Poop appearance can provide insight into what’s going on in your body. So it can be unnerving to see an unusual change in what you leave in the loo. You might be wondering, “Why is my poop bubbling in the toilet?” or “Why do I have foamy diarrhea?” We’ve got answers.
We get it. Poop can be an uncomfortable topic. But pooping is a bodily function, and occasionally what you see in your toilet might send your eyebrows up in alarm. Anyone who has ever eaten beets and then gone number two, for example, has likely experienced this moment of temporary concern when their stool appears pink or red.
Poop appearance can change from day to day and even throughout a day if you go more than once. Many changes are completely normal, while others might signal a concern, especially if they persist.
Of course, when you start searching the internet for information on the topic, you might encounter poop jokes or lists of alarming potential causes. We’re here to cut through that noise and give you the straight facts. Ultimately, if you notice persistent changes, especially with other symptoms, talking to a knowledgeable provider is always a good idea.
Let’s get right to it and unpack reasons why your stool might change in appearance–including looking bubbly or foamy–when to see a doctor, and more.
Why is my poop bubbling in the toilet?
After a number two, you might see bubbles in the toilet. Don’t panic! The first things to consider are actually not related to poop. Bubbles in stool might occur from toilet cleaners if the loo you’re using has recently been refreshed.
Likewise–without getting too into the nitty-gritty of plumbing–sometimes flushing and other mechanisms can cause bubbles in the toilet. And let’s not forget that sometimes when we go number two, we also go number one, and urine can occasionally have a bubbly or foamy appearance.
If you’ve eliminated the above as the source, the following are some poo-related causes of bubbles.
-
Gas release: Sometimes gas from your intestines will show up in your stool, leading to a little toilet bubbling. Factors that can cause gas include eating too fast, chewing gum, drinking carbonated beverages, drinking through a straw, and more. Additionally, bacteria in the gut ferments portions of the foods you eat.
-
Mucus in stool: Your intestines have a mucus layer that serves as protection from toxins and pathogens, and you might sometimes notice that you pass a little mucus as a normal part of gut function. Intestinal mucus can appear bubbly or foamy, just like spit from your mouth or snot from your nose can. Having a little mucus in your stool is normal. Excessive mucus, however, might indicate a food intolerance or sensitivity, a gastrointestinal infection, nutrient absorption issues, irritable bowel syndrome (IBS), or inflammatory bowel disease (IBD). Sometimes, GI infections can cause increased mucus production.
When you’re searching the internet to find a reason for your symptoms, you might come across links to various gastrointestinal (GI) conditions, such as those noted above, and understandably you might grow a little anxious.
