IBS Overview
IBS Overview
Irritable bowel syndrome (IBS) is a chronic gut health condition that affects the function of the gastrointestinal (GI) tract, causing uncomfortable abdominal symptoms that can interfere with daily living.
In people with IBS, the muscles in the colon or small intestine are highly sensitive to normal gut functions, like contractions and gas.
Read on to learn about IBS symptoms, causes, risk factors, and complications—and how we can help you find relief!
IBS symptoms
Wondering if your symptoms might be IBS or looking to better understand your condition? Let’s explore some of the signs of irritable bowel syndrome (IBS) and get you the answers you need, whether you’re newly concerned or already have a diagnosis.
IBS symptoms can vary from person to person, but they have one thing in common: they’re uncomfortable and sometimes painful.
Common symptoms of IBS include:
- Abdominal cramping or pain, often related to having a bowel movement
- Excess gas and bloating
- Diarrhea, constipation, or both
- Mucus covering your poop
- Urgent need to have a bowel movement
- A feeling of still having to go after pooping
Depending on your main symptoms, you may fall into one of four IBS types:
- IBS with constipation (IBS-C). People with this type of IBS have:
- Infrequent bowel movements
- Trouble passing bowel movements without straining
- Hard or lumpy stool
- A sensation of not passing all your stool
- IBS with diarrhea (IBS-D). People with this type of IBS have:
- Mostly loose stools
- Frequent bowel movements
- A regular urgent need to poop
- IBS with mixed bowel habits (IBS-M). People with this type of IBS alternate between having hard and loose stools.
- IBS unclassified. People with this type of IBS have symptoms but don’t neatly fit into any of the categories above.
Living with IBS symptoms can be challenging, but it’s important to know that you’re not alone. In fact, estimates suggest about 6% of U.S. adults live with IBS.
At Oshi Health, our GI specialists, including GI providers, registered dietitians, and gut-brain specialists, work together to address your IBS symptoms.
IBS causes
There’s no exact known cause for IBS, but we know that people with the condition have more sensitive digestive tracts (particularly the colon and small intestine) than those without IBS.
Muscle contractions and gas production are normal digestive functions that can lead to symptoms in people with IBS-related hypersensitivity.
You can also develop IBS after a bacterial or viral infection. And there’s a link between IBS and small intestinal bacterial overgrowth (SIBO).
Additionally, evidence suggests the following may be potential triggers for IBS symptoms:
- Eating certain foods. Most people don’t have to visit the bathroom right after eating. If you have IBS, the urge to go might come sooner or immediately after finishing a meal, especially one containing fat, FODMAPs, or dairy products with lactose.
- Hormone changes. Hormone changes that happen during menstruation, perimenopause, and menopause can increase IBS symptoms. This can make an already uncomfortable time of the month or period of life more difficult for some.
- Stress. Hello, gut-brain connection! Because your nervous system is partially responsible for digestion, high stress levels can trigger spasms in your GI tract, causing or worsening IBS symptoms—and vice-versa.
IBS risk factors
Just because you have a risk factor doesn’t mean you’re destined to get IBS, but it can mean you’re more likely to develop the condition than someone else.
IBS risk factors include:
- Being under 45
- Being female
- Having a recent bout of viral or bacterial gastroenteritis, aka the stomach flu
- Having a family history of IBS
Researchers have also identified a link between stress in early life and an increase in IBS symptoms.
IBS complications
Unlike inflammatory bowel diseases like Crohn’s disease or ulcerative colitis, IBS doesn’t damage the GI tract over time. But it can still seriously affect your quality of life.
You might struggle to feel comfortable in social situations because you’re worried about being near a bathroom, or you might have trouble focusing at work because you need to use the bathroom so often. Painful symptoms like cramping and bloating can also make it challenging to get quality sleep.
All of these can take a toll on your mental health and emotional well-being—which is why a gut-brain specialist can be an important resource.
Additionally, the straining that affects some people with frequent bouts of constipation can lead to or worsen hemorrhoids.
IBS diagnosis
The first step toward an IBS diagnosis is a thorough medical history. At Oshi Health, our GI specialists consider the whole you when working together to make a diagnosis, including your medical history, symptoms, and lifestyle.
Your provider will ask you questions about your symptoms, like when and how often they typically occur or whether certain foods or behaviors tend to make them worse.
They’ll also consider the following:
- Your diet and potential trigger foods
- Lifestyle habits
- Any medications or supplements you’re taking or have tried for your symptoms
- Stress and behavioral health
- Previous surgeries or medical procedures
- Your family history

Let’s talk about poop
It might feel embarrassing at first, but it can help to share the following details about your poop and bathroom habits with your provider:
- How often you poop
- What your poop looks like
- Whether the consistency of your bowel movements changes from week to week or has changed over time
- Whether going to the bathroom helps improve symptoms like abdominal cramping or bloating
And while you don’t need to have had previous testing to meet with an Oshi provider and benefit from our integrated GI care, your provider will review any previous testing you’ve gone through, if any.
