Have you ever felt a painful burning in your chest after eating a big meal or drinking something acidic, like lemonade? If so, you may have experienced acid reflux. When this sensation comes back time and time again, a clinician will often categorize it as gastroesophageal reflux disease, or GERD for short.
GERD and acid reflux impact about 20 percent of the U.S. population, and while they are uncomfortable, you don’t have to live through them without support. There are effective treatments and lifestyle modifications that can help.
Ahead, we go into more detail about how to best manage symptoms, what acid reflux and GERD are, and common signs to look out for. We’ll also discuss how to work with a GI provider to create a customized treatment plan.
What are acid reflux and gastroesophageal reflux disease (GERD)?
Imagine you’re swimming in a river with a strong current. Going downstream is easy, while swimming upstream takes a lot of effort and may lead to exhaustion and fatigue. Food and other secretions in the GI tract work similarly—they move easily down the GI tract as part of the digestive process. But sometimes, the contents of the stomach swim upstream instead.
“Acid reflux occurs when the contents of the stomach, including stomach acid, back up into the upper parts of the GI tract, including the esophagus and sometimes the throat, resulting in uncomfortable symptoms,” explains Kaitlin Voicechovski, MS, RDN, LDN, Lead Registered Dietitian at Oshi Health.
When this swimming upstream process happens chronically, it’s often gastroesophageal reflux disease (GERD). When it comes to GERD, two or more episodes a week is considered chronic.
While GERD includes frequent bouts of acid reflux, these episodes can manifest differently. “Everyone with GERD experiences acid reflux, however symptoms can present differently from person to person,” explains Voicechovski, “Some people feel a burning sensation, others may complain of regurgitation, and some experience symptoms more akin to chest pain without burning.”
Acid reflux symptoms and GERD
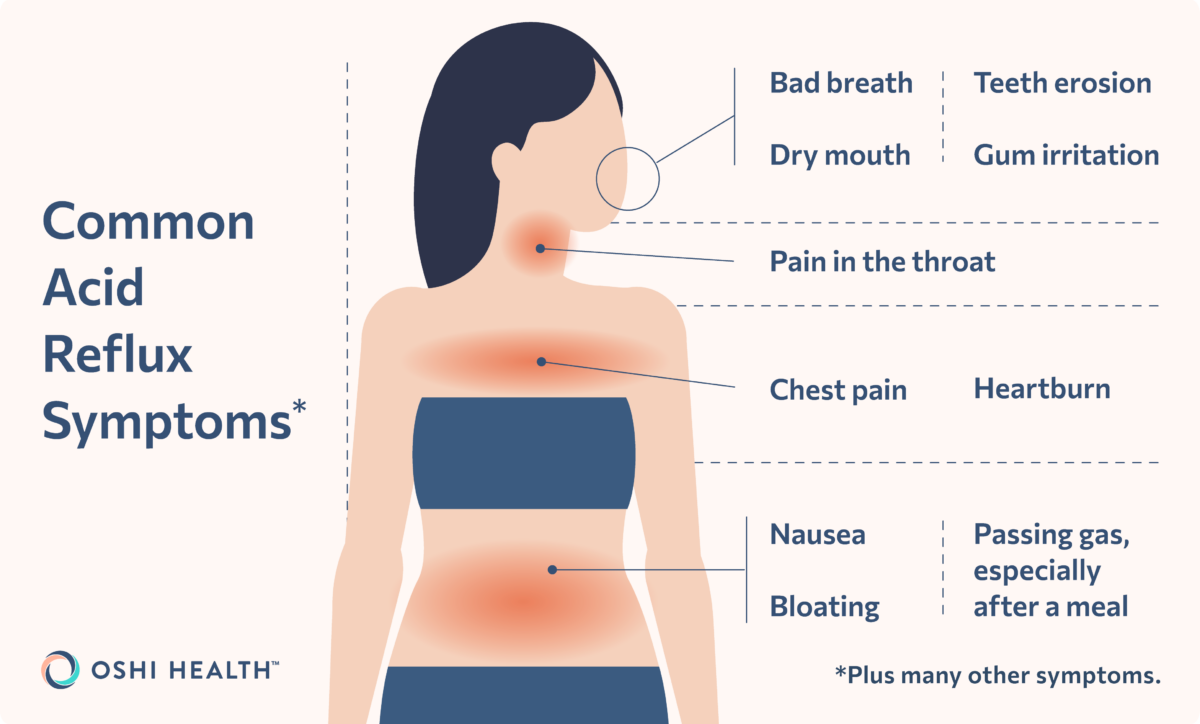
The most common and distinct sign of acid reflux (and therefore, of GERD) is that burning sensation in the chest, a.k.a. heartburn. Sometimes, you can experience heartburn behind the breastbone or in the space between your breastbone and throat. The other defining symptom is regurgitation, when the contents of the stomach come back up the GI tract. Often, this manifests as a sour or bad taste in the mouth.
