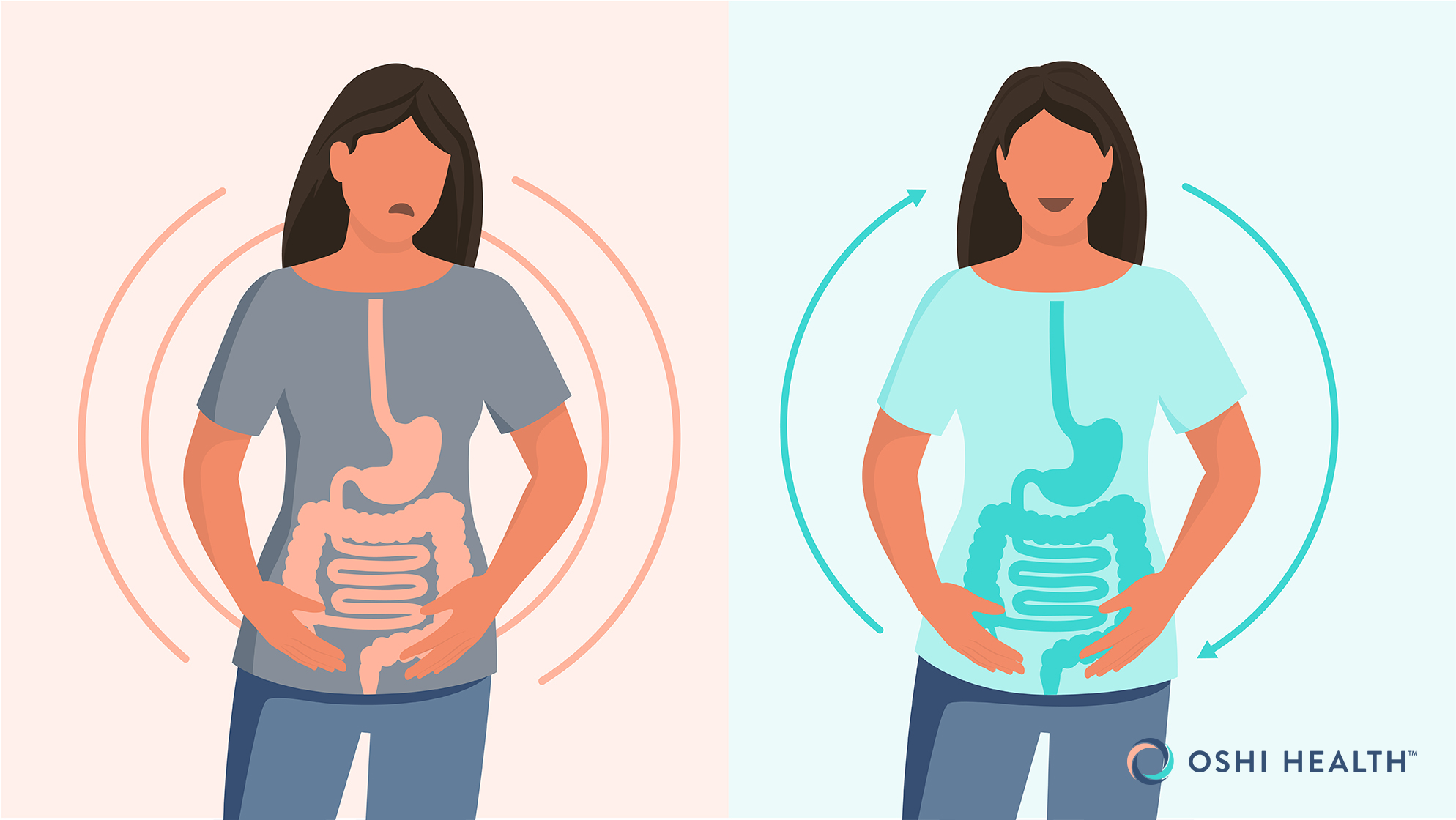
Your gut and brain are in constant communication, meaning stress and anxiety can trigger digestive issues—and vice versa. In this article, you’ll learn more about how this gut-brain connection works and explore strategies to break the cycle for better mental and gut health.