Generally, occasional bubbles in poop are completely normal. If you notice this presentation frequently, however, never hesitate to talk through your symptoms with a knowledgeable GI specialist.
Foamy stool and foamy diarrhea: common causes
Foamy poop or foamy diarrhea can also show up in the bowl. Again, leftover cleaning agents might foam up when your stool hits the water, and toilet water might be a little more effervescent or foamy from various plumbing mechanisms. Plus, as noted above, urine can sometimes appear foamy if you’ve killed two birds with one stone by going number one along with number two.
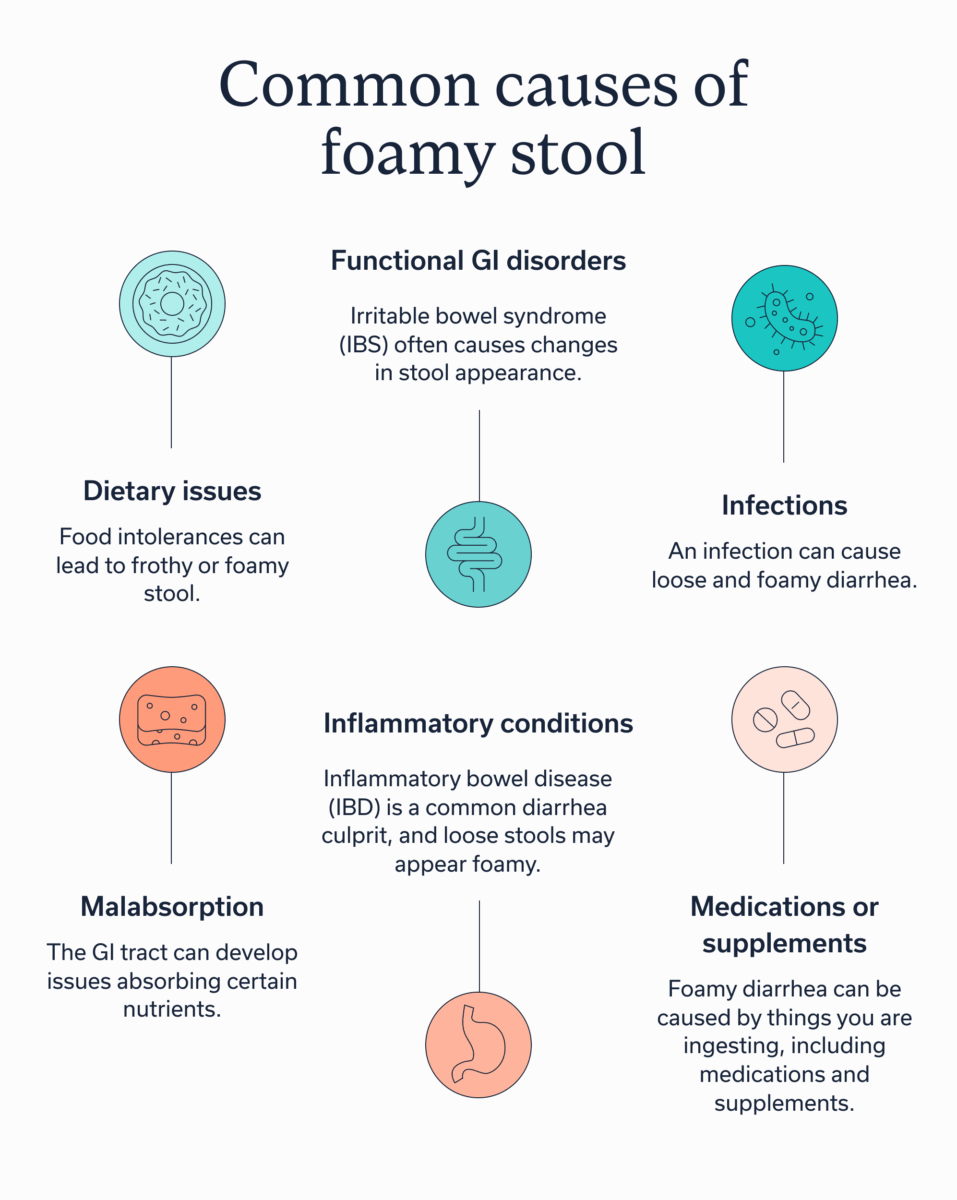
Here are a few common causes of foamy poo:
-
Dietary issues: Food intolerances (e.g., lactose, histamine, FODMAPs, etc.) can lead to frothy or foamy stool.
-
Functional GI disorders: Irritable Bowel Syndrome (IBS) is one of the most common Disorders of Gut-Brain Interaction (DGBI), which are a group of conditions that arise from a disconnect in communication between your gut and your brain. IBS often causes changes in stool appearance.
-
Infections: An infection can cause loose and foamy diarrhea. One consideration is giardiasis, which presents with greasy or smelly poo. Others include various GI infections from foodborne or waterborne illness, sometimes resulting from travel or other exposures.Keep in mind that common illnesses, such as the flu, might lead to a temporary change in how your stool looks.
-
Malabsorption: The GI tract can develop issues absorbing certain nutrients. This may occur if you have celiac disease, bile acid malabsorption , or exocrine pancreatic insufficiency. Malabsorption issues can also occur if you’ve had your gallbladder removed.
-
Inflammatory conditions: Inflammatory Bowel Disease (IBD), including Crohn’s and ulcerative colitis, is also a common diarrhea culprit, and loose stools may appear foamy.
-
Medications or supplements: Foamy diarrhea may also have little to do with your gut and more to do with things you are ingesting, including medications and supplements. Orlistat, a lipase inhibitor, prevents the breakdown and absorption of dietary fat, which may cause greasy stools that foam. Magnesium, a mineral and electrolyte, draws water into the gut to help produce a bowel movement. The softer and looser stool may be foamy. And metformin, a common medication to treat prediabetes and type 2 diabetes, can also cause diarrhea.
Types of poop: what they mean
Maybe your stool isn’t foamy or bubbly, but the appearance still surprises you, or is more frequently straying from your norm. Or maybe you’re getting ready to talk to a clinician and you want to know how to describe your poo. When evaluating and categorizing your poop, it can be helpful to consider whethe r it sinks or floats, its form (shape, size, and consistency), and its color.
Floating vs. sinking
Stool might float if it contains gas or excess fat (steatorrhea), making it harder to flush. This can be normal. However, if it frequently occurs or you have additional symptoms, talking to a provider can help you get to the root cause, including malabsorption issues. Sometimes IBS can lead to floating stools as well.
