produce diarrhea, cramping, and electrolyte imbalance with excessive use. It should not be used long term for chronic constipation.
Magnesium sulfate
Magnesium sulfate (aka Epsom salt) is also poorly absorbed, making it highly effective for constipation when consumed orally. It can produce quick constipation relief (under six hours). As with magnesium hydroxide, magnesium sulfate should be used sparingly rather than regularly. It can also produce side effects, such as sudden loose stool, and can contribute to an electrolyte imbalance.
If you buy Epsom salt, be sure it’s a form you can safely take orally, rather than one intended for the bath only, as these might contain additives, such as lavender or another essential oil that’s not meant to be ingested. All Epsom salts are safe for your bath, but not all are safe for you to dissolve in water for drinking, so read labels carefully and follow their instructions.
Magnesium oxide
Magnesium oxide is another poorly absorbed form, but it’s not as fast acting (takes more than six hours) as magnesium hydroxide or sulfate. It’s ideal for overnight relief because if you take it around bedtime, you should wake up ready to go in the morning. Since it works a bit slower, magnesium oxide may reduce your risk for intense side effects, such as diarrhea or cramping. Consult a provider before using it long-term.
Magnesium citrate
Magnesium citrate has a higher absorption rate than magnesium oxide. But it’s faster acting, doing the job in less than six hours. It’s ideal for bowel prep (cleaning out the intestines) before procedures such as colonoscopy. It serves a gentler alternative to magnesium hydroxide or sulfate, but it acts faster than the also-gentle magnesium oxide. As a bonus, since more of magnesium citrate is absorbed than magnesium hydroxide, sulfate, or oxide, it is also a good choice if you have constipation issues coupled with a magnesium deficiency. Like the other magnesium types we’ve listed so far, magnesium citrate is meant for short-term use, unless a provider recommends you take it longer term.
Magnesium chloride
Magnesium chloride is well-absorbed, making it less effective for constipation relief. However, if other types produce extreme side effects, magnesium chloride might serve as a gentler option for you. But it might take longer (more than six hours) to work. It’s also useful for correcting a magnesium deficiency and to help treat certain conditions, such as migraine. It is suitable for longer-term use at recommended doses under the guidance of a medical professional.
Magnesium glycinate and other types
Additional types of magnesium include glycinate, malate, taurate, L-threonate, lactate, and orotate. These are not generally effective as laxatives since they are highly absorbed. They still have benefits for correcting magnesium deficiency and managing chronic conditions, such as migraine or insomnia, and are suitable for longer-term use as directed by a clinician.
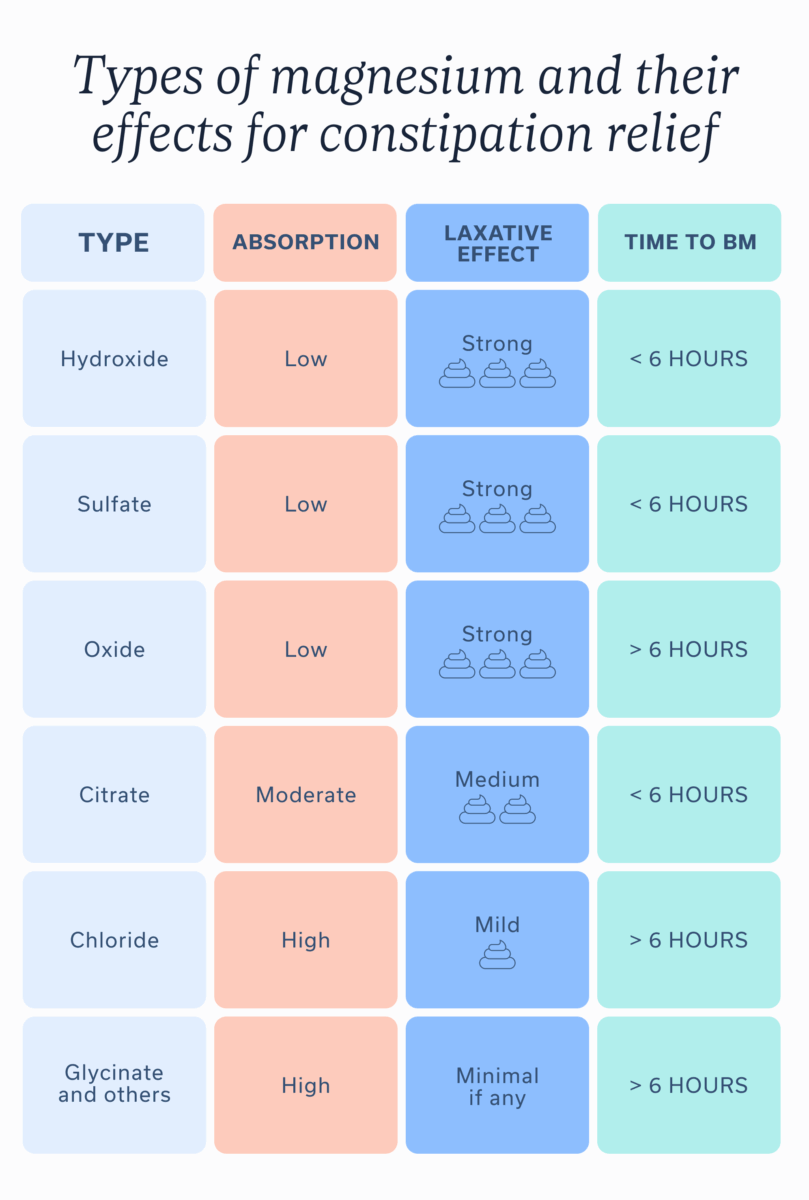
Types of magnesium and their effects for constipation relief
