Meet your team of GI specialists and dietitians
Anti-inflammatory foods have antioxidant properties, which means they fight inflammation in your body and help reduce your risk for several chronic diseases. They can also be a helpful tool in your arsenal if you’re managing a gastrointestinal (GI) condition. What are some of the top anti-inflammatory foods? Fruits and veggies, nuts and seeds, fatty fish, and coffee and tea—to start.
Ready to reduce your inflammation? Work with registered dietitians and GI specialists for sustainable relief.
Whenever I think of the word “inflammation,” I picture the fire emoji on my phone. Inflammation is the way your body signals that something is wrong, and it causes the immune system to jump into action. Think of it this way: If your house is on fire, you call the fire department to put the fire out. But we can take several steps to avoid or lessen the chance of a fire in the first place and to counteract the blaze if one ignites. Anti-inflammatory foods can be both your first responders and your preventive measures.
The typical Western diet—which is full of ultra-processed foods, added sugar, and additives that boost flavor and shelf life—can cause inflammation in our bodies. And that inflammation, particularly when chronic, can wreak havoc on our gastrointestinal (GI) health. The good news? It’s pretty easy to tweak your diet to include some of the best anti-inflammatory foods out there—those that help support GI health, reduce symptoms, and lead to better overall health. Plus, they’re delicious to boot.
In this article, we’ll explore what inflammation is, how to build an anti-inflammatory diet, and which foods to reduce or eliminate if you want to keep inflammation in check.
How inflammation affects the body
The first thing to know about inflammation is that it isn’t always a bad thing. It does get a bad rap for its connection to chronic diseases, such as inflammatory bowel disease (IBD), arthritis, and more. But inflammation in the short term—aka “acute inflammation”—helps keep your body safe.
For example, not too long ago, I ever-so-gracefully slipped on a rain-soaked curb, fell, and skinned my knee while walking to a show. Later, my knee was swollen and red as my body tried to repair the issue and ward off infection. That redness was the result of inflammation kicking off a multi-step process involving my immune system. This includes four superhero-like tasks.
Acute inflammation process
- Irritation is the alarm signal that helps recruit white blood cells to the affected area—they’ll help with protection and repair.
- Amplification involves the release of chemicals that recruit additional types of white blood cells to ramp up the fight. Think of the process as an army bringing in more troops.
- Destruction is when the immune system does its job to neutralize (calm) the injury—and remove debris or bacteria that could cause an infection.
- Termination is the release of chemical substances to chill out the inflammatory process before damage can occur.
As you can see, the acute inflammatory process occurs to help quickly fix a bodily issue—like my skinned knee, a tweaked elbow from a heated game of pickleball, or even a bout of the seasonal nasties, such as the flu or common cold. But chronic inflammation—which is ongoing and becomes problematic—can also occur because of inflammation overload.
Get clinically-proven GI care—from almost anywhere
Oshi Health is in-network with most major insurance


Chronic inflammation
With chronic inflammation, the immune system can’t get us through all four of the acute phase steps. Instead, we get stuck in the irritation and amplification phases, because the immune system is having trouble managing its inflammatory load.
Think of it as if you’ve got two teams playing a game in your body. If the pro-inflammatory processes team is outperforming the anti-inflammatory processes team, then chronic inflammation wins out. The anti-inflammatory team you’re rooting for isn’t going to get the trophy.
Chronic inflammation can occur for multiple reasons, including exposure to toxins (such as pollution, tobacco use, or problematic bacteria and fungi) or from a pro-inflammatory diet.
What can we do?
One of the best ways to combat inflammation and all its symptoms is to eat a well-balanced and diverse diet, full of a variety of fruits, vegetables, nuts/seeds, grains, legumes, and lean protein sources. This helps support the immune system, maintains healthy cholesterol and glucose levels, and more.
The science behind anti-inflammatory foods
Anti-inflammatory foods have antioxidant properties. The term “antioxidant” gets thrown around a lot as a good-for-you thing. But what does it mean? Antioxidants scavenge (counteract) some of the unstable molecules, called free radicals, that can cause trouble in our bodies.