Anxiety and stomach issues go hand in hand. As a frequent public speaker, I’ve found that I can’t eat in the hours before I give a presentation, but afterward, I’m ravenous. And when I get bad news or am terribly stressed or sad, I’ve been known to lose my lunch.
In stressful or anxious moments, suddenly experiencing an upset stomach, with symptoms such as nausea, cramps, bloating, diarrhea, or even vomiting, is common. We often chalk up these sudden symptoms as “having butterflies in the stomach,”“having a nervous stomach,” or even “feeling your stomach drop.” I personally like saying that I have a case of the collywobbles.
But stomach issues can also be chronic or long-lasting. When someone experiences chronic anxiety, the gastrointestinal (GI) tract can react constantly as well. Chronic GI issues can also wreak havoc on your mental health.
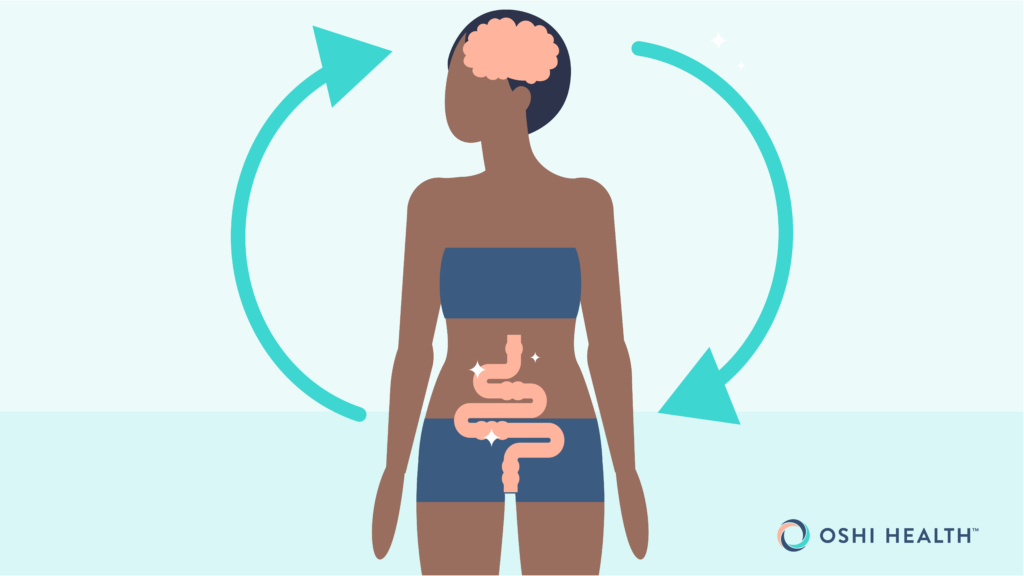
The brain and gut are connected by what’s called the gut-brain axis. Researchers even refer to the GI tract as “the second brain.” In this article, you’ll learn all about the gut-brain connection, how anxiety can affect the stomach, how this relationship has links to conditions such as irritable bowel syndrome (IBS), and what you can do to treat symptoms and move forward.
Understanding anxiety-related stomach issues
“I like to think about the connection between the gut and the brain like a two-way street connecting our minds and bellies,” says Mariah Corneille, PsyD, Lead Gut-Brain Specialist at Oshi Health. “It’s the conversation between our emotions and our digestion, where stress can stir the pot, or throw things off, and a happy gut can maintain harmony within the body.”
For a deeper understanding of the gut-brain connection and why anxiety can drive stomach issues, we need to dive into a brief explanation of the autonomic nervous system (ANS). The ANS controls all the involuntary processes in our body, from heart rate and breathing to sexual arousal and digestion.
“By understanding this relationship,” Dr. Corneille says, “we can better manage how stress affects our gut health and how gut health can affect our mental state.”
Understanding the autonomic nervous system and anxiety
The ANS has three divisions. You’re probably most familiar with the sympathetic nervous system (SNS), also called “fight or flight,” or your stress response. Classic signs you’re in fight-or-flight mode include experiencing an adrenaline rush, an elevated heart rate and blood pressure, and a higher body temperature. I was recently in a minor fender-bender and felt my ANS wake up hardcore.