| Type | Absorption | Laxative effect | Time to BM |
| Hydroxide | Low | Strong 💩💩💩 | < 6 hours |
| Sulfate | Low | Strong 💩💩💩 | < 6 hours |
| Oxide | Low | Strong 💩💩💩 | > 6 hours |
| Citrate | Moderate | Medium 💩💩 | < 6 hours |
| Chloride | High | Mild 💩 | > 6 hours |
| Glycinate and others | High | Minimal if any | > 6 hours |
So, which magnesium is most effective for your constipation relief? The answer will depend on your specific needs. Here are the main points to keep in mind:
- Types that aren’t as readily absorbed will work faster but may produce intense side effects.
- Types that have a moderate absorption rate will take longer but prove a bit gentler.
- Types that have a high absorption rate will be less effective for constipation and will take longer, but they are also more suitable for managing chronic conditions and correcting magnesium deficiencies.
It’s always a good idea to talk to a knowledgeable provider who can recommend the best type of magnesium for your unique circumstances, underlying conditions, medications, and more.
How to use magnesium for constipation
When taking magnesium for constipation, start with the recommended product dose. Or you may even want to try a smaller dose to see how the product affects you. Consume with plenty of water, and consider consuming in the evening before bed.
Taking magnesium at this time can be beneficial because its osmotic effects will go to work for you overnight. As a bonus, some forms of magnesium may improve your sleep. By morning, you should feel the urge to go. However, if you have a more severe form of constipation, your body may take longer to respond.
Hydration is crucial to keep electrolytes in balance, but the water also helps produce the osmotic effect. And since osmosis is the act of pulling water from one area to another, you’ll need to replenish your body’s fluid stores.
Whichever form of magnesium you take—whether in pill form, a powder, or a liquid solution—be sure to drink eight to 10 ounces of water with it.
Potential side effects and precautions
Remember that faster-acting forms and those with less absorption (magnesium hydroxide and sulfate) may cause more intense side effects. Those that have limited absorption but are longer acting (magnesium oxide) and those that are moderately absorbed but faster acting (magnesium citrate) may produce fewer or less intense side effects.
Potential side effects of magnesium for constipation:
- Abdominal cramping
- Gas
- Nausea or vomiting
- Loose or watery stool
- Intense urge to go
- Electrolyte imbalance
- Magnesium toxicity (in high doses)
Those with kidney disease or heart conditions, or who are on medications that affect magnesium levels, should consult their healthcare provider before supplementing.
Several medications interact with magnesium:
- Bisphosphonates (for bone health)
- Antibiotics
- Diuretics (often used for heart conditions)
- Proton pump inhibitors (to treat acid reflux)
Alternatives to magnesium for constipation
Magnesium isn’t the only trick in the book for finding relief from constipation. These solutions may also help.
