Bowel movements aren’t exactly fun, but they shouldn’t be painful either. If you’ve experienced pain when going number two or have irritation or itching in the region, you may have swollen hemorrhoids. But what causes hemorrhoids, are they treatable, and can you prevent them? We’re about to answer all these questions and more about hemorrhoid symptoms and treatment options.
Hemorrhoids occur when the veins around the anus and rectum swell and become inflamed, causing itching and pain in the region. Understandably, they aren’t a topic we often talk about, though they are extremely common. About one in twenty Americans will experience inflamed hemorrhoids in a given year, though that number goes up to 50 percent for those over 50.
Because they’re a bit of a TMI for most face-to-face convos, there are a lot of questions circulating about them online: What causes hemorrhoids? Which symptoms are typical? And, perhaps most importantly, how do you get rid of hemorrhoids? This article is a place to explore these questions and go into all the nitty-gritty details about this uncomfortable, yet highly treatable, gastrointestinal (GI) issue.
What are hemorrhoids?
Technically, we all have hemorrhoids. While we often think of hemorrhoids as a bad thing, they’re actually just part of our anatomy. “Everyone in the world has hemorrhoids,” says Kyle S. Eldredge, DO, a surgeon specializing in colorectal surgery and hemorrhoids, “which are basically just, for lack of a better term, what we call vascular cushions.” These cushions have a very important job: they help us hold in stool so we can put off bowel movements until we get to the toilet.
Yet when we talk about hemorrhoids outside of an anatomy class, we’re often referring to when these blood vessels, located in the lower part of the rectum and the anus, become inflamed. (And because this isn’t a medical textbook, we’ll refer to swollen hemorrhoids as just”hemorrhoids” from here on out to avoid any confusion.)

Another fun fact: Not all hemorrhoids are the same. There are actually two different types: internal and external hemorrhoids. External hemorrhoids form under the skin on the outside of the anus and cause pain, itching, and difficulty with anal hygiene, though this type won’t cause bloody poop.
Internal hemorrhoids are more common and result in quite a few symptoms: itching, bloody bowel movements, burning, swelling, a white or yellow jelly-like discharge from the anus, and difficulty with anal hygiene. These symptoms usually occur when the hemorrhoids prolapse, which is when an inflamed hemorrhoid falls through the anal opening. Less severe prolapses can be pushed back inside the anus by hand, while more severe ones cannot and are more likely to be accompanied by anal bleeding.
| Internal hemorrhoids | External hemorrhoids | |
| Location | The lining of the anus and rectum | Under the skin around the anus |
| How they feel | Only painful, burning, or itching if prolapsed | Often painful, irritating, or burning |
| What they look like | Not usually visible, though a prolapsed internal hemorrhoid can bulge out from the anal opening | Often seen as lumps around the anus |
| Likelihood of rectal bleeding | Bright red stool or blood on toilet paper is likely during bowel movements | Sometimes (when irritated, inflamed, or if they become thrombosed) |
What causes hemorrhoids?
Doctors aren’t actually sure what causes hemorrhoids, though they’re associated with more pressure than usual around the anus and the lower rectum’s blood vessels. Dr. Eldredge states that he often sees hemorrhoids in patients with chronic constipation or straining bowel movements.
“As you’re bearing down or straining to have these bowel movements, you’re basically increasing the pressure down in the pelvis and especially down in the anus,” explains Dr. Eldredge, “What happens is the blood kind of gets stagnant there, and instead of having the natural flow, that stagnant blood pools and, over time, those hemorrhoids enlarge and become symptomatic.”
However, some of Dr. Eldredge’s patients with hemorrhoids report that they are not constipated. They even have regular bowel movements without any straining. Upon further discussion, these patients reveal they’re sitting on the toilet for 30 minutes, even though they finish much quicker. “And being in that sitting stance on the toilet can increase the pressure,” explains Dr Elderedge.
