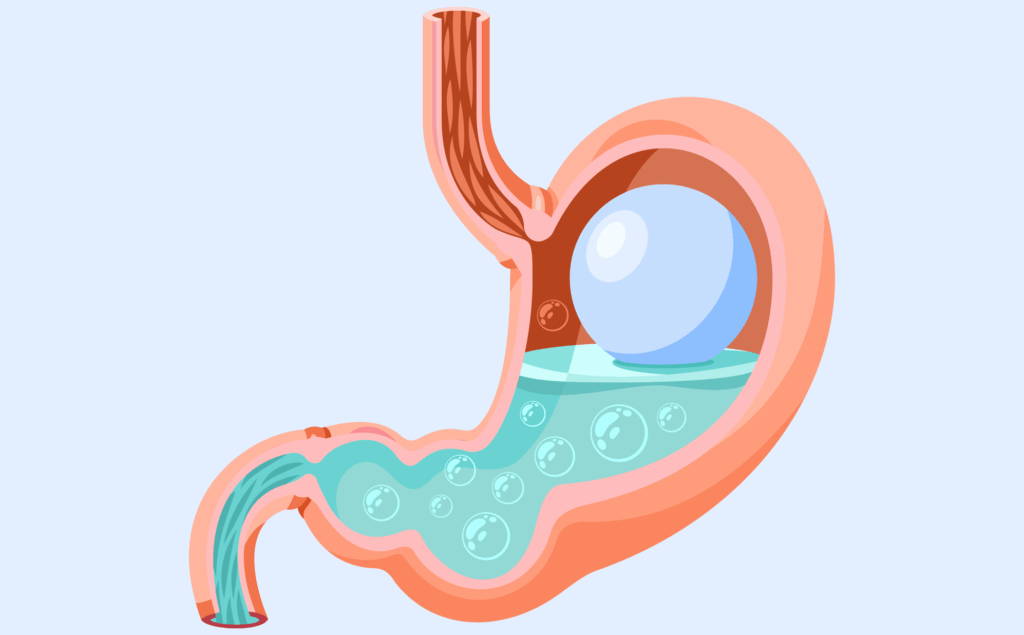
Occasional heartburn is one of the most common GI complaints. But when it progresses beyond occasional and mild to frequent and severe, gastroesophageal reflux disease (GERD) can become a daily misery.
Most of us reach for an over-the-counter antacid (like calcium carbonate) for occasional acid reflux symptoms. But if your symptoms are persistent, and you find yourself using antacids more than twice a week, it’s important to talk to your GI care team about GERD, and to manage the impact of stomach acid on your esophagus. Here are three things they may recommend to avoid triggering GERD symptoms:
1. Eating smaller meals, slowly
Because GERD symptoms occur when food in the stomach and stomach acid are pushed into the esophagus, too much food in your stomach at one time can increase GERD symptoms. Smaller meals, eaten slowly, are easier for your body to digest.
2. Remaining upright after eating
Don’t lie down or recline immediately after eating, which can make it easier for stomach contents to flow to the esophagus, and aggravate GERD symptoms. A good guideline is to avoid lying down within 30 minutes of eating, and avoid eating or drinking large volumes of liquid within two hours of your bedtime.
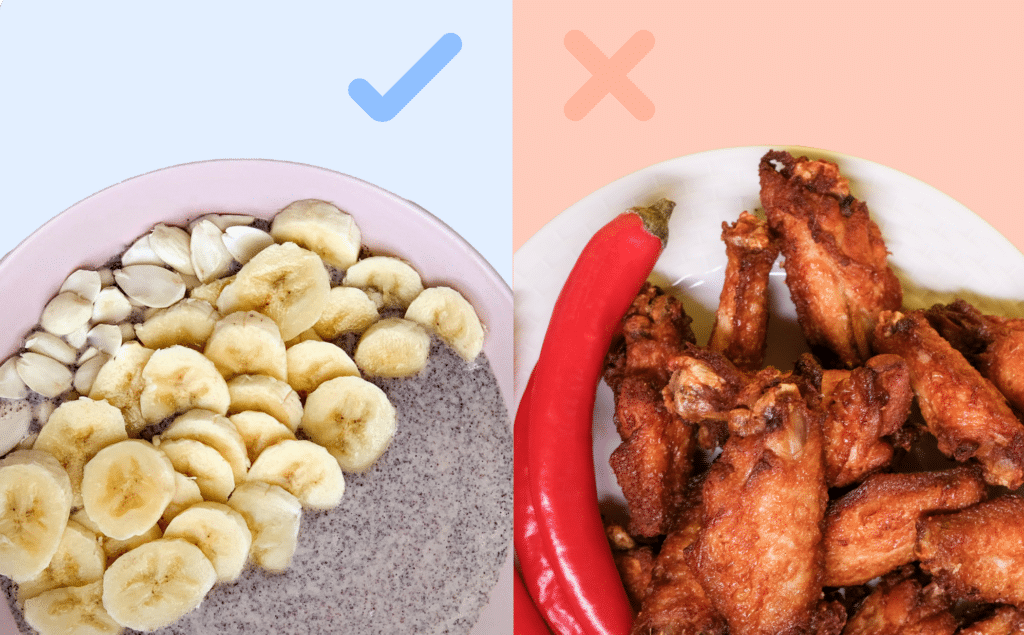
3. Avoiding food triggers
Spicy foods, coffee or strong tea, alcohol, fatty, rich or “heavy” foods, and fried food can irritate the stomach and esophagus, and bring on GERD symptoms. Even “too hot” foods (like soups and teas) can aggravate GERD symptoms. Tracking your food intake with a food diary and working with a GI Registered Dietitian can help you identify the relationship between what you eat and how you feel, and create a sustainable plan to manage any changes. GERD symptoms should not be ignored, because over time, stomach acid can injure the esophagus and lead to narrowing of the esophagus. Fortunately, your GI care team can make personalized recommendations to help diagnose and treat GERD, and improve your overall digestive health.
Oshi is your partner in digestive health
Feel like your digestive concerns are running your life? You’re not alone—and we’re here to help you find lasting relief.
Oshi Health GI providers, gut-brain specialists, and registered dietitians work together to address the root cause of your symptoms and find solutions that actually work for you.
Whether you’re dealing with chronic digestive issues or unpredictable symptom flare-ups, our GI specialists deliver:
✔ Personalized care plans tailored to your lifestyle
✔ Science-backed strategies to calm your gut
✔ Compassionate, whole-person care
✔ And so much more!
Ready to take control of your gut health?