- Consider other over-the-counter options: A stool softener can help get things moving, or other osmotic laxatives, such as polyethylene glycol, can serve as a magnesium substitute.
- Improve gut-brain communication: Conditions such as IBS, which can cause chronic constipation, are often rooted in disrupted gut-brain interaction. Working with a gut-brain specialist can help improve this communication.
- Manage mental health: Stress, anxiety, and inadequate sleep can all contribute to constipation. Focusing on these aspects and treating any underlying mental health conditions may help with regularity.
- Eat plenty of fiber: Fiber has many positive effects on the gut, including bulking stool. But be sure to increase your intake slowly over time to avoid any discomfort. Too much fiber, especially in the absence of hydration, can paradoxically contribute to constipation. Talking to a GI registered dietitian may be of benefit; they can help you customize your fiber needs.
- Engage in physical activity: Movement helps encourage bowel movements, so go for a walk, a light jog, a bike ride, or do whatever it is you enjoy.
- Change your toileting routine or posture: Simple changes can help, such as allowing more time to use the potty upon waking or adding a defecation postural modification device to your bathroom.
- Ask your doctor about prescription medications: In some cases, you may need a prescription for neuromodulators or secretagogues.
- Stay hydrated: No matter which methods you use to resolve constipation, staying hydrated is crucial. So drink up that H2O.
When to see a healthcare provider
Everyone will experience a bout of constipation from time to time as a result from a change in routine, dietary habits, activity level, medications, or other factors. These occasional incidents are generally not cause for concern as long as you are eventually able to find relief, whether naturally or with the help of magnesium.
However, if you have ongoing constipation, you could have an underlying condition that warrants investigation and a treatment plan, so you can go number two with success and a feeling of satisfaction.
Some underlying conditions that can cause constipation include:
- Irritable bowel syndrome (IBS)
- Inflammatory bowel disease (IBD)
- Colorectal cancer
- Diverticular disease
- Neurological conditions (e.g., multiple sclerosis, Parkinson’s disease, etc.)
- Endocrine conditions (e.g., thyroid issues, diabetes, and more)
- Pelvic floor dysfunction
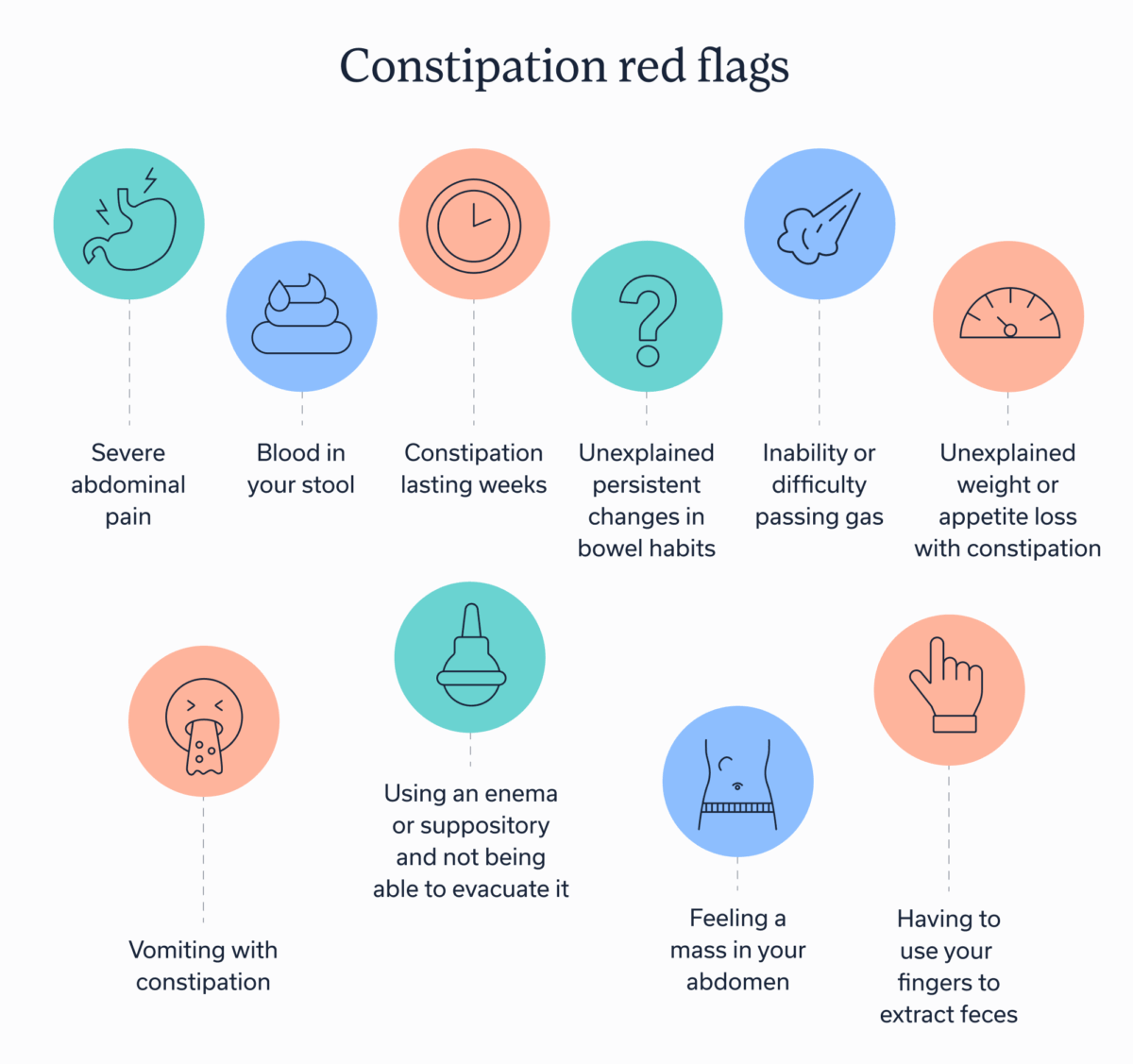
In some cases, constipation can be a medical emergency. The following are some constipation red flags that are signs to see or talk to a provider right away.
