Feeling pain in your pelvis? Straining during bowel movements? Noticing thin, stringy stool? All of these symptoms might point to a common but treatable condition: a hypertonic pelvic floor. Here’s everything you need to know about the relationship between your pelvic floor and bowel movements.
Your pelvic floor muscles are serious contenders for a V.I.M (very important muscle) award. They support the organs in your pelvic region, including your bladder, bowels, and reproductive organs. If they’re chronically tight, a condition called a hypertonic pelvic floor, they can cause some uncomfortable symptoms: difficulty passing a bowel movement, pain during sex, and even blood in your stool.
The good news? “Pelvic floor dysfunction is highly treatable” says Savannah Hood, PT, DPT, a pelvic floor therapist at Inspire Health, “Most people see major improvements with proper care.”
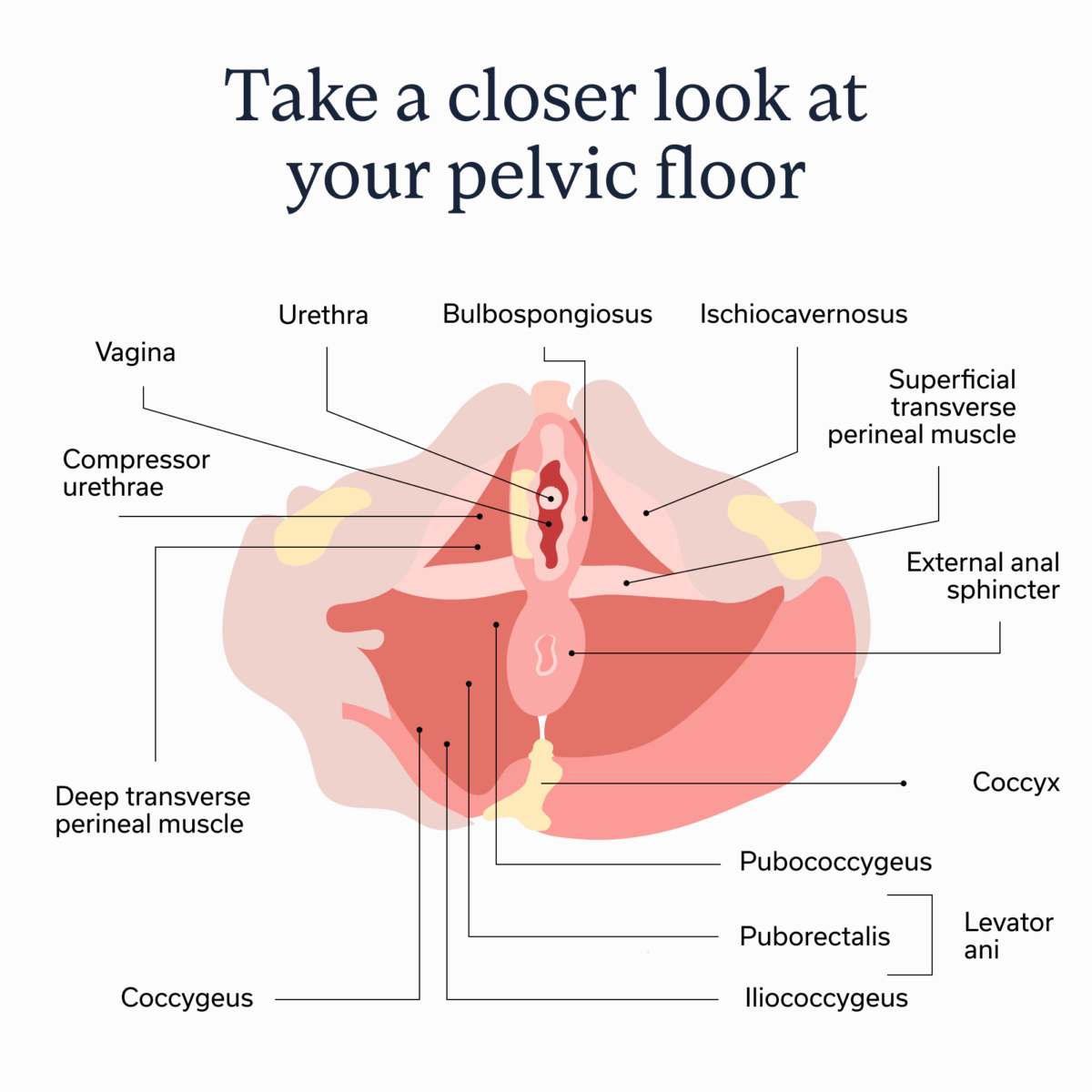
Pelvic floor 101
Have you ever crossed a swinging bridge? Before getting on it, the swaying motion and planks of wood may make it seem like the bridge can’t hold you, but once you get on, you realize it’s much more supportive than it looks.
