People suffering with GI illnesses often aren’t getting the answers or support they need. The current care model—bouncing between primary care to gastroenterologist to procedure—leaves huge gaps in diagnosis and treatment, neglects adjacent specialty treatments like nutrition and mental health, waits until symptoms escalate to react, and eventually causes patients to give up on seeking care. This transactional approach to care leaves people suffering in silence and does little to prevent costly escalations in care.
What people really need falls into the gaps between primary and procedurally-driven GI care: comprehensive, physician-led, behavioral and dietary interventions that have been rigorously studied and proven to reduce symptoms and cost in patients with digestive diseases. Academic referral centers have already moved toward this model, yet the vast majority of patients are unable to access an integrated team of physicians, dieticians, psychologists, and health coaches who are all focused on their GI condition.
People need integrated care — especially for GI conditions. Coordinated, specialized treatments that address all triggers and causes of their GI condition from one central care plan: evidenced-based dietary interventions, GI-focused behavioral therapies, health coaching with daily support, all supervised by a board-certified gastroenterology team.
Why has this care model remained elusive until now, while people suffer in silence?
Integrated care: highly effective and yet so hard to find
Integrated GI care only exists in a few academic medical centers scattered across the U.S. To benefit from this care model, patients need geographic access (or plan to travel), the appropriate health insurance coverage or financial means, and the ability to take significant time away from work.
At these integrated GI care centers, patients get access to a full team of deeply knowledgeable GI specialists, including physicians, nurses and NPs, registered dietitians and psychologists with specific experience in treating GI-related mental health issues. Treatments, diagnostics, labs, and specialists are located on the same campus. This enables patients to complete numerous healthcare tasks in one trip and accelerates diagnostic workup and time to symptom resolution.
Integrated care is patient-focused; the entire team collaborates on a unified treatment plan. Unlike traditional GI care, which is punctuated by wait times and delays, integrated care combines evidenced-based diagnostics and treatments together. Labs and testing are done as the patient meets with highly-trained specialists to tackle other contributing factors. There is clinician support to help implement and promote compliance with prescribed therapies. Perhaps most importantly, treatment programs are not “one size fits all,” but specifically tailored to the patient’s very specific triggers, needs, and preferences.
As you might expect, numerous studies have proven that this model of care improves outcomes, reduces costs, and results in better patient experience. This model works. But it doesn’t scale with brick-and-mortar academic centers.
Procedures are well-funded. Prevention is not.
In traditional GI care, patients are usually steered towards costly and expensive procedures like colonoscopy and endoscopy due to high reimbursement and a lack of incentives for alternative approaches. Procedures increase patient risk and time away from work, and rarely diagnose the prevalent etiologies for the most common gastrointestinal complaints. Instead, they rule out more serious problems like cancer or rare inflammatory conditions and leave patients without a definitive diagnosis. Notably absent from traditional GI care is patient access to evidenced-based dietary, behavioral, and medical care for the most common GI complaints, the ability to get an actual diagnosis, or identify the root cause of symptoms.
For many with GI symptoms, this cycle can repeat itself for years, with no accurate diagnosis or treatment plan. Many patients, desperate to “do something” to alleviate years of unmanaged symptoms, may actually escalate to surgical intervention — like gallbladder removal — as a last measure that is often not medically necessary.
Today, complex but effective conservative interventions like diet, behavioral, and remote monitoring are rarely utilized. They require investment by clinics in additional staff and a higher touch care model. There is no incentive to build out and scale this model, because despite proven effectiveness, the current fee-for-service ecosystem does not incentivize this approach.
Referred to the wrong specialists
Part of the challenge of multi-disciplinary care is that both primary care physicians and gastroenterologists do not have access to expert providers to refer patients for evidenced-based dietary and behavioral GI therapies.
Dietitians without GI training typically do not have deep knowledge of the dietary interventions needed to improve symptoms in this complex patient population. Similarly, generalist mental health practitioners see a variety of conditions including anxiety and PTSD, but lack the speciality training to manage patients with disorders of the gut-brain axis. Behavioral therapies have been shown to be more effective than medications in many patients with IBS.
Without the right kind of GI-specialized behavioral and dietetics help, patients don’t get symptom relief. Worse, they can feel patronized, pigeonholed or invalidated by their doctors. After making the effort and spending time and money to pursue deeper treatment, people are often left wondering if it’s “all in their head” — a very discouraging place.
Underutilized: Nutritional and psychosocial interventions
The role of diet and mental health interventions and their relevance to GI treatment is often overlooked. These disciplines have strong evidence in numerous clinical trials, but due to access and reimbursement issues, are unavailable to the vast majority of patients.
People may leave a GI appointment with a one-page handout on an extremely complex, multi-step diet, and complicated diets are often abandoned because they’re too difficult to understand and implement alone. With the proper support and guidance, dietary change can provide rapid and long-term symptom relief. Better yet, dietitians can often identify more conservative approaches to try and find less complex diets to improve patient compliance.
