GERD Overview
GERD Overview
Gastroesophageal reflux disease (GERD) is a chronic condition in which the contents of your stomach flow back (reflux) into your food pipe (esophagus).
This backflow action usually happens because of issues with the lower esophageal sphincter. This muscle valve separates your stomach and esophagus, managing the flow of food and liquid through the upper part of the digestive tract.
Because the contents of your stomach include stomach acid, a backward flow can irritate the lining of your lower esophagus, leading to uncomfortable symptoms like heartburn and acid reflux.
Read on to learn about GERD symptoms, causes, risk factors, and complications—and how we can help you find relief!
GERD symptoms
Wondering if your symptoms might be GERD or looking to better understand your condition? Let’s explore some of the signs of gastroesophageal reflux disease (GERD) and get you the answers you need, whether you’re newly concerned or already have a diagnosis.
Heartburn is one of the most common GERD symptoms. It can feel like a burning sensation in the middle of your chest, rising into your throat.
Another common GERD symptom is regurgitation. This is when stomach contents flow back through your food pipe into your mouth or throat. You might taste stomach acid or food when it occurs.
Other symptoms of GERD include:
- Nausea or vomiting
- A bad taste in the mouth
- A sensation of a lump in your throat
- Upper stomach or chest pain
- Difficulty or discomfort when swallowing
- Sore throat
- Chronic cough
- Wheezing
- Hoarseness
Living with GERD symptoms can be uncomfortable, but it’s important to know that you’re not alone. In fact, experts estimate that almost a third of U.S. adults live with GERD.
At Oshi Health, our GI specialists, including GI providers, registered dietitians, and gut-brain specialists, work together to address your GERD symptoms.
What causes GERD?
Whenever you eat or drink, swallowing triggers your esophageal sphincter to relax and let food into your stomach—think of it like the doorman to your stomach. When you’re not busy enjoying a meal, the sphincter is supposed to stay closed, keeping stomach contents from taking a return trip.
In people with GERD, the sphincter relaxes when it’s not supposed to or becomes weak over time, leading to annoying bouts of heartburn and reflux.
Causes of GERD include:
- Regularly eating large meals or overeating. This can cause your upper stomach to become distended, putting pressure on your lower esophageal sphincter.
- Frequently lying down right after eating. While a quick nap after eating sounds like a good time, lying down right after mealtime can impact sphincter function, weakening it over time.
- Having a hiatal hernia. A hiatal hernia develops when the stomach pushes above the diaphragm. It can cause problems with your esophageal sphincter.
- Eating certain foods. Spicy, acidic, and high-fat foods and beverages containing caffeine can trigger GERD symptoms.
- Drinking alcohol and smoking. Both can increase esophageal irritation and worsen your symptoms.
- Taking certain medications. Some medications can cause the esophageal sphincter to relax, making GERD worse.
Additionally, factors like stress (hello, gut-brain connection) can make your GERD symptoms worse.
GERD risk factors
Just because you have a risk factor doesn’t mean you’re destined to get GERD, but it can mean you’re more likely to develop the condition than someone else.
GERD risk factors include:
- Using tobacco products or exposure to secondhand smoke
- Being higher weight
- Being pregnant
- Being over 50
- Eating a low-fiber diet
- Eating a high-sugar diet
- Certain medical conditions
- Having a sedentary lifestyle
- Alcohol use
Research also suggests a link between GERD and depression—which is why a gut-brain specialist can be an important resource.
GERD complications
Before we dig into this scary stuff, we want to make sure you know that just because you have GERD doesn’t mean you’ll develop complications. Addressing and managing your symptoms can make you less likely to experience serious side effects.
Over time, untreated chronic reflux can damage the lining of your esophagus, leading to serious GERD complications like:
- Breathing issues. When stomach contents flow back into the esophagus, they can sometimes enter the lungs, increasing your risk of respiratory infections and breathing problems.
- Esophagitis. Inflammation of the esophagus can be mild or severe. In severe cases, tissue may be so inflamed that it leads to narrowing of the esophagus or GI bleeding.
- Barrett’s esophagus. This condition occurs when the tissue in your esophagus goes through a process known as intestinal metaplasia. The tissue starts to look more like the lining of your intestines than your esophagus. People with Barrett’s esophagus are at higher risk of developing esophageal adenocarcinoma, a rare form of esophageal cancer.
- Esophageal cancer. Most people who have GERD don’t develop cancer of the esophagus. But your esophageal cancer risk is slightly higher if you have frequent GERD symptoms, according to the American Cancer Society.
How is GERD diagnosed?
The first step toward a GERD diagnosis is a thorough medical history. At Oshi Health, our GI specialists consider the whole you when working together to make a diagnosis, including your medical history, symptoms, and lifestyle.
Your provider will ask you questions about your symptoms, like when, how often, and for how long they typically occur or whether certain foods or behaviors tend to make them worse.
