Irritable bowel syndrome (IBS) is a condition that involves abdominal discomfort with changes in bowel movements or habits. Although not the only contributor, miscommunication between the gut and the brain can trigger IBS flares, leading to constipation, diarrhea, or a mix of these issues. Neuromodulators are medications that alter the way the nervous system and gut interact and may address issues you’re experiencing with motility, pain, or both.
If you have irritable bowel syndrome (IBS), you experience abdominal discomfort as well as changes in your bowel movements or habits. The condition is the most diagnosed gastrointestinal (GI) disease, affecting 10 to 15 percent of people. I belong to this club.
If you’re like me and have this often-frustrating condition, you may have wondered about medications for IBS, including whether neuromodulators may be able to help. The short answer is that while medications might indeed help you, they aren’t a magic-bullet solution. Nor are they the only treatment or management technique you’ll need.
“Neuromodulators can be quite beneficial for IBS symptom management,” says Steven Feinstein, PhD, a clinical health psychologist and gut-brain specialist at Oshi Health. “But they don’t solve the many contributing factors that cause IBS. It’s the integration of care, only possible on a multidisciplinary team, that can address the medical, behavioral, and nutritional factors that lead to truly life-changing and lasting progress.”
In this article, we’ll explain what neuromodulators are, how they can help with IBS, other IBS medications and treatments, and why a multidisciplinary approach is key to feeling better.
Understanding IBS and its symptoms
IBS is a functional disorder, which means it occurs because your GI tract is having difficulty performing its functions. A functional GI disorder differs from a structural disorder, in which a clinician can detect abnormalities in the digestive tract, such as polyps, tumors, ulcers, and more. In a diagnosis of IBS, no structural abnormalities are causing your symptoms.
Your symptoms may vary, depending on your IBS subtype.
IBS subtypes
- IBS-C: IBS with constipation
- IBS-D: IBS with diarrhea
- IBS-M: IBS with mixed bowel patterns
Common IBS symptoms
- Abdominal pain
- Bloating
- Changes in how often you pass stool
- Changes in stool form or appearance
- Constipation
- Diarrhea
- Distension
- Feeling like you’ve had an incomplete bowel movement
- Feeling unwell
- Gas
- Mucus in the stool
- Pain with bowel movements
- Straining with bowel movements
- Urgency
- Vacillating between constipation and diarrhea
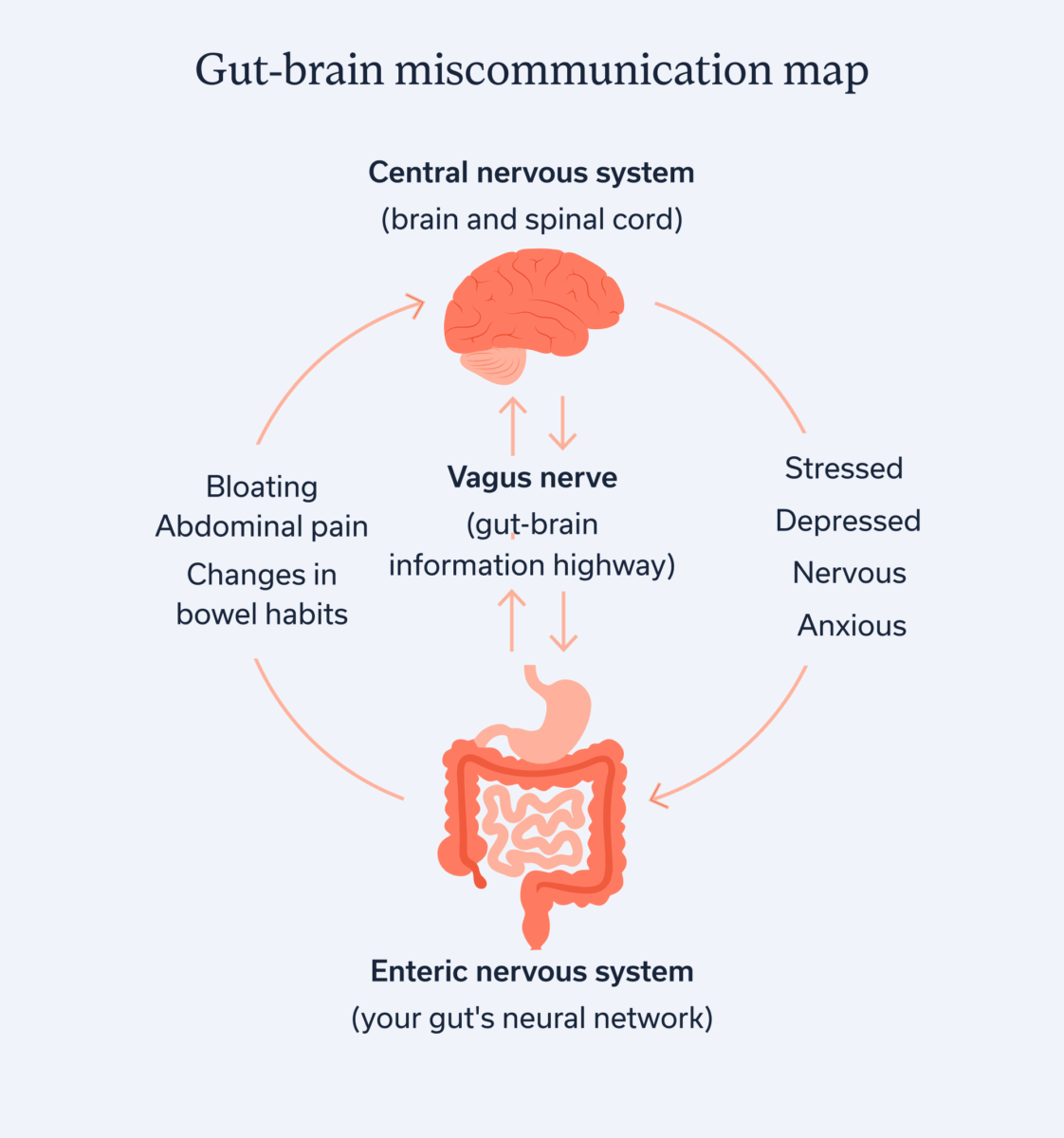