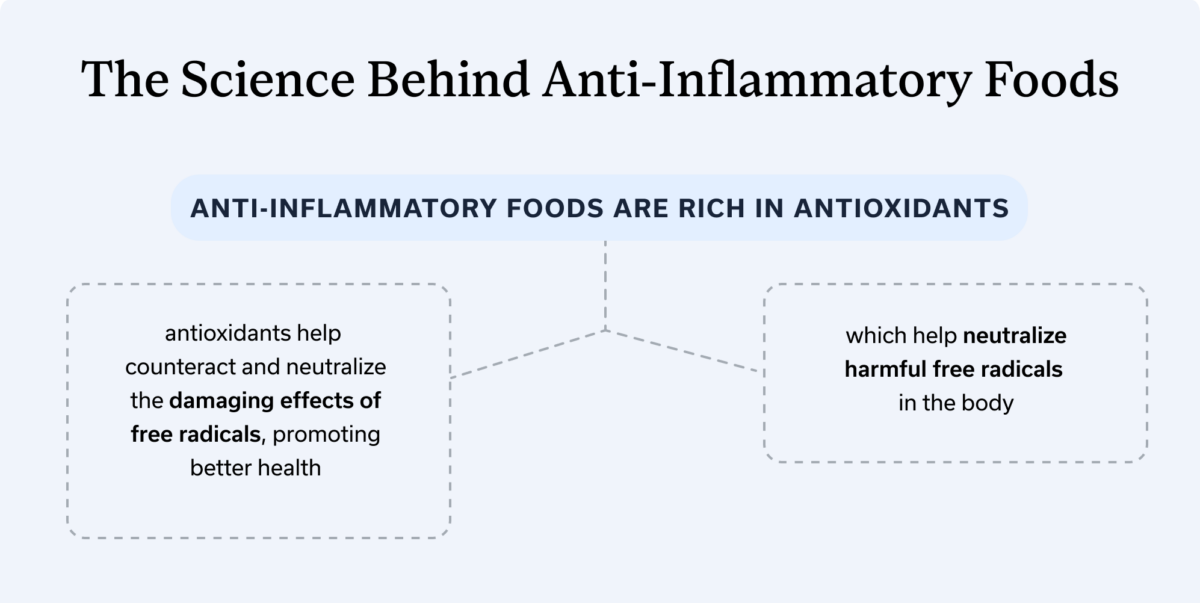
Our cells produce byproducts when they perform their usual functions—for example, converting the foods we eat into usable energy called adenosine triphosphate (ATP). Free radicals are some of those byproducts, and they can be bad for us when they build up. (After all, they are unstable molecules that can cause damage.) Free radical types include reactive oxygen species (ROS) and reactive nitrogen species (RNS).
When we have too many free radicals and not enough antioxidants to keep free radicals in check, we develop oxidative stress, which is a huge contributor to chronic diseases. Oxidative stress can damage our DNA and lead to conditions such as cancer, cardiovascular disease, type 2 diabetes, and neurological disorders. Oxidative stress also contributes to the development of GI conditions, including IBD, and it can disrupt the enteric nervous system (ENT), which is responsible for controlling GI functions.
To make this easier to visualize, I like to think of the old-school game Pac-Man. He’s got to munch on a bunch of mini dots while avoiding four ghosts, right? Think of the mini dots as food in general and the ghosts as free radicals. But remember: The game also has larger dots called “Power Pellets” that give Pac-Man special powers. If Pac-Man eats the Power Pellets, the ghosts turn blue, and Pac-Man can then eat them instead of avoiding them. Basically, anti-inflammatory foods are your Power Pellets. We want to prioritize them as much as possible to counteract those blue-ghost free radicals.
Compounds in food that act as antioxidants
Carotenoids give plant foods their yellow, orange, and red pigments, and some can be converted into Vitamin A. Foods with carotenoids include carrots, some types of squash, and certain peppers.
Polyphenols are compounds that are powerhouses at combating oxidative stress. They include the following types.
- Coumarins are a type of polyphenol found in cinnamon and the stems, roots, and leaves of certain plant foods. Coumarins have neuroprotective properties, meaning they benefit your central nervous system.