They’ll also consider the following:
- Your diet and potential trigger foods
- Lifestyle habits
- Medications or supplements you’re taking or have already tried for your symptoms
- Stress and behavioral health
- Previous surgeries or medical procedures
- Your family history, including whether any close relatives have had Barrett’s esophagus or esophageal cancer
And while you don’t need to have had previous testing to meet with an Oshi provider and benefit from our integrated GI care, your provider will review any previous testing you’ve gone through, if any.
GERD can often be diagnosed based on your symptoms. However, your GI provider may recommend additional testing if you have a combination of risk factors or serious symptoms like:
- Problems swallowing
- Pain when swallowing
- Unexplained weight loss
- Anemia
- Blood in your vomit or stool
Further testing might include:
- An ambulatory 24-hour pH probe involves inserting a tube outfitted with a pH sensor through your nose into your esophagus. It measures the amount of acid flowing backward into your esophagus over 24 hours. monitoring
- An esophagram involves drinking a special barium solution and getting an X-ray of the upper digestive tract to check for anything unusual.
- An esophageal manometry involves passing a flexible tube through your nose into your esophagus to determine the strength of your esophageal muscles. Weakness can indicate GERD.
- An upper endoscopy involves inserting a thin tube with a very small camera into your esophagus to check for tissue damage that might indicate chronic reflux. In some cases, the healthcare professional performing the exam may take a tissue biopsy during the procedure.
At Oshi Health, we take the time to listen to avoid putting you through unnecessary testing—diagnosing and addressing symptoms based on our detailed knowledge of the whole you.
GERD treatment
We take a comprehensive approach to GERD treatment, addressing not just your symptoms but also putting you on a path to better digestive health. Here’s an example of what treatment can look like when GERD symptoms overlap with other digestive concerns, and how our team works together to provide comprehensive, personalized care.
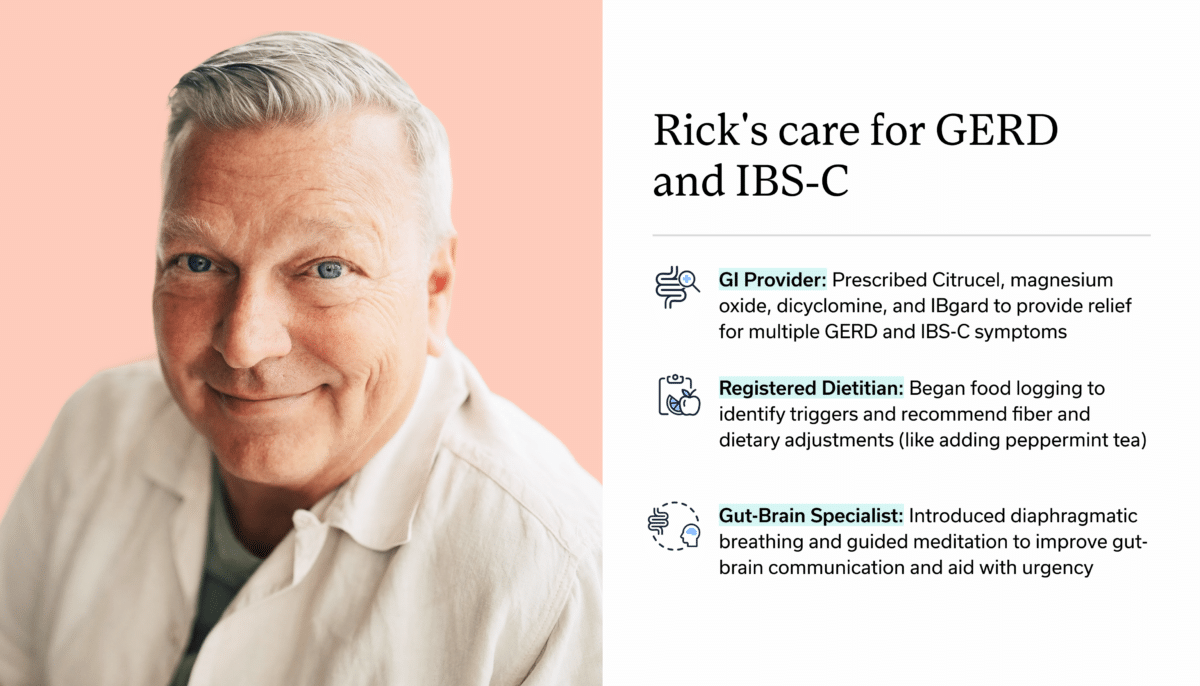
Here’s what our care entails:
1. Identifying GERD triggers & making dietary and lifestyle adjustments
What does your typical diet look like? Do you have dietary triggers that seem to make your symptoms worse?
Our registered dietitians will help you identify your GERD-trigger foods and find ways to modify your diet without necessarily giving up the foods you love.
