People with chronic GI illness like inflammatory bowel disease (IBD), irritable bowel syndrome (IBS), or Gastroesophageal Reflux Disease (GERD) know that dietary changes can help them. It’s quite another thing to change one’s diet day-by-day. Read on to learn more about the life-changing potential of nutritional dietary support.
Without the continuous support of a registered dietitian or GI specialized health coach, most people resolve to interpret and implement their own restrictive (high fiber! dairy free! low acid!) versions of diets. They’re likely to self-eliminate critical nutrients, or unnecessarily sacrifice some of the very foods that may bring them great enjoyment.
Meanwhile, with poor understanding of offending foods, people’s unpredictable and uncomfortable GI symptoms escalate, causing further distress and anxiety. And of course, stress in itself is a trigger for still more GI symptoms.
The resulting toll on mental health is no surprise. Years of discouragement, plus failed attempts at highly complex food elimination and reintroduction diets can create a highly complicated and often negative relationship with food.
The diet & nutrition aspect of managing chronic GI illness goes beyond following a specific diet—it’s actually a complex behavioral health challenge, too. The game changer: a combination of diet support & behavioral health coaching is proven to be some of the fastest, least invasive and most effective interventions to GI symptom relief.
Let’s take a deeper look at this approach, and the factors that influence its adoption:
Mind-boggling diets are easy to abandon
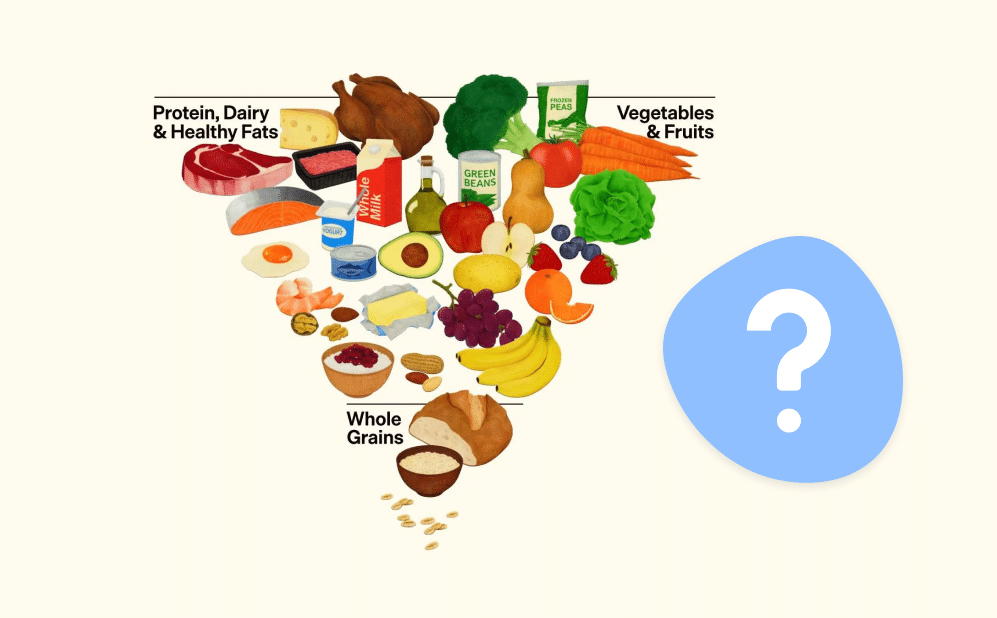
Most people with IBS symptoms know the complexity of the diet called low FODMAP. FODMAPs are specific types of poorly digested carbohydrates found in multitudes of foods, including dairy, grains, fruits, vegetables, legumes and sweeteners. People with IBS are hypersensitive to these foods, causing gas, bloating, stomach cramps, diarrhea, and constipation.
Implementing a low FODMAP diet is incredibly intensive and detailed, and involves 3 phases: elimination of foods high in FODMAPs types and sub-groups of food; reintroduction of one FODMAP subgroup at a time; and then personalization, a highly customized balance of tolerated foods and symptom control.
The level of complexity and detail in implementing a low FODMAP diet is staggering, and its failure rate for people going it alone — assuming they’re even doing it correctly — is, unfortunately, quite high.
Instinctively, there seems to be no rhyme or reason to what a FODMAP food is or isn’t. Here’s just a small example of why it can be so confusing:
• Melons? Generally ok, but absolutely not watermelon.
• Nuts? Go for it, just not pistachios or cashews.
• Bananas? Only if they’re greenish, and not a whole one!
• Cream cheese, no – camembert cheese, yes!
• Wheat bread? Nope, but certain sourdough bread is a-ok.
In addition to the lists of high- and low-FODMAP foods to remember, low FODMAP diets are unlikely to work if people eliminate some FODMAPS but not others; or if people don’t allow the requisite 2-6 weeks of the elimination phase. Still others complicate their results if they try to reintroduce too many foods at once.