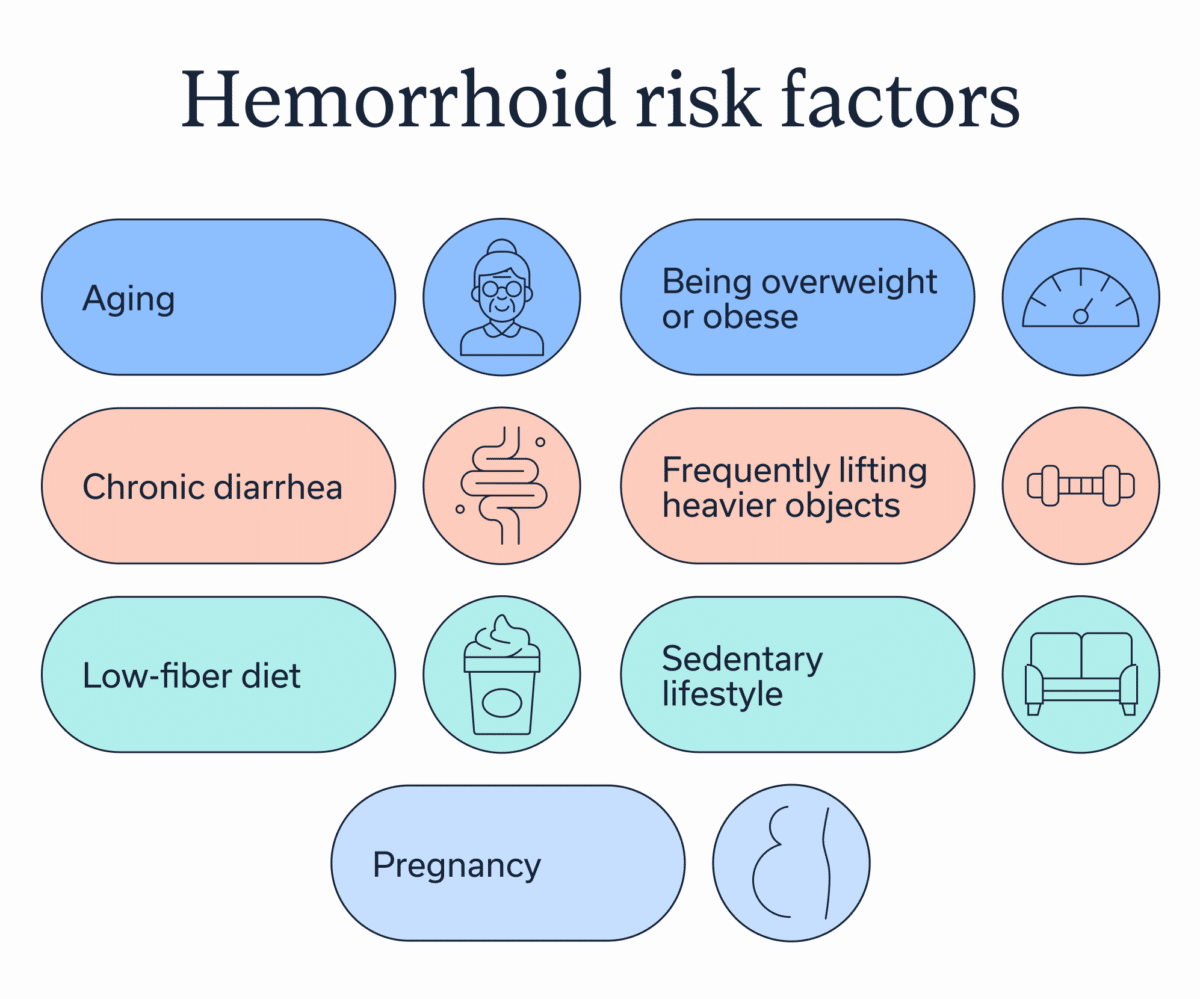
Besides straining and sitting too long on the toilet, many other lifestyle decisions and health factors may put hemorrhoids into a metaphorical pressure cooker:
- Aging, which causes anal and rectal tissues to weaken
- Being overweight or obese
- Chronic diarrhea, since frequent bowel movements irritate the anal area
- Frequently lifting heavier objects
- Low-fiber diet
- Sedentary lifestyle
- Pregnancy
Everyday habits that make hemorrhoids worse (or more likely)
The chance of developing hemorrhoids is highly influenced by what we do day to day. Everyday habits that make hemorrhoids more likely, or worse if they are already occurring, include:
- Dehydration: I’m a runner, meaning I live by the phrase”hydrate or die.” When it comes to avoiding hemorrhoids or preventing them from getting worse, that’s also a good motto. That’s because dehydration is associated with more strained bowel movements and even constipation.
- High BMI: Being overweight or obese places extra pressure on the anus and rectum. In fact, an increase in body max index (BMI) increases the risk of hemorrhoids by 3.5 percent.
- Low-fiber diet: Fiber may be the most underhyped food group. It cleans out your gut and makes stool softer, meaning it can leave the body with more ease. Not getting enough fiber increases the risk of and worsens hemorrhoids.
- Sitting on the toilet for a long time: When we sit on the toilet for longer than necessary, it increases pressure on the veins in the rectum and anus. Take this as a sign to say goodbye to reading or scrolling on the toilet, especially after you’ve gone number two.
- Too much or too little physical activity: If someone already has hemorrhoids, there’s a Goldilocks sweet spot for how much they should exercise. A sedentary lifestyle worsens hemorrhoids, but so does strenuous physical exercise, especially if it involves heavy weights (though cycling, rowing, and horseback riding also place pressure on the anus and rectum). Exercises that won’t worsen pressure on these areas include walking, swimming, and yoga.