Other symptoms of GERD include:
- Bad breath
- Bloating
- Burping or passing gas, especially after meals
- Chest pain
- Dry mouth
- Gum irritation or bleeding
- Nausea
- Pain in the throat
- Teeth erosion
As mentioned, acid reflux and GERD tend to present similarly, but GERD is chronic: With GERD, symptoms happen twice or more per week for weeks or months at a time. Sometimes, GERD can lead to more serious symptoms too, such as a loss of appetite, vomiting, problems swallowing, and bleeding in the digestive tract.
What causes GERD and acid reflux?
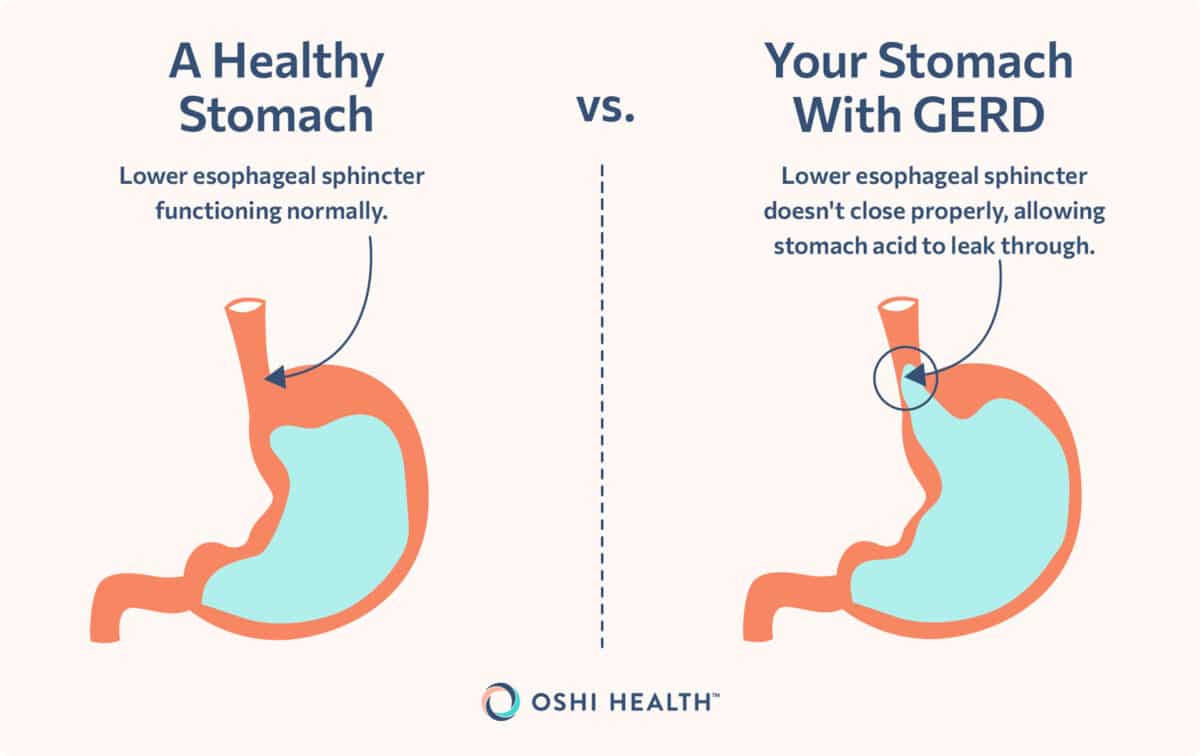
To understand why acid reflux and GERD occur, we have to take it back to anatomy 101, specifically the GI tract. The GI tract spans from the oral cavity in our mouth to the anal canal. It includes the esophagus, a tube that connects the throat to the stomach, and the stomach. Between the esophagus and the stomach is the lower esophageal sphincter (LES). Voicechovski explains that the LES separates these two parts, managing what travels between them.