IBS typically involves some miscommunication along the gut-brain axis. “IBS is more than a gut issue,” Dr Feinstein says. “It’s a communication issue between the gut and brain. The nervous system in our gut communicates directly with our brain to coordinate the amazing and complicated digestive process. Many factors (e.g., stress, trauma, microbiome), can disrupt this gut-brain communication. And when it gets disrupted, we get more dysregulated. This, in turn, can intensify GI symptoms common in IBS such as pain, bloating and changes in bowel habits.”
Yes, the brain is involved in IBS, but it’s clear that those of us who have the condition aren’t imagining our symptoms. Our gut and brain are miscommunicating, and understanding a bit more about the nervous system can help us all better understand IBS.
Your GI tract has an extensive neuronal network called your enteric nervous system (ENS), which controls your digestive functions. The ENS is a branch of your autonomic nervous system (ANS), which controls the involuntary responses in your body (think heart rate, temperature regulation, and more.) You may be more familiar with other divisions of the ANS, which include your parasympathetic nervous system (PNS), also called “rest and digest,” and the sympathetic nervous system (SNS), also called “fight or flight.” The PNS is your “calm” response, whereas the SNS is your “stress” response.
When you’re stressed, depressed, nervous, anxious—you name it—your stress response can disrupt your PNS and ENS, causing a communication snafu. Further complicating matters is that these miscommunications can create a vicious cycle, where GI symptoms can cause increased psychological distress that then leads to even more frustrating GI symptoms.
Treatment overview: Why medication is only one piece
Having IBS myself, I’ve used my journalism skills to conduct a ton of research on the condition over the years. I’ve learned through studies and from working with my own gut-brain clinical support team that your best bet to manage the condition is to come at it from several different angles. These angles include making lifestyle changes, focusing on mental health, and sometimes leaning on medications and supplements if needed.
I take a few healthcare provider-approved supplements and one medication to treat IBS. They help, but ultimately, managing the conditions requires a multidisciplinary approach. For example, for me, I know that getting oodles of exercise, avoiding trigger foods, managing stress and anxiety, engaging in cognitive behavioral therapy (CBT), and doing my best to manage the pelvic pain I have from endometriosis all help keep my symptoms in check—most of the time.
Your treatment approach will likely differ from mine, and that’s why working with a knowledgeable care team that creates an individualized approach for you is important.