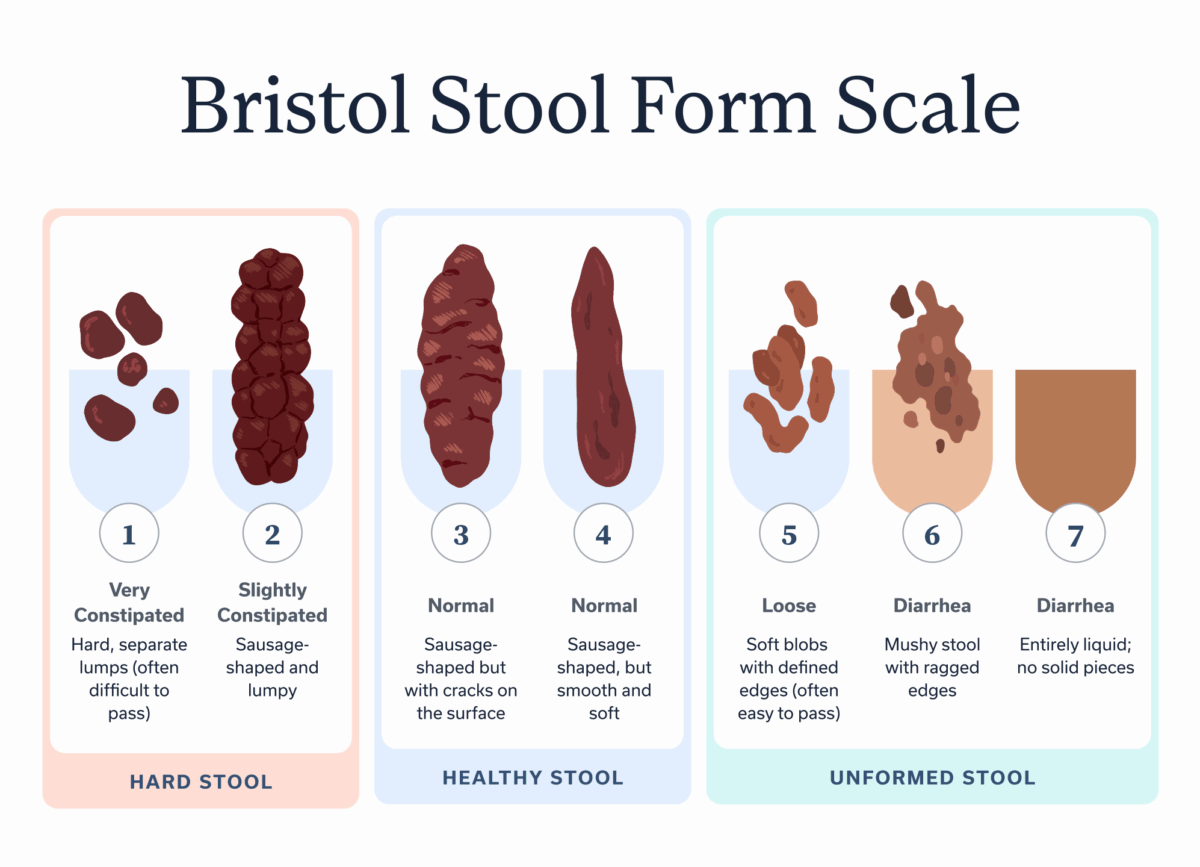
Bristol Stool Form Scale
This chart is a tool that’s widely used by GI providers to help get to the bottom of symptoms. It lists seven types of stool shapes, sizes, and consistencies and correlates them with constipation, diarrhea, inflammation, and more. It’s a great place to start to understand your number twos. The shade of your poop can also provide clues.
Color |
Possible causes |
| Pale or clay-colored |
|
| Yellow or orange |
|
| Green |
|
| Red |
|
| Black or tar-like |
Self-check: questions that help narrow the cause
If the above charts don’t help you narrow down what’s up with your poo, you might wish to ask yourself a few questions to help understand what’s going on with changes to your stool. Your answers might point to the most likely cause. For example, if you were traveling, the change might be related to a disruption in your routine. Having answers to these questions ready to discuss with a GI provider can also be helpful.
Timing:
-
When did the stool change first occur?
-
Was it after eating specific foods?
-
Was it in relation to travel?
-
How often are you noticing the issue?
Associated symptoms:
-
Are you experiencing any other GI symptoms, such as constipation, diarrhea, abdominal, pain, etc.?
-
Are you experiencing any other health symptoms, such as fever, rashes, or joint pain?
Appearance:
-
What is the consistency and shape of your stool?
-
Does your stool have an unusual smell?
-
What color is your stool?
-
Does your stool float or sink?
-
Would you use any other terms to describe your stool?
