Key takeaway: Winter viruses don’t just affect your respiratory system—they can stress your gut, too. Understanding the gut-germ connection can help you support your digestive system and better manage symptom flares.
If you live with chronic or occasional gastrointestinal (GI) symptoms, cold and flu season can feel more precarious than it does for others. Many people with digestive concerns notice their symptoms flare up during or after respiratory viruses—more bloating, diarrhea, constipation, and reflux than usual. That’s because, like your sniffly nose, your gut responds to illness, too.
How gut health and immunity are connected
Much of your immune system lives in or communicates via your gut. When a virus enters your system, this can trigger whole-body inflammation and nervous system changes that can:
- Disrupt digestion
- Increase gut sensitivity
- Mess with your appetite
- Worsen fatigue
“Viral stomach infections can temporarily change how your digestive system works. This happens because the virus can irritate the gut, cause ongoing inflammation, and disrupt the normal balance of bacteria in your intestines. For most people, these changes improve within 3 to 6 months, but a small number may continue to have symptoms longer,” says Oshi GI provider Sarah O’Rourke.
A chronic GI condition can also put you at higher risk of catching viruses. Patients with IBS-D (IBS where diarrhea is a primary symptom) are often low in vitamin D, says Oshi GI provider Robbie Leinart, which can lower their immunity.
Living with a GI condition during cold and flu season
If you’re already living with a reactive digestive system—hello, irritable bowel syndrome (IBS)—you’re more likely to experience stronger reactions during illness.
For those with inflammatory bowel disease (IBD), getting sick with a virus can come with extra worry, especially if you take immunosuppressive medications that affect your immune system and may make recovery more complicated.
And if you live with gastroesophageal reflux disease (GERD), coughing, congestion, inflammation, and over-the-counter meds can worsen reflux symptoms.
When to call a GI provider
- You have GI symptoms that are more severe than your usual baseline
- Your GI symptoms don’t go away
- You experience new GI symptoms
- You have diarrhea that lasts more than 2 days
- You have a fever of 101 or more, and you have blood in your stool or vomit, or worsening abdominal pain
- You're immunocompromised (it's a good idea to check in with your provider, even if you're feeling fine)
- You’re feeling worried and looking for some peace of mind
How to support your gut during illness
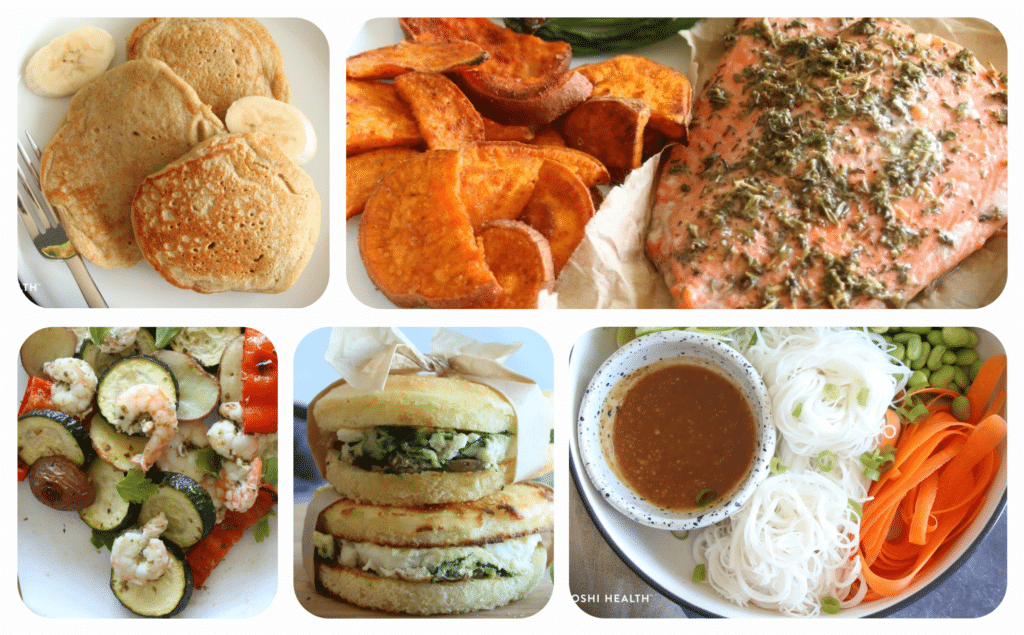
Gentle nourishment
It can be hard to stomach your usual diet when you’re feeling under the weather. So opt for foods that are gentle on your digestive tract and that you find palatable, versus stressing over nutrition.
“A soothing, nutrient-packed bowl of soup or a smoothie is a great choice. Prioritizing well-cooked or blended foods can provide nourishment while being gentle on your digestive system,” says Adrienne Dowd, Oshi registered dietitian.
Provider tip: Prioritize fiber when possible. “We know that fiber helps promote good quality bowel movements. It also helps to feed that good bacteria that support your immune system.” — Robbie Leinart, Oshi Health GI Provider.
Hydrate, hydrate, hydrate
Don’t forget to hydrate! Your body needs fluids to recover, and dehydration can worsen GI symptoms like constipation and diarrhea. Dowd recommends aiming for 64 ounces of fluid each day. You can sip on water or keep a warm cup of herbal tea or bone broth handy.
Provider tip: “A good idea is to keep a pitcher of water next to the bed and have a thermos filled with a hot beverage so that refills are easy and accessible. When we do not drink enough fluids, the fiber we eat will not be hydrated, and that can cause bowel movements to be hard and difficult to pass.” — Beth Rosen, Oshi Registered Dietitian.
Stress check
Winter illness often goes hand in hand with higher stress and disrupted routines. That’s because stress amplifies gut sensitivity and can make it harder for your body to recover when it does get hit by germs. (Read more about the gut-brain connection here).
The number one thing you can do to support your recovery (and your gut)? Rest without trying to push through your symptoms.
Provider tip: Building a stress management toolkit can help you support a healthy immune system and cope with flare-ups if you do get sick. Oshi gut-brain specialist Steve Feinstein recommends diaphragmatic breathing as a good place to start. A consistent guided meditation practice is another way to manage stress levels. “Maybe the easiest is to make about a 10 to 15 minute playlist of your favorite relaxing songs and just set aside some time each day to listen, breathe, and relax to try to settle those flares down,” says Feinstein.
Expert GI care at your fingertips
Because living with a GI condition means needing care beyond a single visit
Takeaway
Cold and flu season can hit differently when you live with a GI condition. But there are ways to help calm flares and make recovery feel more manageable. And you don’t need to go through it alone. Coordinated GI, nutrition, and gut-brain care can help you navigate illness-related flares with more confidence.
Oshi is your partner in ongoing digestive care
GI symptoms don’t wait for your next appointment. Flare-ups and questions can come up between scheduled visits. And we’re here for ongoing support.
Oshi Health gives you access to GI providers, registered dietitians, and gut-brain specialists who work together to help you manage symptoms as they happen and adjust your care as needed.
Whether you’re living with daily digestive discomfort or unpredictable flare-ups, Oshi offers:
✔ Access to an expert care team, including for between-visit support and guidance
✔ Care plans that evolve with you
✔ Evidence-based tools to manage flares, triggers, and setbacks
✔ Compassionate, whole-person care built around your life
You deserve digestive care that meets you where you are.