- Flavonoids are plant compounds that have anti-diabetic, anti-cancer, neuroprotective, and overall anti-inflammatory properties. There are various types of flavonoids: anthocyanins, flavan-3-ols, flavanols, flavones, flavanones, and isoflavones. Say that five times fast!
- Anthocyanins are pigments in red, blue, and purple berries, and purple grapes.
- Flavan-3-ols are most common in tea, cocoa, berries, grapes, and apples.
- Flavanols are found in kale, onions, broccoli, apples, berries, and tea.
- Flavones are present in herbs, like parsley and thyme, and in celery and hot peppers.
- Flavanones are abundant in citrus fruits.
- Isoflavones are in soybeans, soy milk, tofu, and other soy-based products and in legumes.
- Lignans are polyphenols that have antibacterial, antiviral, and anti-cancer properties. These are found in many plant-based foods, including whole grains, flaxseeds, some beans, and several fruits and veggies.
- Phenolic acids are potent polyphenols found in coffee, tea, fruits, veggies, and whole grains.
- Tannins. These are another type of polyphenol found in wine, tea, cocoa, plums, and more.
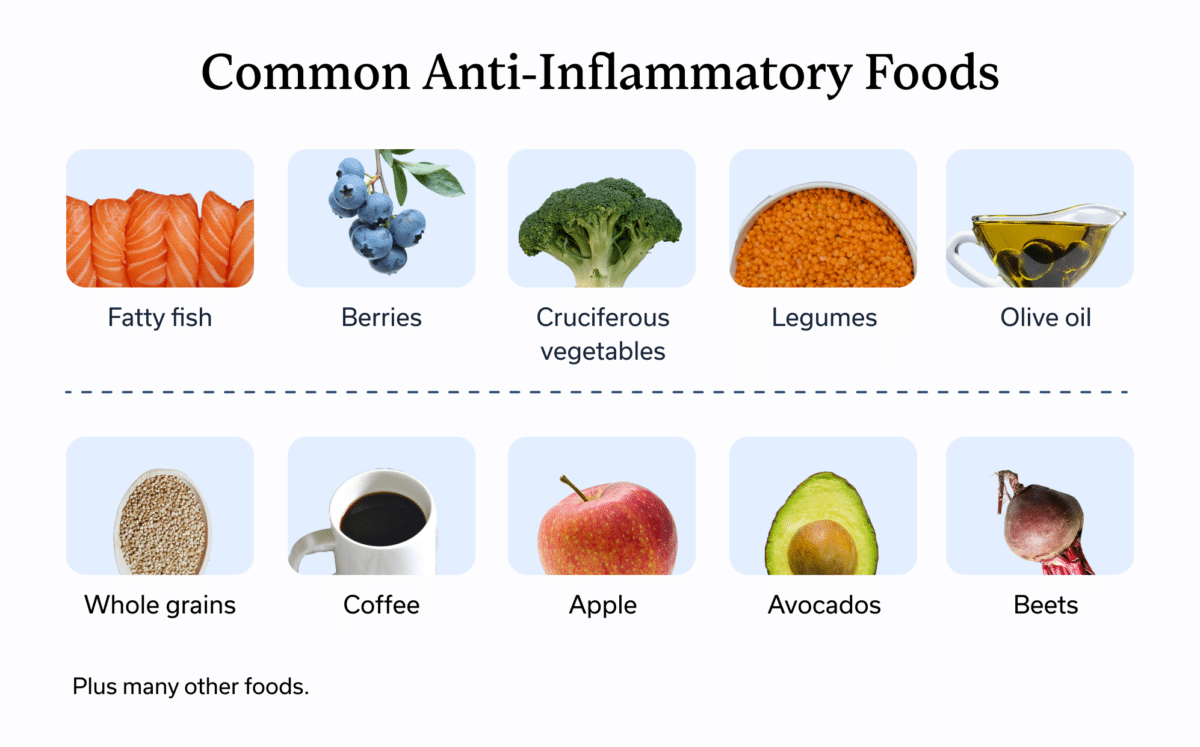
Top 25 anti-inflammatory foods
When thinking about foods that may help to decrease inflammation, you can’t go wrong with fruits and vegetables. All fruits and veggies have a host of antioxidant properties to keep free radicals in check and fight oxidative stress. You’ll also find legumes, spices, nuts and seeds, fatty fish, and whole grains on this list. Note that we’ve organized these foods in alphabetical order, not by any nutritional ranking system (we love them all!).