Above the floor of the pelvis, there’s a group of muscles that work similarly to that bridge: The pelvic floor muscles can move dynamically when we breathe, cough, or during labor, but are designed to keep the pelvic region strong and steady. Together with nearby tissues, they hold the pelvic organs in place. These organs include the bladder, urethra, anus, uterus, cervix, and vagina. If you locate these muscles and organs on an anatomical map, you’ll notice they are all between the lower abdomen and upper thighs.
But that’s not the only function these muscles serve. “Pelvic floor dysfunction can greatly affect bowel movements,” says pelvic floor physical therapist Jessie Klein, PT, DPT, “The alignment of the pelvic floor can affect the angle of which the rectum sits and can most easily complete bowel movements.” She notes that alongside the bowels, these muscles also support sexual functioning and the bladder. Yet we don’t often notice their supporting role unless something is off.
The pelvic muscles can commonly suffer from one or more of these three problems:
- Hypertonic: When they are overactive and tight
- Hypotonic: When they are underactive and weak
- Dyssynergic: When the muscles don’t work well together
When your pelvic floor muscles are too weak, tight, or not operating properly, it can lead to a range of issues including urinary incontinence (loss of bladder control), fecal incontinence (difficulty with or inability to control bowel movements), and/or pain in the pelvic region.
Weak and tight pelvic floor symptoms
Whether your pelvic floor is hypertonic, hypotonic, or dyssynergic, there are overlapping symptoms you may experience. Common symptoms include:
- An urgent or frequent need to urinate
- Constipation, the feeling of needing to poop but not being able to
- Difficulty controlling gas
- Difficulty urinating or emptying your bladder fully
- Leaking urine, especially when laughing, coughing, or exercising
- Leaking stool
- Full or heavy sensation in the vagina (for those assigned female at birth)
- Pulling or aching feeling in the vagina (for those assigned female at birth)
- Pain during sex
More serious symptoms that may require prompt care are:
- Frequent urinary tract disorders
- Pain when urinating
- Full or heavy sensation in the vagina with seeing a bulge coming out of the vagina (for those assigned female at birth)
Seek immediate medical attention if you cannot urinate or have lost complete control of your bowels or bladder.
How pelvic floor dysfunction affects bowel movements
We’ve established that the pelvic floor can impact bowel movements, but why exactly does this connection exist? Like the common real estate mantra, it comes down to location, location, location.
“The alignment of the pelvic floor can affect the angle of which the rectum sits and how easy it is to complete bowel movements,” explains Dr. Klein, “If the pelvic floor muscles are hypertonic or too tense, it can prevent stool coming out completely.”
She adds that a hypertonic pelvic floor may manifest as incomplete bowel movements or stool that looks like thin ribbons. Anal fissures, a tear in the rectum that can cause painful bowel movements and bloody stool, as well as hemorrhoids, swollen veins around the anus, may also appear if your pelvic floor is hypertonic.
However, many of these symptoms could be due to other conditions too, such as chronic constipation or irritable bowel syndrome (IBS). Weakened support from connective tissues (not just pelvic floor muscles) can also cause hemorrhoids, while Crohn’s disease may lead to anal fissures.
Even things like a low-fiber diet or sitting on the toilet for too long can cause some or all of these symptoms, which is why it’s important to see a healthcare provider to determine whether your pelvic floor is actually responsible for the pain or other symptoms you may be experiencing.
Self-check: clues from your routine
If there are multiple conditions and habits that can cause bowel symptoms associated with pelvic floor dysfunction, how can you tell if the pelvic floor muscles or something else is causing your symptoms? A clinical assessment and diagnosis (which we’ll dive into in the next section) is the only surefire way.
While waiting for your appointment or before making one, there is a self-check you can do at home to assess pelvic floor strength:
- In the vagina: If you have a vagina, insert a clean finger inside your vagina and tighten the muscles around it, which is the same squeezing movement you might make while trying to hold in pee. If the pelvic floor is working properly, the muscles should tighten, then easily release.