If the LES inappropriately relaxes, acid reflux (and GERD, when chronic) can occur. When this happens, the stomach’s contents, including stomach acid, move into the upper parts of the GI tract, causing the symptoms we discussed in the previous section.
There are many reasons why the LES may relax, from one-time triggers to structural problems in the LES. Some of the most common causes include:
- Bariatric surgery: Bariatric surgery, which is often used to treat obesity, may also be a risk factor for GERD.
- Eating habits: Both eating habits and what you eat can cause acid reflux, which we’ll dive into more below.
- Hiatal hernia: This condition occurs when the stomach pushes up the diaphragm hole and into the esophagus. It can be caused by multiple factors, including birth defects, an injury, or changes as we age, and often leads to a defective LES.
- Medications: Certain medications may cause and/or trigger GERD symptoms. These include some asthma medications, benzodiazepines (a class of sedatives), calcium channel blockers (which can treat high blood pressure), and nonsteroidal anti-inflammatory medications (NSAIDS).
- Pregnancy: About 25 percent of pregnant people experience acid reflux or GERD. Pregnancy creates a temporary increase in abdominal pressure, which can cause the stomach to push up on the esophagus. Pregnancy usually leads to temporary acid reflux or GERD, often in the first trimester.
- Smoking: Tobacco smoke can relax the LES, causing acid reflux. When someone smokes, they may also take in more air, which increases the pressure on the LES from the stomach.
- Weight: Being obese or overweight increases intra-abdominal pressure which then pushes the stomach upwards. This upward movement may lead to the LES relaxing and stomach acid and content flowing into the esophagus.
GERD complications
Stomach acid breaks down foods, and to do so, it has to be quite powerful. When that powerful acid is misplaced in the upper digestive tract (due to GERD), it can lead to complications.
The most common GERD complications occur in the esophagus. These include esophagitis, a damage to the esophagus from acid, and Barrett’s esophagus, when the tissue lining the esophagus changes. The latter puts someone at greater risk for cancer. Someone with GERD can also develop an esophageal stricture, a condition where chronic inflammation in the esophagus creates a narrowing, which makes it hard to swallow and eat.
But that stomach acid doesn’t always stay in the esophagus. Sometimes it travels to the throat or even into the lungs. The former can cause laryngopharyngeal reflux, resulting in disturbances in the throat and vocal cords. The latter may cause asthma or asthma-like symptoms, such as trouble breathing or coughing.
Diagnosis and testing
If you think you have GERD, the next step is to book a doctor’s appointment—not to DIY your treatment plan. Dietitian Christine Byrne, MPH, RD explains that “so many people try to self-diagnose GERD and acid reflux, which usually leads to more health anxiety, bad treatments, and money wasted.” Instead, she recommends making an appointment with a gastroenterologist or another GI provider.
Your GI provider may be able to give you a diagnosis based on your symptoms and medical history alone. In some cases, they might run additional tests such as 24-Hour esophageal pH monitoring, an upper endoscopy (EGD), and/or esophageal manometry. Other common diagnostic tools include an esophagram, an X-ray of the upper digestive system, and a transnasal esophagoscopy. Along with diagnosing GERD, a GI provider can offer valuable insight into what is causing your symptoms.
Y.W., a patient of Oshi Health, reflects on their experience being diagnosed by a GI provider, “The NP with whom I went over my history and condition was the first person who has the knowledge of the possible cause of my symptoms. I met with three other doctors [before] and none of them was able to confirm/validate what I suspected was causing my GERD. I am very excited with Oshi Health and plan on a follow-up meeting to explore possible treatment solutions.”
Experience GI care the way it should be
Oshi Health is where medical, dietary, and gut-brain treatments come together under one virtual roof, all provided by leading GI specialists. Our whole person approach is clinically proven to help patients find relief from the full spectrum of GI symptoms and conditions, including acid reflux and GERD.
Treatment options
Along with diagnosing GERD and any underlying causes, a GI provider will create a treatment plan. While a successful plan differs from person to person, there are some common elements many plans share, including prescription and over-the-counter medications, and dietary and lifestyle adjustments. In more severe cases, where lifestyle interventions and medications don’t work, your provider may recommend surgery or another procedure.
Prescription and nonprescription medications
“Certain medications can help reduce or eliminate GERD symptoms, so it’s important to seek out a gastroenterologist who can help you with treatment,” says Byrne. The first line of defense is often proton pump inhibitors (PPIs), a class of medication that slows stomach acid production. Omeprazole, the most common PPI, is often prescribed for four to eight weeks.
However despite their popularity, 20-40 percent of those diagnosed with GERD don’t respond to PPIs. When this is the case, a gastroenterologist may prescribe prokinetic medications (which speed up stomach unloading) or histamine H2 receptor antagonists (which inhibit someone’s H2 receptors and lower acid excretion).
If you’re wondering where antacids like Tums fall on this list, it’s lower than you might think. While eating a Tums when experiencing heartburn used to be go-to medical advice, antacids are now often reserved for patients with more mild cases. Antacids, and some drugs in the other medication classes, are often available over-the-counter—that doesn’t mean you should run out and buy a GERD medication right now. It’s best to discuss medication options with a GI provider before purchasing a medication for GERD or acid reflux.
Managing and preventing acid reflux and GERD
Like most health conditions, GERD and acid reflux aren’t managed through medication alone. Your lifestyle choices have a direct impact on symptoms and flare-ups. Potentially helpful lifestyle modifications encompass what’s on your plate, in your wardrobe, and in your exercise routine.
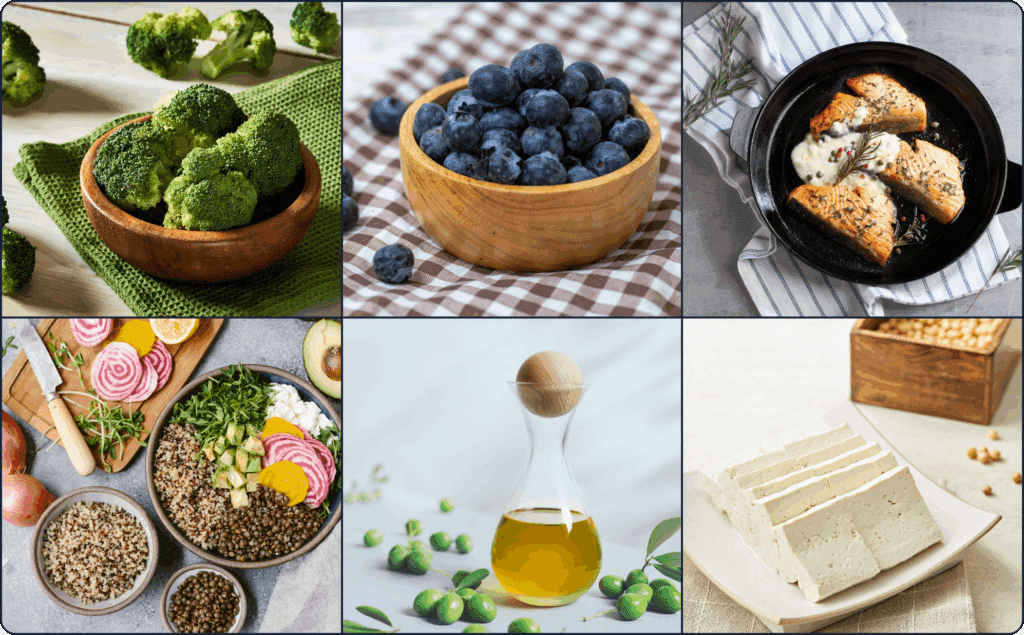
Avoid trigger foods
A key player in managing acid reflux is your diet. Both temporary acid reflux and GERD can be triggered by food. To ensure that your diet is working for, not against, you, it’s best to identify and avoid any trigger foods.