Diagnosis and treatment options
If you decide to seek medical care for your hemorrhoids, you’ll want to visit a gastroenterologist or other GI provider. In an initial appointment, they’ll ask about your medical history, with specific emphasis on your symptoms and associated lifestyle habits like bowel patterns and diet.
They’ll also conduct a physical exam, which can reveal any:
- Anal fissures, which are small tears in the anus
- Blood clots, also known as thrombosed hemorrhoids, usually external
- Lumps
- Mucus or stool leakage
- Prolapsed internal hemorrhoids
- Skin irritation
- Skin tags
- Swelling
While the physical exam and medical history are often enough to diagnose external hemorrhoids, internal ones sometimes require a digital rectal exam. Despite the name, it doesn’t involve any tech; instead, a GI provider inserts a gloved, lubricated finger into the rectum, feeling for anything that’s off or different than expected.
When hemorrhoids are to blame, the GI provider will then create a tailored treatment plan. Often, this starts with at-home treatments, medication, and in-office treatments, moving to surgical options only if other options don’t work.
If another condition is suspected, the GI provider may order additional tests, most commonly a colonoscopy, which screens for colon cancer and other irregularities in the colon. You can think of this like choosing the scenic route on the GPS: it’s not always necessary, but it provides a more holistic view of your GI health.
Non-medical treatment options: How to treat hemorrhoids at home
Hemorrhoids can sometimes be treated at home via a mix of lifestyle changes and over-the-counter medications.
Common lifestyle changes are:
- Fiber: More high-fiber foods on your plate, such as whole-grain cereals, whole-wheat bread and pasta, nut butters, apples, broccoli, green leafy vegetables, and nuts, can help facilitate less strained bowel movements.
- Better bathroom habits: Try to strain less and sit on the toilet for less time. And, respond ASAP when you feel the urge to go.
- Hydration: Stay hydrated, though exact hydration recommendations vary based on age, gender, activity level, and outdoor temperature.
- Warm baths: Take sitz baths, which are warm water soaks, to help soothe pain.
- Avoid triggers: Steer clear of anything that triggers pain or discomfort in the anal region, like harsh wipes or soaps.
Over-the-counter options include:
- Topical creams: Hemorrhoid topical creams are applied to the region to treat specific symptoms, such as pain or itching.
- Suppositories: These are inserted inside the rectum and treat hemorrhoids.
- Pain relievers: These can be used in the short-term if recommended by a provider.
Medical treatment options for hemorrhoids
When at-home measures and OTC medications don’t cut it, a healthcare provider may recommend an office-based treatment. There are four main office-based procedures for hemorrhoids. All of them aim to cut off the blood supply to the hemorrhoid.
- Rubber band ligation: A doctor places a special rubber band around the hemorrhoids base to cut off blood supply. The banded part then shrivels up and falls off, usually within a week. These rubber bands aren’t like the ones you’ll find in your home, and this shouldn’t be attempted at home since it can cause scarring.
- Sclerotherapy: A GI provider inserts a solution into the anus, which scars the tissue, cutting off the blood supply to the hemorrhoid.
- Infrared photocoagulation: A doctor inserts an infrared light into the anus, causing the tissue to scar and the blood supply to be cut off.
- Electrocoagulation: A provider uses an electrical current to scar internal tissue, cutting off the blood supply and causing the hemorrhoid to fall off.
For more severe or complicated cases, surgery may be required. These are usually outpatient surgeries, meaning you can go home afterwards. These are a last resort for hemorrhoids that don’t respond to other treatments or are particularly large.
“Although I’m a colorectal surgeon, surgery is actually one of the last things that I recommend,” says Dr. Eldredge. He points out that most cases resolve with lifestyle changes, medications, and/or in-office procedures.
In the rare cases where surgery is required, there are two effective types:
- Hemorrhoidectomy: When a surgeon removes a large external hemorrhoid or a prolapsed internal hemorrhoid.
- Hemorrhoid stapling: When a provider uses a special stapling tool to pull an internal hemorrhoid back in or to remove it.
When it might not be”just hemorrhoids”
There’s no denying that hemorrhoids are uncomfortable, but they are also highly treatable. That doesn’t mean they aren’t without their complications:
- Bleeding from a hemorrhoid may result in anemia, a condition where someone feels extremely tired due to a lack of red blood cells.
- External hemorrhoids may cause sores that may become infected.
- External hemorrhoids may lead to blood clots. When a blot clot dissolves, it can leave behind extra skin called a skin tag.
- When a prolapsed internal hemorrhoid is cut off from its blood supply, it may become extremely painful (a condition known as a strangulated hemorrhoid).