Neuromodulators for IBS: A first-line approach
Based on your unique cluster of symptoms and other factors, your provider may suggest a medication. Neuromodulators are one class of medications that you might encounter as someone living with IBS.
What are neuromodulators and how do they work?
“Neuromodulators are medications that change the way the nervous system processes pain and motility signals between the brain and the gut,” Dr. Feinstein says.
Neuromodulators have different mechanisms of action, depending on the medication. This class of medications includes antidepressants, antipsychotics, anticonvulsants, and more.
I get it. When a healthcare provider suggests you go on an antidepressant or antipsychotic, you may feel like they aren’t taking your physical symptoms seriously and are chalking your experience up to mental health issues. But that’s not the case. Where appropriate, providers may recommend these medications to improve gut-brain interaction, rectify motility disturbances, and reduce visceral hypersensitivity.
- Motility disturbances. Motility is the movement of food and waste through the digestive tract, which may be impaired in people with IBS, often from gut-brain miscommunication.
- Visceral hypersensitivity. Visceral hypersensitivity is when you experience pain when your organs are performing their usual functions, again generally from disrupted gut-brain communication.
“Since IBS is now understood as a disorder of this brain-gut interaction,” Dr. Feinstein says, “these medications can impact our experience of GI symptoms. For example, people with IBS often have increased nerve sensitivity in the gut which intensifies the experience of symptoms, such as gas and bloating, to more painful and even life-disrupting levels.”
Types of neuromodulators used for IBS
Tricyclic and tetracyclic antidepressants (TCAs)
Tricyclic antidepressants include amitriptyline, nortriptyline, imipramine, desipramine, and more. They are a go-to treatment for people experiencing visceral hypersensitivity with IBS. These meds tamp down pain by inhibiting the reuptake of the neurotransmitters serotonin and norepinephrine. Inhibiting reuptake means you will have higher levels of these neurotransmitters in your brain.
Tetracyclic antidepressants include mirtazapine, mianserin, and trazodone. They are a potential treatment for people experiencing early feelings of fullness (satiety) when eating, nausea and vomiting, and sleep disturbances. Although slightly different, they work in some ways that are similar to tricyclic antidepressants. Some tetracyclic antidepressants increase the release of norepinephrine, while others inhibit serotonin and norepinephrine reuptake.
Selective serotonin reuptake inhibitors (SSRIs)
Selective serotonin reuptake inhibitors (SSRIs), another type of antidepressant, include paroxetine, fluoxetine, sertraline, citalopram, escitalopram, and more. They can help with anxiety, depression, and phobias, all of which can contribute to IBS symptoms. SSRIs, as their name suggests, work by inhibiting the reuptake of serotonin, elevating your brain’s levels of the feel-good hormone.
Serotonin norepinephrine reuptake inhibitors (SNRIs)
Serotonin norepinephrine reuptake inhibitors (SNRIs), yet another type of antidepressant, include duloxetine, venlafaxine, desvenlafaxine, milnacipran, and more. They help with IBS-related pain. SNRIs work by blocking the reuptake of both serotonin and norepinephrine, boosting levels of these neurotransmitters to help relieve visceral hypersensitivity, often characteristic of IBS.
Delta-ligand agents
Delta-ligand agents include gabapentin and pregabalin. These two specific medications are anticonvulsants that also help with nerve pain. In fact, pregabalin gained its original Food and Drug Administration (FDA) approval for the treatment of neuropathic pain. Providers sometimes prescribe both these medications to treat fibromyalgia, for example. Many people with fibromyalgia also have IBS, and these medications can help treat related visceral hypersensitivity that many people with these conditions experience.
Atypical antipsychotics
Atypical antipsychotics include sulpiride, levosulpiride, quetiapine, aripiprazole, and olanzapine. These medications block dopamine receptors, but they have additional mechanisms of action. Blocking dopamine receptors may help with pain by causing a reduction in pain perception. Although research is still emerging for their use in people with IBS, atypical antipsychotics may be helpful for reducing visceral hypersensitivity.
Azapirones
Azapirones are a type of anti-anxiety medication and include buspirone and tandospirone. By interacting with your serotonin receptors, they can help reduce anxiety, which can itself be an IBS trigger. They may also help with motility concerns, but we need more research on these medications for the treatment of IBS.