Voicechovski adds that while these triggers are unique to the individual, there are some common ones, such as:
- Alcohol
- Carbonated beverages
- Coffee (and caffeine in general)
- Chocolate
- Citrus or tomato products
- Fatty or fried foods
- Garlic
- Mint
- Onions
- Spicy foods
Working with a registered dietitian who has experience treating GI symptoms and conditions can be incredibly helpful in the process of uncovering potential trigger foods and providing dietary guidance that eases—rather than exacerbates—your symptoms.
Adjust eating habits
It’s not just what you eat that impacts acid reflux and GERD—how you eat influences symptoms too. Byrne recommends eating smaller, more frequent meals if suffering from acid reflux. With smaller portions, the stomach doesn’t produce as much stomach acid at once, reducing symptoms like heartburn. Emerging research also suggests eating slowly may prevent GERD symptoms.
Those with GERD and acid reflux may want to plan their last meal so it’s at least two hours before bedtime. When we lie down to sleep, our bodies can have a more difficult time digesting food, meaning more stomach acid could leak up into the esophagus.
Exercise regularly
Alongside a nutritious diet, another great strategy is to exercise regularly. A 2023 meta-analysis suggests those who meet the CDC’s physical activity guidelines had a lower risk of developing GERD. The CDC recommends two muscle-strengthening sessions, such as lifting weights or pilates, paired with 150 minutes of moderate cardio activity each week. Moderate activity could include walking, biking, or swimming. For more rigorous aerobic activity, the recommended weekly time is one hour and 15 minutes each week. And keep in mind these are all minimums, not maximums.
Before lacing on those sneakers, there are some additional guidelines for those diagnosed with GERD. For one, don’t exercise after eating. Exercising right after a meal can interfere with digestion. A 2022 study suggests that minimizing your time spent sitting may also be key to managing acid reflux, indicating that the frequency of exercise matters more than the intensity.
Stop or don’t start smoking
We’ve all heard that smoking is bad for our health. One way it impacts us: increasing the chance of developing GERD or worsening symptoms. Voicechovski recommends quitting smoking—or better yet, don’t start. She explains, “Nicotine is known to relax the LES, increasing the chances of reflux.”
The U.S. Department of Health and Human Services offers many resources for those looking to quit, including a quiz that will help you develop a personalized quitting plan. A healthcare professional may also be able to provide support and accountability throughout the quitting journey.
Avoid tight-fitting clothing
There isn’t a full-blown dress code those with GERD need to follow, but avoiding tight clothing may be a good idea. This is especially true if clothing is tight around the stomach, since that tightness can squeeze the stomach and relax the LES.
Surgery and other procedures
In severe cases where reflux does not respond to diet, lifestyle changes, and medication, surgery could be considered. The most common surgery is nissen fundoplication, a procedure that can fix a hiatal hernia. For this procedure, a surgeon wraps the stomach around the esophagus. (It’s worth noting that with fundoplication, a significant portion of patients need to go back on reflux medications after the surgery.)
A minimally invasive version of this surgery, transoral incisionless fundoplication (TIF), is also an option. Unlike nissen fundoplication, TIF doesn’t involve an incision, leading to faster recovery times with fewer complications. Another newer surgery is LINX device implantation. A LINX is a magnetic sphincter augmentation device that wraps around the LES and helps control what does and doesn’t get through it—and in which direction food moves.
Outlook and prognosis
GERD can be uncomfortable, but the good news is that most cases are highly treatable through a combination of dietary and lifestyle adjustments. For more severe GERD, surgery or another procedure may be required. Even after surgery, lifestyle modifications, such as the ones above, may help manage symptoms and prevent more serious complications.