And, it’s not one size fits all—specific FODMAPS that may be huge offenders for one person, may be perfectly fine for another person and in fact shouldn’t be eliminated, because they are critical to supporting that person’s healthy gut bacteria.
Even the most motivated and diligent people attempting to do a low FODMAP diet on their own find it time-consuming, overwhelming, and confusing, and often abandon it.
However, with instruction, hands-on support, meticulous monitoring, frequent check-ins, behavioral coaching and custom tweaking, low FODMAP diets often bring rapid and game-changing symptom relief to people suffering with GI symptoms.
Wishing for diet and nutrition help
It may surprise you to learn that despite struggling with unmanaged GI symptoms for years, most people have never worked with a dietitian. Yet a recent survey of IBS patients in the U.S. showed that more than 60% of this population wished they had been informed by their provider about the impact of food, mental health and lifestyle in relation to their illness.
GI-specialized dietitians are an underutilized, highly knowledgeable resource, but people just aren’t getting to them. They may instead seek help from general dietitians, who have broad – but not deep – knowledge of GI conditions. For others, education and care coordination from their GI doctors may be lacking; insurance may not cover this benefit, or they simply may not know how to find a qualified dietitian.
Even GI experts often lack the highly specific knowledge to help their patients: 40% of GI doctors and 16% of GI nurses feel they do not have good knowledge of IBD nutrition.
How Oshi Health sets you up for success
Working with an Oshi registered dietitian isn’t just following a meal plan. Our RDs use evidence-based nutrition care tailored to your specific needs, including:
- A well-balanced, nutritionally optimized care plan
- Supplement recommendations, if needed, to ensure you meet all your nutritional needs
- Elimination diet guidance when necessary to identify food triggers
- Diet education specific to your GI condition with access to a library of resources
“Low-hanging fruit” controls symptoms fast
Sometimes, a GI-trained dietitian determines that low FODMAP is not necessarily the first step. They may instead tailor an expert combination of very simple dietary interventions that can quickly reduce or eliminate their specific GI symptoms.
Many people are surprised to learn that these “lighter touches” can make an enormous impact with rapid symptom relief. They can have pleasant and unexpected “aha” moments – for example, garlic is a big GI offender, but with an expert and nuanced diet/nutrition intervention, people might learn that garlic oil or other garlic seasonings are still perfectly ok.
Some of a dietitian’s other interventions may include:
• Implementing “low FODMAP lite,” modified to eliminate the most commonly consumed high FODMAP foods, identified through journaling or an assessment with the dietitian
• Adjusting amounts of fiber (soluble, insoluble)
• Addressing GERD triggers (spicy foods, chocolate, citrus)
• Reducing GI stimulants like salt, fat, sugar, caffeine, alcohol
• Modifying the texture of diet (soft, “GI gentle”)
GI-trained registered dietitians also balance their recommendations with other behavioral, preference-based, whole person considerations and helpful tools that can help adherence to programs:
• The person’s own dietary philosophy, likes/dislikes, lifestyle and other medical conditions
• Other health aspects: hydration status, nutrient deficiencies (e.g. not enough protein)
• Supplement expertise (fiber, enzyme, vitamin, mineral)
• Suggestions on tweaking size, frequency and timing of meals, additional focus on chewing
• Simplify implementation of programs with meal ideas, recipes, shopping lists
Dietary triggers evade and evolve, requiring lifelong management
Another complicating and potentially discouraging aspect of GI diets is that people’s triggers don’t always stay the same. They can and do change over the years, even once they’re initially well-managed and stabilized. Lifelong intervention is required to monitor symptoms and triggers, tweak diet and behavior to keep symptoms under control. Ongoing observation, identification of patterns, modifications to diet are possible with consistent support and access to coaching to guide decision-making.
Behavior and diet for sustained relief
Getting GI-specific diet and nutrition expertise and support in treating GI symptoms is game-changing. This combination of support, training, monitoring, and behavior coaching makes dietary changes effective and satisfying – even life-changing – for people.
Because they achieve symptom relief, people feel empowered, hopeful and confident. Because it’s customized to their preferences, the program is sustainable, with a high likelihood of long-term compliance. The longer people stay on the prescribed diet/nutrition program, the better skilled they are at understanding potential relapse trigger points – and not being derailed and discouraged by them. The result is an enduring, holistic lifestyle and behavioral change.
Oshi is your partner in digestive health
Feel like your digestive concerns are running your life? You’re not alone—and we’re here to help you find lasting relief.
Oshi Health GI providers, gut-brain specialists, and registered dietitians work together to address your symptoms and find solutions that actually work for you.
Whether you’re dealing with chronic digestive issues or unpredictable symptom flare-ups, our GI specialists deliver:
✔ Personalized care plans tailored to your lifestyle
✔ Science-backed strategies to calm your gut
✔ Compassionate, whole-person care
✔ And so much more!
Ready to take control of your gut health?