Constipation red flags
- Severe abdominal pain
- Blood in your stool
- Constipation lasting weeks
- Unexplained persistent changes in bowel habits
- Inability or difficulty passing gas
- Unexplained weight or appetite loss with constipation
- Vomiting with constipation
- Feeling a mass in your abdomen
- Having to use your fingers to extract feces
- Using an enema or suppository and not being able to evacuate it
Key takeaways
- Magnesium can be a great tool for addressing occasional constipation, but not all forms work well to produce relief.
- The magnesium types that work best for constipation are ones that the body doesn’t fully absorb.
- This is because the magnesium ions that remain in your digestive tract pull water in to help produce a bowel movement.
- To find the right magnesium for you and to create a treatment plan for your constipation, reach out to Oshi Health.
FAQ
-
The best form of magnesium for constipation will depend on your unique situation and your desired effect. Types that aren’t as readily absorbed (hydroxide and sulfate) will work faster but may produce intense side effects. Those that have limited absorption but are longer acting (magnesium oxide) and those that are moderately absorbed but faster acting (magnesium citrate) may produce fewer or less intense side effects. Those that have a high absorption rate (glycinate, malate, taurate, L-threonate, lactate, and orotate) will have little effect on constipation.
-
Yes, magnesium can make you poop if it is a form that the body doesn’t too readily absorb. Magnesium works for constipation by pulling water into the intestines where it can trigger a bowel movement. Highly absorbed forms of magnesium enter the bloodstream rather than staying in the digestive tract for a laxative effect.
-
You can take magnesium for constipation at any time. However, you may wish to take it overnight to produce a bowel movement in the morning. If you have more severe constipation, magnesium may take longer to work.
-
Magnesium use for constipation relief could cause the following side effects: abdominal cramping, gas, nausea or vomiting, loose or watery stool, the intense urge to go, an electrolyte imbalance, and magnesium toxicity (at high doses).
Get relief from chronic constipation
Feel like your bathroom habits are running your life? We get it. And we’re here to help. Oshi Health GI providers, gut-brain specialists, and registered dietitians work together to find solutions that actually work for you.
Whether you’re dealing with chronic constipation or fluctuating bowel movements, our GI specialists deliver: