These days, having a social life often means attending gatherings that involve eating and drinking. When you have inflammatory bowel disease (IBD), participating in these types of social events—like going out to eat—can be anxiety-provoking. But it doesn’t have to be.
“When in a flare state, it can be scary to dine out, but with a bit of prep in advance, the experience can be pleasant,” says Kelly Krikhely MS, RD, CDN, a New York City-based nutritionist specializing in digestive disorders. “The first trip to a new restaurant is usually the hardest. Once you identify items on the menu that you tolerate well, return trips will be much less stressful.”
Next time your friend group wants to go out to eat, it may help to keep these tips in mind.
1. Do your research in advance: Don’t wait until the pressure is on and the server is taking your order to decide what to eat. “Research the menu in advance to come up with a strategy for what you plan to order,” says Krikhely. You can even call ahead if you have specific questions about the menu or how a particular dish is prepared to help you identify “safe” dishes to order before you even arrive at the restaurant.
2. Have a snack before you go: Avoid showing up at the restaurant too hungry, as hunger can cloud your judgment, and lead you to not make smart food choices. “Sometimes I’ll eat a little something before heading out so I am not too hungry and can keep my meal simple when in public,” says Natalie Hayden, who was diagnosed with Crohn’s disease in 2005.
3. Dress for the occasion: “I recommend wearing pants with an elastic waistband or a dress versus wearing jeans or dress pants if you can get away with it,” adds Hayden. “Oftentimes when I’m bloated, restricting my stomach adds to the pain.”
4. Stake out the nearest restroom: “Once you arrive at the restaurant, it can be helpful to check out where the bathrooms are and to sit on the outside of the booth in case you need to make a mad dash,” adds Hayden.
5. Avoid trigger foods: Especially if you’re in a flare, you’ll want to avoid foods that can make symptoms worse. For most people, that means choosing nutritious foods that are easy to digest and have little soluble fiber, like cooked vegetables and fruits, oatmeal, and lean sources of protein like chicken or eggs.
“As a general rule of thumb, try to choose menu items with simple ingredients,” says Krikhely. “A broth-based soup, a simple turkey sandwich, or grilled salmon or chicken with white rice or skinless baked potato are examples of go-to items that are typically well-tolerated.”
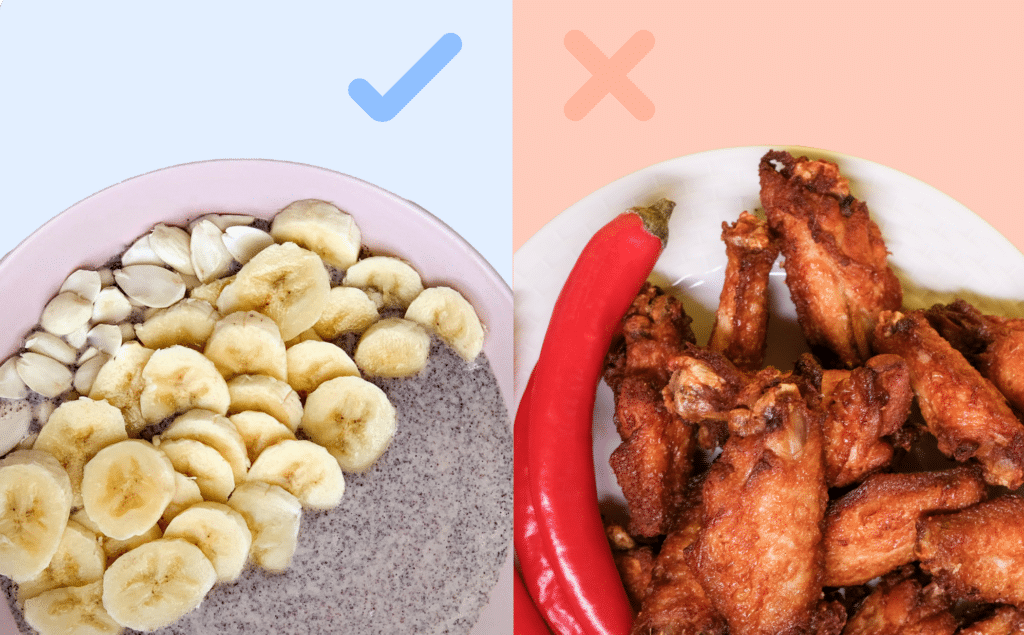
6. Consider how foods are prepared: “It’s usually preferable to limit fried foods when dining out,” says Krikhely. “Key words on the menu that can commonly be considered red flags include fried, creamy, crispy, crunchy, battered, and spicy.” Large quantities of fat or spicy foods are often not well tolerated, she explains—though, she adds, that’s only the case for some IBD patients. You may want to stick to preparation methods that are well-tolerated by people with IBD—like baked, broiled, boiled, steamed, poached, grilled, or sautéed.
7. Make special requests as needed: Many restaurants are happy to accommodate special requests to alter how a dish is prepared—all you need to do is ask. “You can ask the chef to customize your dish to eliminate items you know may be poorly tolerated,” says Krikhely. “You can also ask to adjust the method of preparation, grilled fish instead of fried fish, for example. And because many sauces contain lots of fat and spices that may not be well-tolerated, requesting sauce on the side can be a simple solution.”
8. Consider portion sizes: When you have IBD, portion size can make a difference. “Small, frequent meals are typically better tolerated than large portions,” says Krikhely. “Share your entree with a friend, or eat half the portion and take the rest home to enjoy the next day.” You can also order an appetizer, which is typically a smaller portion than an entrée—just avoid those that are fried.
“I try not to overeat when I dine out,” says Jordan Wilson, who was diagnosed with ulcerative colitis in 2010. “I make sure to keep it light and relatively clean.” By “clean”, Jordan explains, he means meals prepared simply with only a few fresh ingredients.
9. Schedule outings wisely (and reschedule if needed): “Sometimes a heavy lunch or dinner can’t be avoided. If that’s the case, I make sure to keep my afternoon calendar clear of appointments,” says Wilson.
10. Ask your doctor if medication can help: Depending on your specific symptoms, your doctor may recommend anti-diarrheal medications, antispasmodics, or lactase supplements to help you go out to dinner with ease.
Need help identifying what foods to eat and what to avoid? Get access to a personalized team of GI providers, including a GI Registered Dietitian, when you sign up for Oshi Health.
Medically reviewed by Jenny Blair, MD
Oshi is your partner in digestive health
Feel like your digestive concerns are running your life? You’re not alone—and we’re here to help you find lasting relief.
Oshi Health GI providers, gut-brain specialists, and registered dietitians work together to address the root cause of your symptoms and find solutions that actually work for you.
Whether you’re dealing with chronic digestive issues or unpredictable symptom flare-ups, our GI specialists deliver:
✔ Personalized care plans tailored to your lifestyle
✔ Science-backed strategies to calm your gut
✔ Compassionate, whole-person care
✔ And so much more!
Ready to take control of your gut health?