- Alliums, such as leeks, onions, and garlic
- Apples
- Avocados, which have a host of healthy fats
- Beets
- Berries
- Celery
- Cherries
- Citrus fruits, such as grapefruit, orange, lemon, lime, and more
- Coffee and tea
- Cruciferous vegetables, such as broccoli, cauliflower, Brussels sprouts, kale, arugula, bok choy, cabbage, and more
- Dark chocolate—the darker, the better
- Fatty fish, such as salmon, sardines, mackerel, and anchovies
- Green leafy vegetables, such as kale, chard, spinach, arugula, and more
- Herbs, such as thyme and parsley
- Legumes, such as lentils and beans
- Mushrooms
- Nuts and seeds (aim for raw, rather than roasted) such as almonds, Brazil nuts, walnuts, chia, flaxseeds, pumpkin, and basil seeds
- Olive oil
- Orange vegetables, such as carrots and squash
- Peppers—all kinds, including the hot ones
- Purple vegetables, such as eggplant, cabbage, carrots, potatoes, and more
- Root vegetables, such as parsnips, turnips, Jerusalem artichokes, sweet potatoes, yams, rutabaga, fennel, and more.
- Spices, such as ginger, turmeric, and cinnamon
- Tomatoes
- Whole grains, such as millet, quinoa, oats, farrow, barley, and black, red, brown, and wild rice
Tips for building an anti-inflammatory diet
Now that you know which foods are packed with anti-inflammatory compounds and other benefits, you may wish to include more of them in your diet. Here are a few tips to consider when revamping your nutrition, especially if you have a GI condition.
Focus on whole foods
Anti-inflammatory nutrition plans include foods in their whole or original form, or as close to their original form as possible. This means you should load up your shopping cart with actual fruits and veggies, rather than, say, fruit juices or veggie chips. You can still cook your whole foods as needed.
Watch out for trigger foods
If you’re opting for an anti-inflammatory diet and managing a GI condition, such as irritable bowel syndrome (IBS) or inflammatory bowel disease (IBD), you may have certain food intolerances, or certain foods may trigger your symptoms. For example, if you have gastroesophageal reflux disease (GERD), spicy peppers, although anti-inflammatory, might be on your red-flag list.
Work with a GI registered dietitian
If you aren’t sure of your potential trigger foods—or if you just want guidance and support regarding nutrition and gut health—working with a GI registered dietitian, like those at Oshi Health, can help. They’re specialized in tailoring a diet to your individual needs and preferences, including incorporating foods that align with your culture.
Meet Oshi's GI registered dietitians
Looking for tailored dietary support?
At Oshi, our registered dietitians have advanced training and extensive experience in treating gastrointestinal (GI) issues. Working with your GI provider and gut-brain specialist, they’ll help you get to the bottom of digestive symptoms and find real, lasting relief.