They may also recommend additional testing if you have a combination of risk factors or serious symptoms like:
- Blood in your stool
- New onset symptoms over 50
- Unexplained weight loss
- Diarrhea at night
- Fever
- Iron deficiency anemia
- Family history of colorectal cancer, inflammatory bowel disease (IBD), or celiac disease
There’s a myth that IBS is a diagnosis of exclusion, but that couldn’t be further from the truth. Healthcare professionals use a specific set of guidelines to diagnose IBS based on your symptoms and their patterns—to more quickly reach a diagnosis and get you on the path to relief.
While testing may be required to rule out other conditions, we do our best to listen and avoid putting you through unnecessary and repeat testing—diagnosing and addressing symptoms based on our detailed knowledge of the whole you.
In-network with most major health plans
Unlike traditional healthcare providers, we don’t bill on a per visit basis. With insurance coverage, most Oshi Health patients get a year of unlimited care and only pay for four in-network specialist visits. For those four visits, copays and deductibles apply based on your plan benefit details

IBS treatment
We take a comprehensive approach to IBS treatment, addressing not just your symptoms but also putting you on a path to better digestive health. Here’s an example of what treatment can look like when IBS symptoms overlap with other digestive concerns, and how our team works together to provide comprehensive, personalized care.
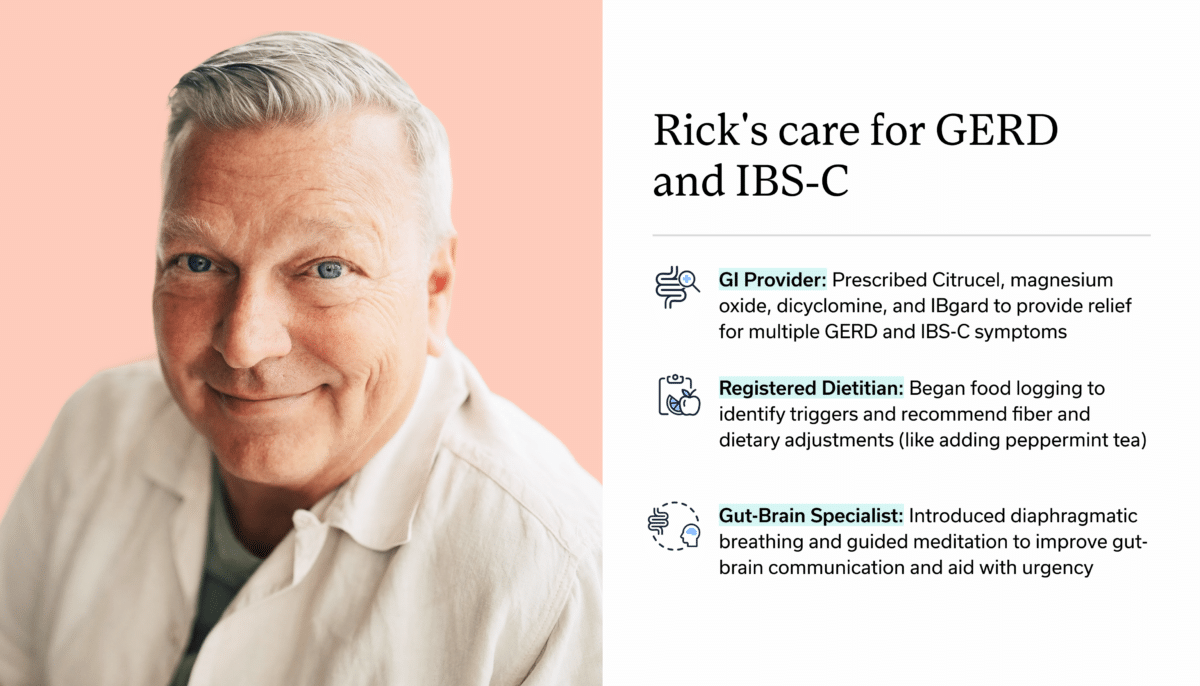
Here’s what that treatment entails:
1. Identifying triggers & making dietary and lifestyle adjustments
What does your typical diet look like? Do you have dietary triggers that seem to make your IBS symptoms worse?
Our registered dietitians will help you identify your IBS-trigger foods and find ways to modify your diet without necessarily giving up the foods you love.