We have another branch clinically known as the parasympathetic nervous system (PNS), also called “rest and digest.” You’re in rest-and-digest mode when you feel calm and relaxed.
The third branch is the enteric nervous system (ENS). The ENS is an extensive network of millions of neurons along the walls of your GI tract. It controls digestive functions, such as gastric secretions, motility (the movement of food and waste), and more. It works independently and in conjunction with the SNS and PNS.
“The enteric nervous system,” Dr. Corneille says, “governs the function of the gastrointestinal system and operates independently but in close coordination with the parasympathetic nervous system, which is responsible for rest and digestion.”
Understanding the gut-brain axis
The gut-brain axis involves communication processes from your central nervous system (CNS), which is your brain and spinal cord, and all three branches of your ANS.
The reason your GI tract may act up in an acute stress moment, such as when you must give a presentation, is because your fight-or-flight switch gets flipped on. When this happens, your body is essentially going into survival mode. In doing so, it turns off the switch on your rest-and digest mode and affects how the enteric nervous system operates.
“The enteric nervous system works hand-in-hand with the parasympathetic nervous system, kind of like a conductor leading an orchestra, to keep our bodies in harmony, especially during rest, where the body can exert all energy towards optimal gut functioning,” Dr. Corneille says.
“This interaction is vital for maintaining a balance, ensuring that our digestive processes run smoothly, particularly in moments of relaxation or when the body is healing,” she adds.
We can take my recent minor fender bender as an example. I got rear-ended, which flooded me with adrenaline in the moment. Essentially my body immediately allocated all resources toward my ability to survive by putting me in fight-or-flight mode.
My rest-and-digest mode went on pause, impacting my enteric nervous system’s ability to do what it was supposed to with my breakfast. My breakfast did not make a reappearance, but that’s because I sat on the shoulder of the road for few minutes, taking deep breaths to reactivate my rest-and-digest mode and get my enteric nervous system to return to tackling the mix of coffee and smoothie in my stomach.
By the way, the gut-brain connection also works in reverse. Having a disrupted gut microbiome can also lead to stress and get those butterflies or collywobbles really going regularly. That’s just one reason why GI health is so important.
Causes of anxiety-related stomach issues
Stress and anxiety can disrupt the enteric nervous system. “Normal function of the nervous system, tasked with keeping us alive, is to prioritize action and deprioritize brain-gut communication,” says Steve Feinstein, PhD, a gut-brain specialist at Oshi Health.
Fight-or-flight mode is great when we must react quickly to save ourselves or loved ones. Hundreds of years ago humans had to be ready to run from predators, for example. In more modern times though, we typically aren’t fleeing from tigers or grizzly bears, except maybe in our more adventurous dreams.
“Our nervous system at times can be quite out of step with our lives today,” Dr. Feinstein adds. “Threats today often come not in the form of an attack but [in the form of] more chronic psychosocial stressors.”
Today, we face chronic stress from relationship problems, politics and the news, community issues, money concerns, busy schedules, and work, school, and family responsibilities. Hello, to-do list!
“As a result,” Dr. Feinstein says, “these times of stress lead to decreased brain-gut communication and the increased dysregulation of the digestive process.”
We can also experience chronic stress from previous traumas. Chronic stress and past traumas are linked to anxiety and panic disorders. Chronic stress can lead to a state of hypervigilance, where you’re subconsciously always on edge in case of a threat. Hypervigilance plays a big role in post-traumatic stress disorder (PTSD), generalized anxiety disorder (GAD), and social anxiety disorder.
Ultimately, when we experience anxiety, whether in the moment or long-term, our stress response gets ratcheted up, which can cause GI issues via the gut-brain axis.
Symptoms of anxiety-related stomach issues
You might experience a wide range of GI symptoms resulting from anxiety or stress. And some GI conditions have connections to anxiety, including irritable bowel syndrome (IBS), gastroesophageal reflux disease (GERD), and inflammatory bowel disease (IBD).
IBS is categorized into three types:
- IBS with mostly constipation (IBS-C)
- IBS with mostly diarrhea (IBS-D)
- IBS with mixed bowel habits (IBS-M)
In a 2016 journal article published in Psychological Medicine, researchers conducted a meta-analysis of existing studies and found that people with anxiety had a more than two-fold risk of developing IBS.