Medications, supplements, and lifestyle:
-
Have you started a new medication?
-
Have you started a new supplement?
-
Have you changed your diet in any way?
-
Are you experiencing an uptick in stress, anxiety, or other mental health concerns?
When to seek care: red flags
If your bowel changes persist or reoccur, you should talk to a provider, especially if they are affecting your quality of life, such as with persistent diarrhea, or you are experiencing additional unpleasant symptoms. Likewise you should talk to a clinician if you are experiencing any of the following red flags.
-
Blood in your stool or urine
-
Black or tarry stool
-
Persistent pale stool
-
Fever (especially over 102 degrees Fahrenheit)
-
Persistent nausea, vomiting, or diarrhea
-
Persistent or severe pain
-
Excessive mucus in your stool
-
Sudden changes in appetite
-
Dehydration from ongoing diarrhea
-
Sudden changes in bowel habits
-
Unintended weight loss
-
You are pregnant and suspect an infection or food poisoning
Potential treatments for your poop problems
The best treatments to address changes in your bowel habits will depend on the underlying cause. That’s why consulting a healthcare provider is always a good place to start.
Options for resolving your symptoms may include changing your diet, making additional lifestyle changes, or taking medications or supplements if needed. A GI care team can help you decide the best options for you to get you back to feeling better. Here are a few treatments they may recommend.
Dietary modifications
If a food intolerance or malabsorption is the culprit of your bowel changes, then changing your diet may be necessary. But diets for managing these issues don’t need to be restrictive. A GI registered dietitian can work with you to create a plan that aligns with your tastes and nutritional needs.
Lifestyle adjustments
Depending on the underlying reason for the changes in your bowel habits or stool appearance, lifestyle changes may also be beneficial. For example, if stress or anxiety are leading to persistent diarrhea, then working with a gut-brain specialist can help you address communication disruptions that are behind your symptoms.
Medication and supplements
In some cases, you may need medications or supplements, especially if you have an infection or an underlying condition. Again, working with a care team is best to determine what’s right for you. Options may include anti-diarrheal agents, antibiotics, other prescription medications, or evidence-based supplements to support GI health.
Key takeaways
-
Poop sometimes changes appearance from your usual presentation. These occasional changes can be completely normal.
-
Poop may appear bubbly or foamy from mixing with urine or cleaning agents in the toilet, but sometimes these issues indicate an underlying issue.
-
If changes in color, shape, and consistency persist, talking to a knowledgeable GI provider, such as those at Oshi Health to get to the root cause and find solutions if needed.
FAQ
-
In some cases, it can be normal for poop to bubble in the toilet. Common causes include passing trapped gas along with stool, passing mucus with stool, cleaning agents left in the toilet, plumbing mechanisms, and urine mixing with feces. However, if you frequently have bubbling stool and this is a change from your normal experience, consider talking to a clinician about your concerns.
-
Stress can cause a temporary change in poop appearance, but the changes vary widely. You might experience loose or water stool, small or hard pellets from constipation, greenish stool that has rapidly moved through your digestive system, and mucus in your feces.
-
If your bowels are bubbling, that usually means you have trapped gas within the GI tract. Gentle movements can help you release this trapped air or encourage a bowel movement that alleviates some of your discomfort. If you frequently have bubbling bowels, talking to a provider is a good idea to address any potential underlying causes.
-
Gastroesophageal disease (GERD) generally doesn’t change the appearance of your stool directly. However, if you are taking medications for GERD, these can lead to constipation (especially Tums) or diarrhea. If you experience black or tarry stool that is not after Bismuth subsalicylate use, however, that could be an indication of a GI bleed caused by complications from GERD. Seek an evaluation as soon as possible.
-
Poop can change appearance from one day to the next based on diet, stress level, and other factors. Healthy poop is generally brown or light brown and sausage-shaped, with either smooth edges or with cracks on the surface. However, you might notice the occasional smaller lumps or pellets if you’re trending toward temporary constipation, or you might have softer lumps if you’re trending toward temporary diarrhea. Again, these changes can be completely normal on occasion.
Oshi is your partner in digestive health
Feel like your digestive concerns are running your life? You’re not alone—and we’re here to help you find lasting relief.
Oshi Health GI providers, gut-brain specialists, and registered dietitians work together to address the root cause of your symptoms and find solutions that actually work for you.
Whether you’re dealing with chronic digestive issues or unpredictable symptom flare-ups, our GI specialists deliver:
✔ Personalized care plans tailored to your lifestyle
✔ Science-backed strategies to calm your gut
✔ Compassionate, whole-person care
✔ And so much more!
Ready to take control of your gut health?