- In the rectum: Place a clean finger inside the rectum and tighten the muscles. They should tighten and then be able to release if the pelvic floor is working properly.
Diagnosis: How clinicians figure out what’s going on
While an at-home check provides useful clues, it doesn’t replace a diagnosis from a qualified clinician. “Getting a skilled assessment is the gold standard,” says Dr. Klein, “It’s difficult to know whether you have a problem with your pelvic floor muscles without a proper assessment.”
When assessing the pelvic floor, a healthcare provider will ask about your symptoms, physically examine your pelvis, and review your medical history. They will also typically order additional tests, especially if your bladder or bowel function have been impacted.
The use of the term “healthcare provider” here can mean a few things. When the pelvic floor impacts bowel movements, there are a few subspecialties of clinicians who can diagnose your symptoms, mainly gastrointestinal (GI) providers and physical therapists with additional training in the pelvic floor. Odds are, you’ll probably work with both during your treatment.
Pelvic floor dysfunction treatment
While pelvic floor dysfunction can be treated, the exact care plan varies depending on whether problems stem from weak, tight, or uncoordinated muscles. No matter which type, treatment options fall into a few key camps: developing a better bowel routine, pelvic floor physical therapy, lifestyle and behavioral changes, and dietary adjustments.
Pelvic floor physical therapy (PFPT)
Once you have your diagnosis, you’ll most likely start pelvic floor physical therapy (PFPT), which focuses on helping the muscles hit a goldilocks level of tension (aka not too tight or too weak). Dr. Klein says that in PFPT, “you will learn many techniques, exercises, and self-care strategies to help with your pelvic floor and bowel dysfunction.”
Many of these techniques will be done during physical therapy appointments, though your provider will probably give you homework, which may include breathing techniques as well as exercises that target the pelvic muscles.
Foundational bowel regimen
If your pelvic floor is negatively impacting your bowel movements, it’s time to take a look at your number-two routine. If it’s difficult to complete a bowel movement, bowel retraining may be helpful—if your healthcare provider advises it. With this approach, you use something called “digital stimulation” to hopefully rev up some action. Don’t let the word “digital” scare you—there’s no technology involved. Instead, you:
- Lubricate a finger, insert it into the anus, and move it around to relax the muscles.
- After stimulation, sit on the toilet with as much privacy as possible.
- Repeat the first two steps if you don’t have a bowel movement in 20 minutes.
Along with digital stimulation, another component of bowel retraining is setting a specific time for a daily bowel movement, ideally 20 to 40 minutes after a meal. Turns out a regular routine keeps you regular.
Dr. Hood also says that a squatty potty or small footstool can help with pelvic alignment when going to the bathroom. She explains, “Elevating your feet changes the angle of your pelvis, which helps the pelvic floor relax and makes bowel movements easier and more complete.”
Lifestyle strategies
Many GI providers and physical therapists recommend lifestyle changes to better support pelvic floor muscles. These can include:
- Low-impact workouts: When the pelvic floor isn’t working as intended, high-impact workouts, like CrossFit or running, may put extra strain on the region. Low-impact workouts, like barre and Pilates, strengthen the body without extra strain, says Dr. Hood.
- Pain management: Warm baths, topical therapies for fissures or hemorrhoids, and other provider-recommended treatments may help with any pain.
- Stretching: Gentle stretching and exercises throughout the day can help ease tension on the pelvis.
Nutrition
At first glance, nutrition is the dark horse of this list. It doesn’t have a clear connection to pelvic floor muscles. But as most guidance on healthy living will tell you: Nutrition and movement go hand-in-hand. And that means bowel movements and movements by the pelvic floor muscles.
While researchers are still unsure why nutrition impacts the development of pelvic floor disorders, there is ample evidence to show the connection exists, meaning a balanced diet reduces the risk of developing these disorders and may help treatment.
Since “eat healthy” is super vague advice, here are some more specific guidelines to follow:
- Eat a well-balanced plate: “Adding more fruits, vegetables, whole grains, and oats can make a big difference, especially when paired with enough plain water throughout the day,” advises Dr. Hood. Plus, a well-balanced diet lowers the risk of obesity or being overweight, which are risk factors for pelvic floor disorders.