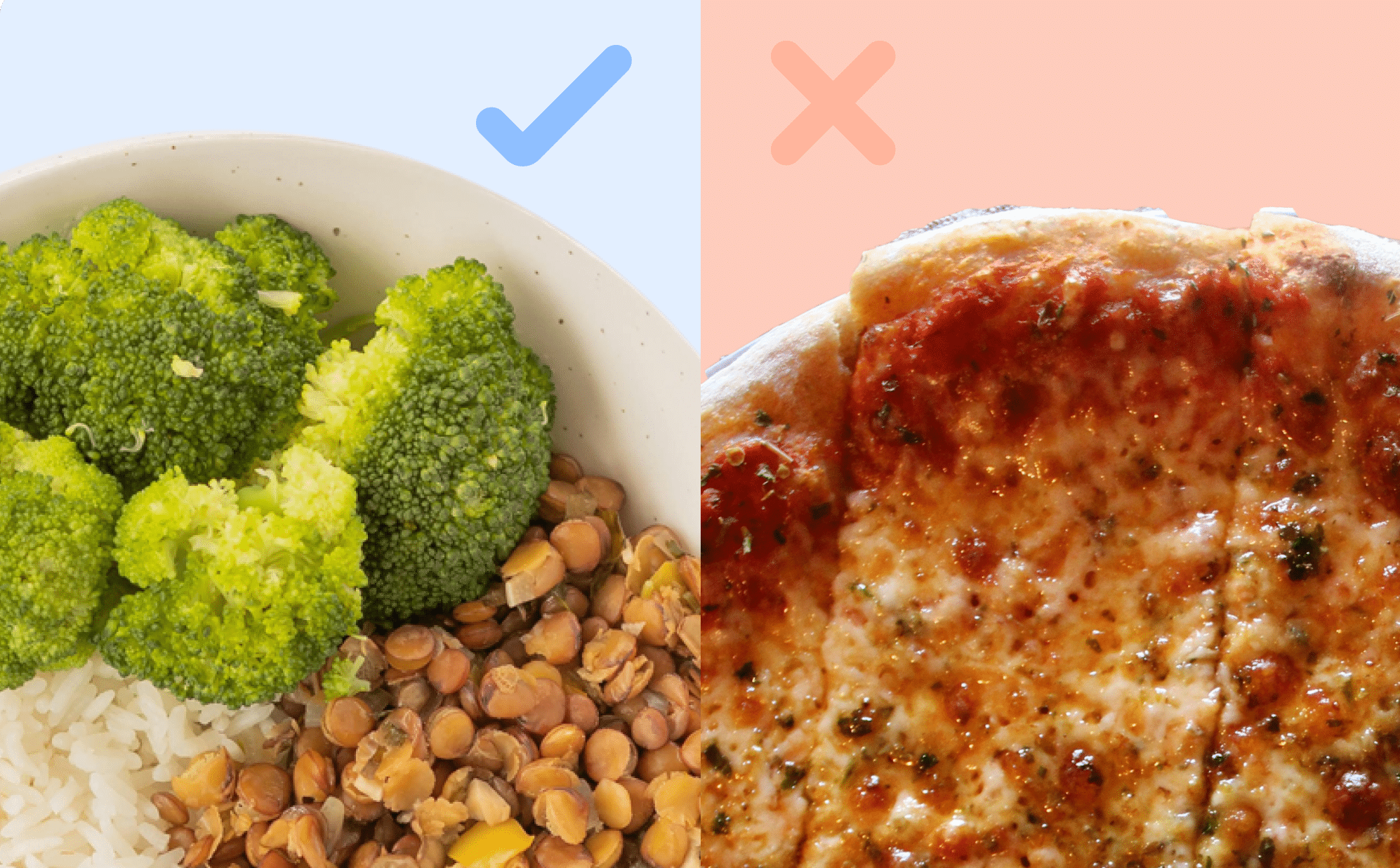
Focus on adding in foods
Optimizing your diet to be more anti-inflammatory can feel overwhelming. But instead of focusing on what to eliminate, focus on what to add. By adding more fruits, veggies, fatty fish, legumes, whole grains, and your favorite herbs and spices, you will naturally start to eliminate some foods that are inflammatory.
For example, I love berries, and I find that when I eat them regularly, I don’t have cravings for processed sweets. Nuts are also great to reach for when I get a hankering for the crunch factor. Grabbing a handful of almonds makes me less likely to reach for chips or crackers.
GI experts recommend eating a variety of these anti-inflammatory foods to reap the most benefits. You’ll also be loading up on micronutrients (vitamins and minerals) that are important for gut health. Consuming anti-inflammatory foods helps you eat a more favorable macronutrient profile, as well.
The three macronutrients are carbohydrates, fats, and protein. And your macronutrient profile involves the percentage of calories from each category. When you eat anti-inflammatory foods, you’re prioritizing fiber-rich carbohydrates, healthy fats, and lean protein, which helps lessen the chances that you’re eating empty calories, those without nutritional benefits.