GERD is a more serious and chronic form of acid reflux or heartburn. A 2024 study published in the journal Scientific Reports found an association between GERD and anxiety and depression.
Anxiety doesn’t cause IBD, which includes Crohn’s disease and ulcerative colitis, but it can exacerbate symptoms. Plus, those who have IBD are at a higher risk of developing anxiety and depression.
Anxiety-related stomach symptoms and conditions
- Abdominal pain
- Acid reflux or GERD
- Bloating
- Changes in appetite (a loss or increase)
- Constipation
- Diarrhea
- Gas
- IBS-C
- IBS-D
- Indigestion
- Nausea
- Vomiting
- Worsened IBD symptoms
Diagnosing and treating anxiety-related stomach issues
Your Oshi provider will work with you on using your gut-brain axis to help calm your mind and your stomach. If needed, your provider may also run some tests to help rule out or diagnose any underlying conditions that could be the culprit of your GI distress.
If you do have a condition that affects the GI tract, focusing on the gut-brain connection can greatly complement other methods of care, including medications or altering diet. For example, IBS treatment works best when it encompasses both physical and mental health care.
Effective solutions for reducing stomach pain
The solutions that are best for you will depend on your specific underlying condition or symptoms. However, several methods can help you calm your mind and therefore your stomach, via the gut-brain connection.
“Our interventions target nervous system control to minimize this disconnect and the impact on the gut,” Dr. Feinstein adds.
These solutions all help you switch off or control your fight-or-flight response, which then helps you tap into your rest-and digest response. When you’re in rest-and-digest mode, your enteric nervous system (the neurons in your GI tract) gets the chance to work more effectively. The following are all natural remedies for anxiety relief that may help ease your GI symptoms.
Belly breathing
Belly breathing is a technique you can use in the moment to help keep your mind and stomach calm. It’s a great tool if you suddenly experience nausea, pain, bloating, or other symptoms in the face of a stressor.
“It’s like hitting the reset button on your nervous system—sending a message between your gut and brain that it’s safe to relax,” Dr. Corneille explains. “This simple, yet powerful, technique can quickly soothe both the mind and the digestive system, making it a go-to tool in anxiety-provoking situations.”
Mindfulness meditation
Mindfulness-meditation techniques have been shown to help with various anxiety-related stomach issues, including IBS. You can learn mindfulness meditation by working with a therapist or using an app that offers a guided practice.
According to the American Psychological Association, a mindfulness-meditation practice might include focusing on the present without judgment, engaging in breathwork, and even performing gentle movements.
GI-focused cognitive behavioral therapy
Cognitive behavioral therapy (CBT) is a form of therapy that has proven effective in the face of anxiety, according to the American Psychological Association. A gut-brain specialist, such as those at Oshi, can help you use CBT to improve your gut-brain connection.
Three principles of CBT
- Examining and changing unhelpful ways of thinking
- Examining and changing unhelpful behavior patterns
- Learning better ways of coping with anxiety and stress
The International Foundation for Gastrointestinal Disorders says, “CBT helps control thoughts and changes a person’s reaction from ‘fight or flight’ to ‘rest and digest.’” The organization goes on to explain how with IBS, someone might engage in “catastrophizing” or “assuming the worst.”
Here are some examples. With catastrophizing, someone might think, My IBS is ruining my life. With assuming the worst, usually about a future event, someone might think, I will be stuck in the bathroom for my whole vacation. CBT can help you retrain such thoughts and focus instead on proactive approaches for managing situations that might crop up with IBS.
Gut-directed hypnotherapy
Gut-directed hypnotherapy involves having a gut-brain specialist help you to imagine a different experience of sensations, emotions, and more while in a hypnotic state.
The Crohn’s & Colitis Foundation is an advocate for managing anxiety with hypnotherapy for IBD. And research over the past decade has shown that hypnotherapy may improve IBS GI symptoms up to 73 percent.