- Enjoy highly processed foods in moderation: One study found women who ate an ultra-processed diet (think: foods with many, many ingredients on the label like cakes and potato chips) had a higher rate of pelvic floor disorders. While it’s ok to occasionally splurge, cut back on highly processed foods when possible.
- Get adequate fiber: “Most people don’t meet the recommended 25–30 grams of fiber per day,” says Dr. Hood, “Low fiber can contribute to constipation, diarrhea, and increase risk for other health issues.”
- Hydrate: Hydration supports proper bowel function, though some liquids, like alcohol or coffee, can actually contribute to dehydration, meaning it may be safer to stick to water and herbal teas if experiencing bowel symptoms.
Pelvic floor exercises (what helps vs. what to avoid)
When we think of pelvic floor workouts, kegels, an exercise where you tighten, hold, and then release pelvic floor muscles, are probably the first to come to mind. However, you shouldn’t do this exercise unless it’s recommended by a provider. “Doing too many kegels actually worsens some symptoms,” Dr. Hood explains, “so kegels alone aren’t always the best solution.”
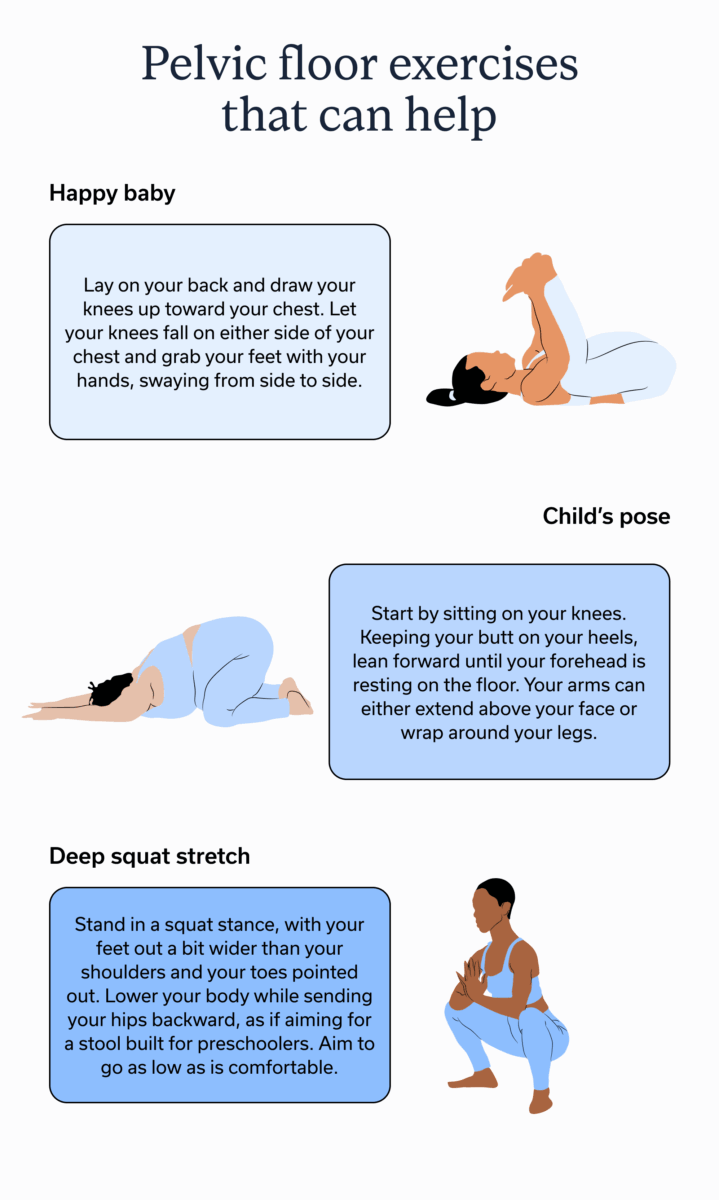
What exercises can help? Dr. Klein often advises people try exercises that relax pelvic floor, such as:
- Happy baby: Lay on your back and draw your knees up toward your chest. Let your knees fall on either side of your chest and grab your feet with your hands, swaying from side to side.
- Child’s pose: Start by sitting on your knees. Keeping your butt on your heels, lean forward until your forehead is resting on the floor. Your arms can either extend above your face or wrap around your legs.
- Deep squat stretch: Stand in a squat stance, with your feet out a bit wider than your shoulders and your toes pointed out. Lower your body while sending your hips backward, as if aiming for a stool built for preschoolers. Aim to go as low as is comfortable.