Living with acid reflux and GERD
The above medications and lifestyle modifications can work wonders, but sometimes flare-ups still happen. If you experience acid reflux or other symptoms associated with GERD, you don’t have to grin and bear it. There are actionable steps to take during an acid reflux attack, plus questions to ask GI specialists to better manage your symptoms.
What to do during an acid reflux attack
If you experience an acid reflux attack, lifestyle modifications like changing your diet or quitting smoking may not help in the moment. Fortunately, there are smaller actions that can relieve symptoms ASAP. These include measures we’ve already discussed, such as switching to looser clothing.
Taking a sip of water to wash the stomach acid into the lower part of the GI tract may help as well. Sipping water is especially important when taking medication, for GERD or any other conditions.
Possible questions to ask your doctor
The above actions are a great place to start, but they are general. To get a more customized plan for treatment and to better manage acid reflux attacks, ask your gastroenterologist or GI provider:
- What is the most likely cause of my acid reflux?
- Are there any tests I need to confirm GERD diagnosis or the underlying cause?
- Is my acid reflux acute or chronic?
- What are my treatment options?
- Should I follow any lifestyle or dietary restrictions?
These questions work for most patients, but you can brainstorm additional questions specific to you. If, for example, you also have another GI condition, like Crohn’s disease, and are curious about managing it alongside your GERD, that would be a topic to bring up with your GI provider or gastroenterologist.
Final thoughts
Whether you’re experiencing temporary acid reflux or GERD, it’s important to remember you’re not alone and there are multiple treatment options. Often, the best approach to GERD and acid reflux is a combination of medications and lifestyle modifications.
That combination, however, looks different for everyone. To discover the best treatment plan for you, work with a team of GI specialists, such as those at Oshi Health. Oshi’s team have helped patients like you manage GERD symptoms and reduce the frequency of acid reflux flare-ups. Schedule an appointment with an Oshi GI specialist today.
Frequently asked questions (FAQs)
-
There isn’t a single “cure” to GERD. You can’t get a vaccine or take a pill to get rid of this condition. GERD can, however, be managed and possibly cured with a comprehensive treatment plan that includes medication and lifestyle modifications.
-
Making acid reflux go away often requires a multi-pronged approach. It often starts by going to a GI specialist, such as a gastroenterologist, who can assess any underlying causes and prescribe any necessary medications. Alongside medications, lifestyle changes, such as avoiding trigger foods or quitting smoking, can impact GERD.
-
Acid reflux and GERD are related, but not the same. Acid reflux refers to the process where the stomach’s contents, including stomach acid, return to the upper part of the GI tract, causing heartburn and/or other uncomfortable symptoms. If acid reflux occurs two or more times a week, a clinician may diagnose you with GERD.
-
A GERD episode is often treated with over-the-counter or prescription medications and lifestyle modifications, such as changing into loose fitting clothing and not lying down after eating. More long-term adjustments are often required to manage GERD, such as making dietary changes and developing better eating habits.
-
The most common symptoms of GERD are heartburn, or a burning sensation in the chest, and regurgitation, when the stomach’s contents head back up the GI tract. Six other common symptoms include nausea, a bad taste in the mouth, chest pain, dry mouth, pain in the throat, and gum irritation.
-
GERD is a common condition in babies. It often manifests as spit up, which over half of all babies do during their first three months. GERD in babies, however, often goes away quickly, with few children experiencing symptoms after their first birthday. If a baby does have GERD, seek out a pediatric gastroenterologist as GI providers like Oshi Health do not treat children.
Oshi is your partner in digestive health
Feel like your digestive concerns are running your life? You’re not alone—and we’re here to help you find lasting relief.
Oshi Health GI providers, gut-brain specialists, and registered dietitians work together to address your symptoms and find solutions that actually work for you.
Whether you’re dealing with chronic digestive issues or unpredictable symptom flare-ups, our GI specialists deliver:
✔ Personalized care plans tailored to your lifestyle
✔ Science-backed strategies to calm your gut
✔ Compassionate, whole-person care
✔ And so much more!
Ready to take control of your gut health?