When patient advocate Tina Aswani Omprakash, 35, reached an impasse with symptoms related to her inflammatory bowel disease (IBD), she turned in frustration to her nutritionist. On her nutritionist’s suggestion, Omprakash, who lives in New York City, decided to give the low-FODMAP diet a try.
What are FODMAPs?
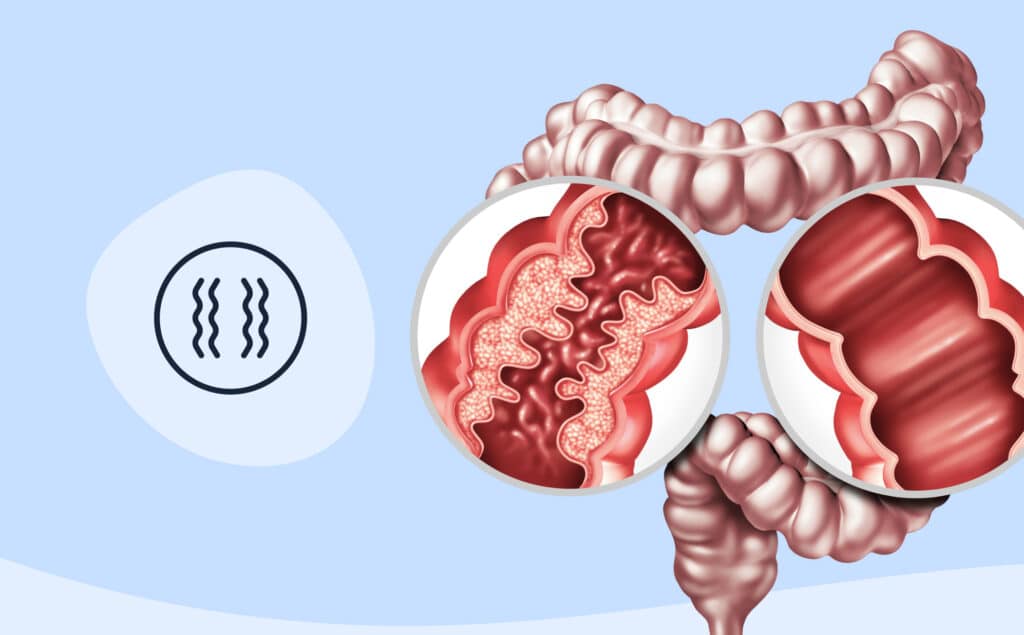
FODMAPs stands for “fermentable oligosaccharides, disaccharides, monosaccharides, and polyols,” all sugars that are common in foods. If these small sugars go unabsorbed and hang around in the intestines long enough, they can produce diarrhea and abdominal bloating and cramping, depending on where they linger. People who have irritable bowel syndrome (IBS) can sometimes find symptom relief through steep reductions in FODMAP intake. The benefits for people with IBD, however, are less clear.
Low FODMAP diet pitfalls
Trying a low FODMAP diet is not for the weak at heart. “It was kind of daunting at first to realize how much I had to cut out,” says Omprakash. In the end, after trying it for a couple of months, she saw some symptom relief, but emphasizes that because of her additional history of many surgeries, IBS, and having no colon, her experience is quite individual. Omprakash does not currently adhere to a strict form of the diet.
The gut is sensitive and highly personal, and so there’s no one-size-fits-all approach to whether people find relief from reducing FODMAPs Kelly Issokson, RD, CNSC, is an IBD Dietitian (clinical nutritionist) affiliated with the Cedars-Sinai Nutrition & Integrative Inflammatory Bowel Disease Program in Los Angeles. She says that for certain IBD subgroups, there may be benefit of the low FODMAP diet. However, this diet is not for everyone.
People with IBD should talk with their health providers before making any significant dietary changes. With that caveat in mind, here are 7 things to know if you’re considering a low FODMAP diet.
1. Benefits vary for people with IBD: One analysis of the collective findings from several studies showed that a low-FODMAP diet can reduce symptoms of nausea, bloating, gas, and diarrhea if IBD is inactive, says Issokson. Patients without active inflammation seem to gain the most benefit, she says, noting that patients with constipation usually see the least benefit.
2. It can be a hard diet to follow: Omprakash calls it “daunting,” and Issokson says one of the toughest parts is having to avoid onions and garlic, which, as she notes, “seem to be in nearly every food!”
3. It doesn’t put the brakes on active IBD or reduce IBD activity: Issokson says evidence to date shows no benefit of low FODMAP in these cases, and that constipation can even worsen for some people.
4. It’s a good idea to focus on fiber sources: Because the diet might exacerbate constipation in some people, attention to fiber is crucial, says Issokson, ticking off some examples to consider including: green bananas (ripe bananas are high in FODMAPs), cooked carrots, nut butters, chia seed, and kiwi.
5. It’s not a long-term commitment: The diet can trigger unwanted decreases in gut bacteria diversity, so it’s not a long-term diet to follow, says Issokson. In addition, because it’s so restrictive, it can affect of quality of life. On the physical front, low calcium intake is another risk.
6. You should work with a registered dietitian who specializes in GI conditions: Doing so is important to ensure an appropriate and nutritionally sound approach to the diet, says Issokson, who urges a consult with a clinician before any big dietary changes.
7. You can individualize it: For example, patients with IBD may not need to follow a complete low-FODMAP diet and can gain symptom improvement by reducing only fructans (commonly found in wheat and onion), says Issokson. A GI Registered Dietitian can help you identify your food triggers and work to avoid them.
Medically reviewed by Matthew Hamilton, MD
Oshi is your partner in digestive health
Feel like your digestive concerns are running your life? You’re not alone—and we’re here to help you find lasting relief.
Oshi Health GI providers, gut-brain specialists, and registered dietitians work together to address the root cause of your symptoms and find solutions that actually work for you.
Whether you’re dealing with chronic digestive issues or unpredictable symptom flare-ups, our GI specialists deliver:
✔ Personalized care plans tailored to your lifestyle
✔ Science-backed strategies to calm your gut
✔ Compassionate, whole-person care
✔ And so much more!
Ready to take control of your gut health?