And complications aren’t the only risk. Hemorrhoid symptoms overlap with many other conditions, including anal fissures, polyps, colon cancer, and inflammatory bowel disease (IBD). That means if hemorrhoids don’t go away after a week or so of at-home treatment, a GI provider probably needs to be looped in. They can diagnose an official cause, which may or may not be hemorrhoids.
When to seek care
As mentioned above, if you suspect hemorrhoids and symptoms haven’t gone away after a week of at-home treatment, you should schedule a visit with a GI provider. You can either ask your primary care doctor for a referral or work with a provider like Oshi Health, which offers virtual appointments with a GI care team.
No matter who your provider is, it’s important to share everything — and I mean everything. Your GI provider has seen all the GI symptoms, and the more you share, the more effective the treatment plan can be.
You also shouldn’t wait too long. Dr. Eldredge mentions that he sometimes sees patients who have had symptomatic hemorrhoids for 20 years before they make an appointment. “If someone is having issues, don’t be afraid to talk to the primary care doctor, gastroenterologist, or general or colorectal surgeon,” advises Dr. Eldredge, “Because the longer they wait, the more painful and the worse they can get.”
You should call a provider immediately or head to the emergency room if hemorrhoids are accompanied by:
- Heavy anal bleeding, especially if you notice black tarry stools
- High fever
- Anemia symptoms, such as dizziness or shortness of breath
- Severe anal or abdominal pain
Preventing hemorrhoids and flares: Everyday strategies
Odds are, many people will experience hemorrhoids at one point or another. But that doesn’t mean there aren’t effective prevention strategies:
- Establish regular bathroom routines. Especially ones that don’t involve sitting on the toilet for long periods.
- Get enough fiber. This is usually defined as 21-38 grams per day.
- Stay hydrated. My cross-country coach used to say you’ve reached the “hydration station” when your pee is pale or clear; darker yellow pee typically indicates dehydration.
- Stay active. A good weekly minimum is 150 minutes of cardio and two strength training sessions.
- Eat a diet that helps you maintain a healthy weight. This might include plenty of veggies, fruits, lean protein, whole grains, and legumes.
- Treat any other GI conditions. Other GI concerns, like constipation and diarrhea, can make hemorrhoids worse. Treatment can help you find relief.
Final thoughts
- Hemorrhoids are a common GI condition. They are caused by increased pressure on the veins inside or outside of the anus and lower rectum.
- Hemorrhoid symptoms include a burning or painful sensation, especially when sitting or during a bowel movement. They can also lead to itching or irritation around the anal opening, skin tags, mucous discharge, and rectal bleeding.
- Many cases go away with at-home and over-the-counter treatments, though it’s important to see a GI provider if hemorrhoids don’t disappear within one week. They can cause complications, and symptoms are similar to those of other GI conditions.
- A GI provider like Oshi Health can diagnose what’s causing your symptoms and can develop a comprehensive, personalized treatment plan. At Oshi, we approach gut health from every angle, meaning you have access to GI providers, dietitians, and gut-brain specialists as needed.
Frequently asked questions (FAQs)
-
Hemorrhoids are triggered by pressure on the veins in and around the anus and lower rectum. Many factors may cause this pressure, including being overweight or obese, aging, pregnancy, straining or sitting on the toilet for too long, and chronic constipation or diarrhea.
-
Most of the time, hemorrhoids go away with at-home measures, such as eating more fiber, hydrating, and taking warm baths, and over-the-counter hemorrhoid medications. If these don’t work, office treatments to cut off blood supply to the hemorrhoids may be required. In rare cases, surgery may be necessary.
-
No one knows the exact cause of hemorrhoids, though they seem to stem from increased pressure in the lower rectum and anus. Many factors may increase pressure in this region, including straining on the toilet for too long, chronic constipation, aging, lifting heavy objects, being overweight or obese, and pregnancy.
-
If you suddenly have hemorrhoids, something is probably increasing pressure on the anus and lower rectum. Possible causes include straining or sitting on the toilet for too long, frequently lifting heavy objects, pregnancy, a low-fiber diet, chronic constipation, aging, or being overweight or obese.
-
Hemorrhoids cannot directly cause diarrhea. If experiencing both, it may be due to an underlying gastrointestinal condition, such as an inflammatory bowel disease. Chronic diarrhea, however, can irritate the anus and lower rectum, contributing to hemorrhoids.
Oshi is your partner in digestive health
Feel like your digestive concerns are running your life? You’re not alone—and we’re here to help you find lasting relief.
Oshi Health GI providers, gut-brain specialists, and registered dietitians work together to address your symptoms and find solutions that actually work for you.
Whether you’re dealing with chronic digestive issues or unpredictable symptom flare-ups, our GI specialists deliver:
✔ Personalized care plans tailored to your lifestyle
✔ Science-backed strategies to calm your gut
✔ Compassionate, whole-person care
✔ And so much more!
Ready to take control of your gut health?