A physical therapist with training in PFPT can recommend additional exercises, striking a balance between ones that strengthen and lengthen the pelvic muscles.
Breathing exercises may also help, particularly diaphragmatic breathing, which is a slow, mindful style of breathing. When the diaphragm, the main muscle for breathing, moves, the pelvis does too. “As you inhale, your abdomen and pelvic floor should expand and relax,” says Dr. Klein. The relaxation is particularly helpful for a hypertonic pelvic floor.
When to seek care (Red flags and next steps)
Knowing when to seek care for symptoms isn’t easy. But there are a few red flags to look out for: You should visit a GI provider about bowel-related symptoms that may be associated with pelvic floor issues if you experience:
- Leaking urine or stool: “Leaking is a clear sign the pelvic floor needs attention,” says Dr. Hood.
- Chronic constipation: When constipation lasts for weeks, it’s another nudge to make an appointment.
- Rectal bleeding: If there is blood in stool movements, make an appointment with a GI provider.
- Pelvic pain: “With sex or otherwise, pain is not normal and should be addressed,” says Dr. Hood.
Once the diagnosing provider has a clear idea what’s going on, they’ll likely compile a multidisciplinary team to help with treatment. For pelvic floor issues, the team roster often includes a GI provider, pelvic floor PT, and possibly a GI registered dietitian or gut-brain specialist.
Prevention and long-term maintenance
Certain risk factors for pelvic floor disorders, like having a hysterectomy, having a vaginal childbirth, or weakened muscles due to genetics, are out of our control.
That said, there are some ways to prevent pelvic floor disorders or maintain progress after treatment ends:
- Maintain a healthy weight: Being overweight or obese can cause extra strain on the pelvic floor. By maintaining a healthy weight with a balanced diet and regular physical movement, you can help prevent problems with the pelvic floor.
- Manage gastrointestinal conditions: Having a GI disease associated with chronic constipation, diarrhea, or other irregular bowel symptoms increases the strain on the pelvic floor. By managing these conditions, you reduce the risk of pelvic floor disorders.
- During pregnancy: If pregnant, consider prepartum or postpartum pelvic floor training with a qualified physical therapist. This can reduce the risk of pelvic floor complications during or after pregnancy.
Key takeaways
- Pelvic floor disorders, including hypertonic pelvic floor dysfunction, can disrupt bowel movements, as these disorders mean the pelvic floor muscles aren’t controlling the anus and rectum as they should.
- Common bowel-related symptoms of pelvic floor disorders include leaking stool, blood in stool, difficulty pooping, thin stool, hemorrhoids, and anal fissures.
- Fixing a pelvic floor problem often involves lifestyle and nutrition changes, as well as medical guidance. A GI provider, such as those at Oshi Health, can play a role in determining if bowel-related symptoms are due to an issue with the pelvic floor or another condition. Oshi can also help you find a pelvic floor therapist to provide additional support and treatment.
Frequently asked questions (FAQs)
-
Fixing a hypertonic pelvic floor is often a combination of attending pelvic floor physical therapy sessions, doing exercises and stretches that relax the pelvic floor muscles, and engaging in breathing exercises that further loosen these muscles. If bowel movements are affected by a tight pelvic floor, bowel retraining and following nutrition advice, such as eating more fiber, may help as well.
-
A tight pelvic floor can affect bowel movements. It most typically leads to constipation or difficulty passing bowel movements since when pelvic floor muscles are tight, they aren’t able to relax properly to allow stool to leave the body.
-
While there is an hypertonic pelvic floor and IBS, there is no evidence that a tight pelvic floor causes IBS. It’s more likely that constipation from IBS affects the pelvic floor muscles, increasing the likelihood of pelvic floor disorders.
Oshi is your partner in digestive health
Feel like your digestive concerns are running your life? You’re not alone—and we’re here to help you find lasting relief.
Oshi Health GI providers, gut-brain specialists, and registered dietitians work together to address your symptoms and find solutions that actually work for you.
Whether you’re dealing with chronic digestive issues or unpredictable symptom flare-ups, our GI specialists deliver:
✔ Personalized care plans tailored to your lifestyle
✔ Science-backed strategies to calm your gut
✔ Compassionate, whole-person care
✔ And so much more!
Ready to take control of your gut health?