This might involve:
- Increasing or decreasing your fiber intake, or modifying the types of fiber in your diet, depending on your symptoms
- Eating smaller, more frequent meals
- Identifying high FODMAPs in your diet and whether they’re a trigger for your symptoms
Additional lifestyle habits that may help with symptom relief include:
- Improving Sleep hygiene refers to habits that help promote quality sleep like creating a comfortable bedroom environment and reducing screen use before bed.
- Regular physical activity
- Improving your toilet posture and positioning
2. Working on the gut-brain connection
Did you know your brain and digestive system are in constant communication? It’s why you might feel butterflies in your stomach when you experience heightened emotions like stress or excitement.
The close link between your gut and mind can also play a role in conditions like IBS. In fact, many people report that their IBS started during a period of high stress.
Living with chronic IBS symptoms can be incredibly stressful. Stress can actually make your symptoms worse, creating a vicious cycle where stress and GI discomfort feed off each other.
Our gut-brain specialists can help you identify potential stress-related IBS triggers.
Gut-brain specialists are trained and licensed behavioral health professionals with specific experience treating GI concerns like IBS. Working alongside GI providers and registered dietitians, they can help you take control of your symptoms by providing you with the skills and tools to cope with distressing thoughts, feelings, and physical reactions that may be contributing to GI distress.
This might include:
- Diaphragmatic breathing exercises
- Progressive muscle relaxation (PMR)
- Mindfulness-based therapies
- Cognitive behavioral therapy (CBT) for GI symptoms
- Gut-directed hypnotherapy (GDH)
Oshi Health gut-brain specialists are here to support you as you navigate living with a chronic digestive health condition, helping to normalize and validate your GI-related concerns—so you never feel alone in your journey to symptom relief.
3. Prescribing or recommending medications
Medications are just one piece of the journey to symptom relief. Our whole-person approach to GI care looks at lifestyle factors such as diet and stress that may be contributing to symptom flares. Depending on your unique needs, medications may be a part of your personalized treatment plan.
Your provider may recommend or prescribe the following to help with constipation, diarrhea, or abdominal pain:
- Fiber supplements like psyllium fiber
- Magnesium oxide to help treat constipation
- Miralax to help soften stool
- Peppermint oil capsules for relief from gas, bloating, and abdominal pain
- Prescription medications such as:
- Loperamide
- Antispasmodics
- Bile acid binders
- Tricyclic antidepressants
- And others based on your unique needs
4. Whole-person care for IBS
At Oshi Health, no two treatment plans are the same.
Our GI specialists work together to create a personalized treatment plan to address your symptoms. We consider the whole you—not just your IBS. That means taking into account diet, lifestyle, and the gut-brain connection, ensuring you get the individualized care you need.
Already seeing a GI provider? We can provide support between visits and work with your existing gastroenterologist as an extension of your care.
- decrease in unnecessary (and expensive) procedures and tests
- of undiagnosed patients get a clear diagnosis within 3 months
- of patients report better quality of life, with less stress and anxiety, within 3 months
Source: Results of a clinical trial conducted in partnership with a national health plan
Oshi is your partner in digestive health
Feel like your digestive concerns are running your life? You’re not alone—and we’re here to help you find lasting relief.
Oshi Health GI providers, gut-brain specialists, and registered dietitians work together to address the root cause of your symptoms and find solutions that actually work for you.
Whether you’re dealing with chronic digestive issues or unpredictable symptom flare-ups, our GI specialists deliver:
✔ Personalized care plans tailored to your lifestyle
✔ Science-backed strategies to calm your gut
✔ Compassionate, whole-person care
✔ And so much more!
Ready to take control of your gut health?
Frequently Asked Questions
-
Living with IBS can be unpredictable, with periods where you’re feeling fine and periods where you have to rush to the bathroom. When something triggers symptoms, you might experience bloating, excess gas, abdominal pain, and changes to your bowel movements—all of which can seriously impact your quality of life.
-
Irritable bowel syndrome (IBS) is a condition that affects intestinal function. In someone with IBS, the intestines are hyper-sensitive, responding atypically to normal gut functions and causing symptoms like pain and discomfort.
Inflammatory bowel disease (IBD) refers to two GI conditions—Crohn’s disease and ulcerative colitis—involving visible inflammation of the intestines.
-
Common IBS trigger foods include:
- High-fat foods like fried foods
- Common high FODMAP foods like apples, garlic, onion, wheat, and dairy
- Very high fiber foods
- Caffeine
- Chocolate
Your IBS trigger foods might not be the same as someone else’s. That’s why it can help to work with a registered dietitian to identify foods that make your symptoms worse and find a diet that works for you.
-
For most people, IBS is a lifelong digestive health condition. While there’s no cure, it’s possible to reduce or eliminate IBS symptoms altogether with a combination of diet modifications, medications, and gut-brain interventions.
Last medically reviewed October 2025