What to expect from neuromodulators
Which neuromodulator may be right for you will depend on your specific symptoms, the other treatments you’ve tried so far and their results, your underlying conditions, and more.
Neuromodulators may take time to work, so you may need to track your symptoms over the course of a few weeks.
“Most patients notice improvement in GI symptom discomfort after three to four weeks of consistent neuromodulator use,” Dr. Feinstein says. “Those patients with co-occurring anxiety or sleep difficulties often experience improvements in these symptoms even within a couple of weeks of starting medication.”
Your provider will likely start you on a low dose first to assess whether you experience side effects, which vary by medication. If you’re tolerating the medication well, they may increase your dose if needed.
Expert GI care for the whole you
Our licensed GI specialists are here to listen and help you find lasting relief
Other medications used in IBS treatment
Neuromodulators aren’t the only medications on the block for treating IBS. Again, your care team will assess which medications are right for you based on individual factors.
For IBS with diarrhea (IBS-D)
- Rifaximin, a gut-directed antibiotic, helps address imbalances to your gut microbiome, the community of bacteria that live in your digestive tract.
- Eluxadoline slows down an overactive bowel.
- Loperamide, sold under the brand name Imodium, is an over-the-counter medication intended for the short-term use of easing diarrhea.
- Bile acid binders (e.g., cholestyramine) bind to bile acids in your gut and reduce the amount that enters your colon, helping to reduce diarrhea.
For IBS with constipation (IBS-C)
- Lubiprostone softens the stool to ease bowel movements.
- Linaclotide increases fluid secretion in your intestines to help facilitate bowel movements.
- Plecanatide increases intestinal fluid secretion and intestinal motility, and it softens stool.
- Osmotic laxatives (e.g., polyethylene glycol) increase water in the stool to soften it and aid bowel movements.
For abdominal pain and bloating
Your provider may also recommend enteric-coated peppermint capsules. Peppermint oil may help reduce pain and other symptoms associated with IBS, and the coating prevents the medication from dissolving in your stomach before it reaches your intestines.
Key takeaways
- IBS is a condition that involves miscommunication between your gut and your brain.
- This miscommunication can lead to discomfort associated with constipation, diarrhea, or a mix of these issues.
- Neuromodulators alter the way the nervous system and gut interact; they may address issues with motility, pain, or both.
- Everyone who has IBS experiences the condition a bit differently; a knowledgeable care team (check out Oshi Health’s approach) can help you decide if an IBS medication is right for you and which one may be appropriate.
FAQ
-
Neuromodulators alter the way your nervous system and gut interact. They may address common IBS symptoms related to motility dysfunction or visceral hypersensitivity, an increase in pain of your internal organs.
-
Neuromodulator medications include antidepressants, antipsychotics, anticonvulsants, and anti-anxiety medications.
-
Everyone with IBS experiences the condition a bit differently, so the best medication for you will depend on your symptoms, your underlying conditions, other treatments you’ve tried, and more. A knowledgeable care team can assess you to determine which medication, if any, is right for you.
-
If you are experiencing an IBS flare, you may wish to consult your care team for a customized approach to managing your flare. The best ways to calm a flare will depend on your unique symptoms and other factors. However, avoiding trigger foods and eating easy-to-digest foods that are gentle on your GI system can help. Focusing on stress management and your mental health can also help the gut and brain communicate better and may lessen or resolve your flare symptoms.
-
IBS triggers vary from person to person. However, one of the most common triggers is stress, which can disrupt communication along your gut-brain axis.
-
IBS does not have a cure or a one-stop-shop pill. However, some medications, such as those that affect motility and alter pain signals, can help ease your symptoms, along with lifestyle and diet changes.
Find lasting relief from IBS symptoms
Feel like irritable bowel syndrome (IBS) is getting in the way of enjoying your life? You’re not alone—and we’re here to help.
Oshi Health GI providers, gut-brain specialists, and registered dietitians work together to address symptoms like indigestion, bloating, and stomach pain, and find solutions that actually work for you.
Our GI specialists will work with you to reduce symptom flare-ups through:
✔ Personalized care plans tailored to your lifestyle
✔ Evidence-based IBS nutrition guidance
✔ Science-backed strategies to calm your gut
✔ Compassionate, whole-person care
✔ And so much more!
Ready to take control of your IBS symptoms?