Managing stress and anxiety for long-term relief
Anxiety and stress are intricately connected. Reducing stress may help reduce anxiety, and vice versa, and therefore calm your stomach symptoms. The best stress- and anxiety-reduction techniques for you will depend on your unique symptoms and circumstances.
Identify your stress triggers
One of the first steps is identifying your stressors and anxiety triggers. Dr. Corneille says this involves being a detective and looking for bodily clues—and then taking a proactive approach.
“Keeping a journal of symptoms, diet, and stress fluctuations can help highlight patterns and pinpoint what might be causing flare-ups,” she says. “It’s about noticing the patterns—what foods, thoughts, or situations set off your digestive alarms—and then taking steps to manage them before they spiral.”
Practice stress-reducing techniques
We all face times of heightened stress every now and then. This could be because of a big work or school project or deadline, facing an illness or that of a loved one, and more. We can take steps in the moment, such as belly breathing to help us remain calm. However, chronic stress is something we need to work on lessening long-term. Here are some helpful habits.
Sustainable habits for stress reduction
- Engage in regular downtime. Taking time for yourself is self-care. Build mini bouts of downtime into your everyday schedule. And plan for longer stretches, such as a vacation or staycation, every so often for recharging.
- Prioritize your sleep quality and quantity. Research shows that good sleep helps you become more resilient to stress, meaning you’re better able to cope with it when it arises.
- Engage in regular exercise. Exercise can boost your mood. It also helps your body adapt to physical stressors, which can help you become more resilient to mental stressors in everyday life. As an added benefit, exercise may improve the gut microbiome, which may also help ease GI issues.
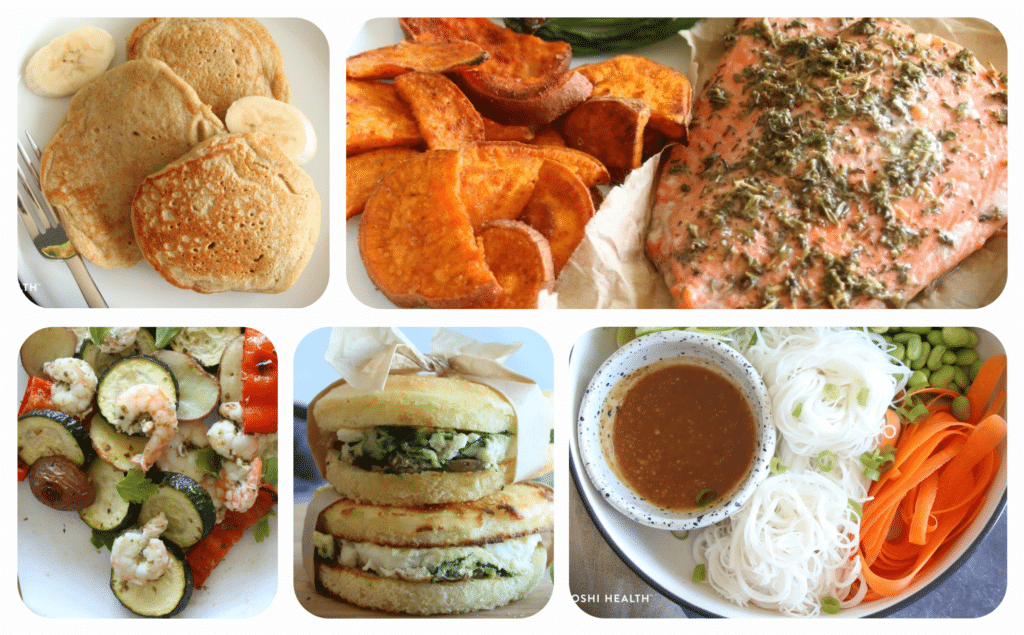
Dietary changes for a healthy digestive system
In addition to working on the gut-brain connection, changing your diet may help alleviate stomach symptoms and even reduce stress. The specific diet you need to follow will depend on any allergies or sensitivities you may have, and any underlying conditions.
For example, people with IBD may need to avoid certain foods. And people who have IBS and some other conditions may need to follow a low FODMAP diet. A low FODMAP diet helps reduce intake of fermentable oligosaccharides, disaccharides, monosaccharides, and polyols, hence the acronym.