Foods to avoid that promote inflammation
Of course, being mindful of which foods drive inflammation can help you reduce their presence in your diet, too. You can aim to reduce or eliminate your intake of:
Ultra-processed foods
Ultra-processed foods that are high in sodium, added sugar or gums, and flavor-enhancing and shelf-life-preserving chemicals can promote inflammation. Eliminating these from your diet as much as possible can help reduce inflammation and help you feel better. As for processed foods like frozen veggies or canned beans, those can help support your overall gut health.
Processed meats
Processed meats include those that have been preserved through curing, salting, or smoking. That means bacon and packaged ham, turkey, chicken, bologna, and more. Processed meats contain nitrites and nitrates; these naturally occurring compounds aren’t harmful on their own, but when exposed to high temperatures and then consumed, they can promote the growth of cancerous cells.
Red meat
The occasional consumption of lean red meat likely isn’t harmful. However, higher intake of red meat may have associations with higher levels of inflammatory biomarkers.
Refined carbohydrates
Refined carbohydrates—like white bread and rice—are carbs in which the beneficial fiber, protein, and other nutrients have been stripped out and you’re left with a highly processed carb that will likely spike your blood sugar and drive inflammation. However, keep in mind that many refined carbohydrates are fortified with vitamins and minerals, meaning the manufacturer has added in these nutrients. Plus, sometimes refined carbohydrates are easier to digest for people who have GI conditions or when they are experiencing a flare.
Added sugar
We’d never tell you to skip the occasional sweet treat. But even though humans don’t need added sugar to survive, many processed foods contain high amounts of it—especially in the form of high-fructose corn syrup. Overconsumption of sugar negatively impacts the immune system and causes inflammation.
Fried foods
We need more research into whether processed seed oils—such as canola, corn, sunflower, cottonseed, safflower, soybean, grapeseed, rice bran, and peanut oils—are problematic long-term. But existing research suggests they may lead to oxidative stress.
These oils are high in omega-6 fatty acids, which can drive inflammation. Omega-3 fatty acids, on the other hand, are anti-inflammatory. When we eat more omega-6 than omega-3 fatty acids, inflammation can ensue, so eating a lower ratio is better. In other words, eat those fatty fish and nuts and seeds, and reduce your intake of processed seed oils. For cooking or seasoning, stick to olive and avocado oil as much as possible.
Key takeaways
- Although inflammation in the short term can be a good thing for fighting off an infection or healing an injury, chronic inflammation is lasting and can lead to a host of chronic diseases.
- We can combat chronic inflammation by eating anti-inflammatory foods, which are loaded with antioxidants.
- Antioxidants help reduce the build-up of harmful free radicals that can lead to damage and health issues.
- Part of eating an anti-inflammatory diet also means reducing intake of inflammation-causing foods, such as ultra-processed items and those with added sugar. For help with building an anti-inflammatory diet, Oshi Health’s GI registered dietitians and other GI providers can help.
FAQ
-
The strongest anti-inflammatory foods are fruits and veggies, nuts and seeds, fatty fish, and coffee and tea. These all contain beneficial plant compounds that fight oxidative stress.
-
Some studies show drinking coffee and/or tea in moderation might reduce inflammation. Another excellent option is tart cherry juice.
-
You can’t “flush” inflammation from your body since it’s an important function of your immune system. However, you can eat an anti-inflammatory diet to help reduce chronic inflammation, which is linked to chronic disease. Anti-inflammatory foods include fruits and vegetables and those that contain omega-3 fatty acids. Check out the list in this article.
Oshi is your partner in digestive health
Feel like your digestive concerns are running your life? You’re not alone—and we’re here to help you find lasting relief.
Oshi Health GI providers, gut-brain specialists, and registered dietitians work together to address the root cause of your symptoms and find solutions that actually work for you.
Whether you’re dealing with chronic digestive issues or unpredictable symptom flare-ups, our GI specialists deliver:
✔ Personalized care plans tailored to your lifestyle
✔ Science-backed strategies to calm your gut
✔ Compassionate, whole-person care
✔ And so much more!
Ready to take control of your gut health?