Depending on what triggers GERD symptoms for you, management might also involve lifestyle changes, including:
- Avoiding eating 2-3 hours before lying down
- Sleeping with your head elevated to prevent reflux symptoms at night
- Hydrating properly
- Adjusting your meal portion sizes
- Eating smaller, more frequent meals
- Avoiding tight-fitting clothing
- Avoiding tobacco and alcohol use
- Maintaining a healthy weight for you
2. Working on the gut-brain connection
Did you know your brain and digestive system are in constant communication? It’s why you might feel nauseous when you experience heightened emotions like stress or excitement.
The close link between your GI system and mind can also play a role in conditions like GERD.
Our gut-brain specialists can help you identify potential stress-related triggers causing excess acid production.
Gut-brain specialists are trained and licensed behavioral health professionals with specific experience treating GI concerns like GERD. Working alongside GI providers and registered dietitians, they can help you take control of your symptoms by providing you with the skills and tools to cope with distressing thoughts, feelings, and physical reactions that may be contributing to GI distress.
They can also help you work on how to talk about your GERD with the people in your life. Read our guide for tips on having conversations about your digestive condition.
Some examples of common therapeutic gut-brain approaches include:
- Diaphragmatic breathing exercises
- Guided imagery and visualization
- Mindfulness meditation
- Cognitive behavioral therapy (CBT) for GI symptoms
- Gut-directed hypnotherapy (GDH)
Oshi Health gut-brain specialists are here to support you as you navigate living with a chronic digestive health condition, helping to normalize and validate your GI-related concerns—so you never feel alone in your journey to symptom relief.
3. Prescribing or recommending medications
Medications are just one piece of the journey to symptom relief. Our whole-person approach to GI care looks at lifestyle factors such as diet and stress that may be contributing to symptom flares. Depending on your unique needs, medications may be a part of your personalized treatment plan.
Typical medications used to treat GERD include:
- Antacids. These over-the-counter (OTC) medications can help treat mild reflux and heartburn symptoms.
- Proton pump inhibitors (PPIs). PPIs reduce stomach acid production, helping to heal the lining of your esophagus. They’re available over the counter and by prescription.
- H2 blockers. Similar to PPIs, H2 blockers are another option for reducing stomach acid. Your provider may recommend them if your GERD symptoms tend to strike at night or only occasionally.
- Alginate therapy. Alginates are found in certain types of brown seaweed. And it turns out seaweed isn’t just for sushi! While not as effective as H2 blockers and PPIs, this natural treatment option combines with the acid in your stomach to create a gel-like barrier that prevents acid from rising into your esophagus.
- Sucralfate. This medication forms a protective shield for the lining of your stomach and esophagus. It’s not typically the first choice for GERD, but your provider might recommend it if you’re pregnant or trying to become pregnant.
- Potassium-competitive acid blockers (PCABs). These work similarly to PPIs, but act faster and don’t need to be activated by stomach acid. The effects of PCABs may also last longer, even if you take them after eating. If you don’t respond well to PPIs, your provider might recommend a PCAB.
4. Whole person care for GERD
At Oshi Health, no two treatment plans are the same.
Our GI specialists work together to create a personalized treatment plan to address your symptoms. We consider the whole you—not just your GERD. That means taking into account diet, lifestyle, and the gut-brain connection, ensuring you get the individualized care you need.
Already seeing a GI provider? We can provide support between visits and work with your existing gastroenterologist as an extension of your care.
- decrease in unnecessary (and expensive) procedures and tests
- of undiagnosed patients get a clear diagnosis within 3 months
- of patients report better quality of life, with less stress and anxiety, within 3 months
Source: Results of a clinical trial conducted in partnership with a national health plan
Oshi is your partner in digestive health
Feel like your digestive concerns are running your life? You’re not alone—and we’re here to help you find lasting relief.
Oshi Health GI providers, gut-brain specialists, and registered dietitians work together to address the root cause of your symptoms and find solutions that actually work for you.
Whether you’re dealing with chronic digestive issues or unpredictable symptom flare-ups, our GI specialists deliver:
✔ Personalized care plans tailored to your lifestyle
✔ Science-backed strategies to calm your gut
✔ Compassionate, whole-person care
✔ And so much more!
Ready to take control of your gut health?
Frequently Asked Questions
-
Many factors can trigger GERD symptoms, including spicy, acidic, and high-fat foods, beverages with caffeine or carbonation, large meals, eating before bed, and stress.
-
GERD is a chronic condition. Whether you have mild, moderate, or severe GERD and any underlying conditions will determine how long it takes to heal with treatment.
GERD symptoms like reflux and heartburn can last for a few minutes or several hours.
-
Trouble getting Zzz’s because of nighttime heartburn and reflux? It can help to sleep on your left side, according to research. Other ways to prevent bedtime GERD symptoms include avoiding eating too close to bedtime and keeping your head elevated.
Last medically reviewed October 2025