In general, people can increase gut health with the following food strategies:
- Reduce sugar. Sugar contributes to inflammation and disrupts the gut microbiome and intestinal barrier, leading to GI and other symptoms. High sugar consumption and anxiety are also linked.
- Reduce ultra-processed foods. Ultra-processed foods are often high in added sugar, preservatives, and other additives. These ingredients can also disrupt the gut microbiome and barrier and cause inflammation. Some preliminary research shows a connection between ultra-processed foods and mental health issues.
- Increase fruits and vegetables. Fruits and vegetables, which are high in anti-inflammatory compounds, help improve the gut microbiome and strengthen and maintain the gut barrier. However, if you require a low FODMAP diet, you may need to avoid some fruits and vegetables. Your Oshi provider can help customize a diet that’s right for you.
- Decrease omeg-6s and increase omega-3s. When we have a higher ratio of omega-6 fatty acids to omega-3 fatty acids, as is common in the Western diet, inflammation can increase. Omega-6s are common in processed seed oils, such as canola, soybean, sunflower, and corn. Instead, cook with olive or avocado oil, which are rich in omega-3s. Boosting omega-3 intake may lessen anxiety.
When to seek medical attention for stomach issues
Most people experience occasional GI discomfort, such as bloating. And our bowel habits can temporarily change from factors like travel, diet, and illness.
But if you have unexplained stomach issues that don’t resolve in a few days, you should consult your doctor to uncover the root cause. A GI behavioral health provider can help you determine if anxiety is causing some of your issues. Track your symptoms in a journal until your appointment and note if anything worsens or alleviates symptoms.
Seek urgent medical care for the following symptoms:
- Sudden and severe stomach pain that impacts your daily functioning
- GI issues that are accompanied by a high fever
- Blood in your stool or vomit
- Black or tarry stool for several days
- A hard abdomen
- Vomiting that doesn’t resolve
- The inability to have a bowel movement or pass gas
- GI issues that cause you to feel dizzy or to faint
- GI issues accompanied by heart palpitations or shortness of breath
Whole-person GI care—now available from almost anywhere
Oshi Health is where medical, dietary, and gut-brain treatments come together under one virtual roof, all provided by leading GI specialists. With virtual visits available within 72 hours—including evenings and weekends—we make it easy to see a GI provider within days.
Frequently asked questions (FAQ)
-
Yes, anxiety can cause GI issues, such as pain, bloating, nausea, vomiting, constipation, diarrhea, and more.
-
You can get rid of anxiety that is affecting your GI tract by taking deep and slow breaths, reducing stress, and more. However, if you frequently experience GI issues because of anxiety, talk to your doctor. You may have an underlying GI condition or may be experiencing chronic anxiety. Treatments can help.
-
Keep a journal that tracks your mood, stress level, and GI issues. If you notice an uptick in stomach pain or symptoms when you are anxious or stressed, you are likely experiencing stomach issues that are triggered by changes in your mental health.
-
Supplements that might help your upset stomach may be different than those that help someone else. That’s because symptoms vary. Talk to your doctor or provider who can recommend the right supplements for your unique stomach concerns related to anxiety.
Takeaway
It makes sense: How we feel mentally can impact how our stomach feels. Anxiety and stomach issues are intricately connected via the gut-brain axis, and the GI tract is actually considered our second brain. Doing your best, with the help of evidence-based practices, to keep stress and anxiety in check can also help keep stomach issues in check.
GI-focused mental health care can be difficult to find. But the gut brain-specialists at Oshi Health can help you find solutions for calming anxiety that’s impacting your stomach. Oshi’s program implements seamlessly with your existing GI care if you already work with a doctor. Click here to get started.
Oshi can help you heal your gut-brain connection
When anxiety hits, your stomach often feels it first. If your digestive issues flare up with stress or worry, you’re not imagining it.
Whether you’re facing daily discomfort or unpredictable flare-ups, Oshi gut-brain specialists can help you:
✔ Understand how stress and emotions impact your gut
✔ Find personalized solutions that fit your lifestyle
✔ Calm your digestive system with science-backed strategies
✔ And so much more!
Ready to feel better from the inside out?