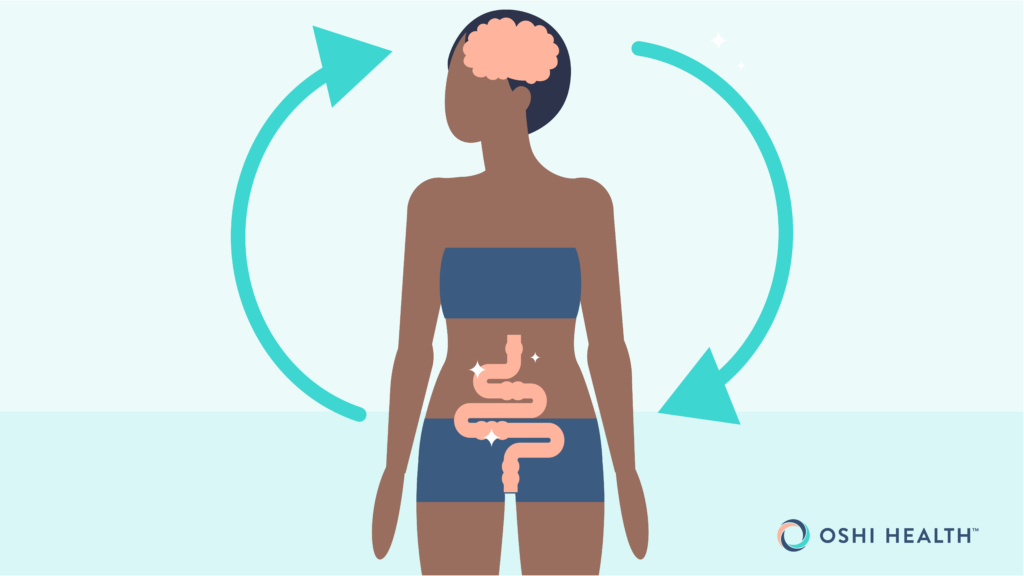
The “gut-brain” connection is a known medical paradigm, with an entire subspecialty of gastroenterology focused on these patients. There are more neurons in the gut than in the brain, and the vagal nerve literally connects the brain to the gut and influences digestive function. GI-focused behavioral therapies include cognitive behavioral therapy, gut-directed hypnotherapy, and other techniques that target these gut neurons to create long-lasting and durable symptom resolution.
People must cobble together their own GI care teams
Traditional GI care puts the burden on the person suffering with GI symptoms to be their own patient advocate, referral coordinator, and care manager. They must research and verify the credentials of the gastroenterologist, dietitian, and psychologist. They typically bounce between their PCPs and GI doctors trying to manage flare ups, and frequently end up in the ER. They spend hours on online message boards trying to understand the complicated universe of treatments, tests, and possible diagnoses or to commiserate with others that are also struggling to find and access care that works.
As they cobble together their own care teams, they encounter significant wait times, time away from work for appointments, specialists only marginally qualified to treat GI issues, various patient portal communication and payment systems, and endless billing, insurance and coverage hassles.
With no centralized care coordinator, communication between providers is non-existent and the onus is on the patient to convey critical lab results, procedures, medications or treatment information. There is no feedback loop and frequently, even conflicting medical advice.
In this staggered care sequence, frustrated patients often give up on GI care. They end up in the ER because they lack access to evidenced-based integrated GI care — although they are diligently trying to see specialists. This is the failure point and a significant cost center of traditional GI care.
Integrated GI care in action
Here’s what integrated care looks like: Jen, a 37 year old who has been suffering with undiagnosed GI symptoms for 4 years has developed a fear of eating, because she believes food is the direct cause of painful or unpredictable GI symptoms. She presents to an integrated GI team with frequent GI distress cramps, bloating, and diarrhea.
Traditional GI care would have started her with an upper endoscopy, which would usually be normal, to rule out a blockage, and would have sent her home with a one-page handout on a “low FODMAP” diet, a very complicated and overwhelming dietary protocol, and maybe the phone number for a dietitian, who may or may not take insurance. She would still be without a confirmed diagnosis or actual treatment plan, and with a near 100% chance of her symptoms continuing.
In an integrated care model, after a detailed intake with a GI provider, Jen meets frequently with her dietitian who helps her identify and eliminate the foods that aggravate her symptoms – providing some relief within a few weeks. Labs will be done to rule out malnutrition or identify inflammation. A specialized GI health coach is on hand every day to help Jen to implement a complex diet and answer her questions.
A GI psychologist educates Jen about the gut-brain axis, addresses her compulsive fears with action-based cognitive behavioral therapy, and uses mindfulness to help her learn to calm the triggers of a symptom flare-up, and avoid unnecessary and expensive utilization when symptoms acutely escalate. With regular psychologist visits and at-home practice of these techniques, Jen learns she can control most of her symptoms on her own, and gets even more symptom relief within 4 sessions. If her symptoms do flare, she can quickly get in touch with her care team to get help, potentially avoiding a trip to the ER.
Jen achieved symptom control without ever needing a colonoscopy or ending up in the ER with a flare.
Make integrated care accessible to all
The case for challenging the status quo and democratizing integrated care is clear. It closes coverage gaps and focuses on the root of the problem, not just treating symptoms. Because it starts with broader, more conservative interventions, its approach is lower cost than invasive, “diagnosis of exclusion” approaches that require procedures like endoscopy and colonoscopy. It provides fast symptom relief, prevents flare-up escalation and provides durable solutions.
Most importantly, it significantly improves quality of life and outcomes for people living with GI conditions.
Oshi is your partner in digestive health
Feel like your digestive concerns are running your life? You’re not alone—and we’re here to help you find lasting relief.
Oshi Health GI providers, gut-brain specialists, and registered dietitians work together to address the root cause of your symptoms and find solutions that actually work for you.
Whether you’re dealing with chronic digestive issues or unpredictable symptom flare-ups, our GI specialists deliver:
✔ Personalized care plans tailored to your lifestyle
✔ Science-backed strategies to calm your gut
✔ Compassionate, whole-person care
✔ And so much more!
Ready to take control of your gut health?